Abstract
Purpose
This study’s purpose was to investigate how an ideal anatomic femoral attachment affects the dynamic length change pattern of a virtual medial patellofemoral ligament (MPFL) from an extended to a highly flexed knee position; to determine the relative length and length change pattern of a surgically reconstructed MPFL; and to correlate femoral attachment positioning, length change pattern, and relative graft length with the clinical outcome.
Methods
Twenty-four knees with isolated nonanatomic MPFL reconstruction were analysed by three-dimensional computed tomography at 0°, 30°, 60°, 90°, and 120° of knee flexion. The lengths of the MPFL graft and a virtual anatomic MPFL were measured. The pattern of length change was considered isometric if the length distance changed <5 mm through the entire dynamic range of motion.
Results
Knee flexion significantly affected the path lengths between the femoral and patellar attachments. The length of the anatomic virtual MPFL decreased significantly from 60° to 120°. Its maximal length was 56.4 ± 6.8 mm at 30°. It was isometric between 0° and 60°. The length of the nonanatomic MPFL with a satisfactory clinical result decreased during flexion from 0° to 120°. Its maximal length was 51.6 ± 4.6 mm at 0° of knee flexion. The lengths measured at 0° and 30° were isometric and statistically greater than the lengths measured at higher flexion degrees. The failed nonanatomic MPFL reconstructions were isometric throughout the dynamic range, being significantly shorter (27.1 ± 13.3 %) than anatomic ligaments.
Conclusion
The femoral attachment point significantly influences the relative length and the dynamic length change of the grafts during knee flexion–extension and graft isometry. Moreover, it influences the long-term outcome of the MPFL reconstructive surgery. A nonanatomic femoral fixation point should not be considered the cause of persistent pain and instability after MPFL reconstruction in all cases.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Currently, medial patellofemoral ligament (MPFL) reconstruction is the procedure of first choice for treating patients with chronic lateral patellar instability and at least two documented patellar dislocations [22]. Many surgical techniques with various femoral graft fixation sites have been described for the reconstruction of the MPFL, with generally good short- and mid-term clinical outcomes [22].
Interest in anatomic ligament reconstructions began with the anterior cruciate ligament (ACL) and now includes the MPFL, for which femoral anatomic attachment of grafts is increasingly favoured. Anything that is not completely anatomic seems to be perceived as incorrect, but high-level evidence to support that perception is lacking. Moreover, the normal anatomic location of the femoral MPFL attachment is not as well defined as for other knee ligaments [15, 27], and no definitive studies have analysed the effects of nonanatomic femoral fixation point on the outcome. Therefore, very little information exists about the best femoral attachment site of the graft, and controversy continues about the importance of an anatomic MPFL reconstruction.
As in ACL reconstruction surgery [12], changes in the femoral attachment site have been hypothesized to have a considerable effect on the relative length of the reconstructed MPFL as well as on the length change pattern of the graft throughout the dynamic range of knee motion. All these items will have an impact on failed surgeries.
Our study was designed to (1) investigate the effect of an ideal anatomic femoral attachment site on the dynamic length change pattern of a virtual MPFL graft from an extended knee to a highly flexed position with three-dimensional computed tomography (3D-CT) reconstructions; (2) determine the in vivo relative length and the length change pattern of the reconstructed MPFL; and (3) correlate femoral attachment positioning, length change pattern, and relative graft length with failed surgery as a clinical outcome. The final objective of the study was to demonstrate that a nonanatomic femoral fixation point should not be considered the cause of all cases of persistent pain and instability after an MPFL reconstruction.
Materials and methods
Between 2002 and 2012, 101 consecutive patients (104 knees) with chronic lateral patellar instability with at least two documented patellar dislocations underwent MPFL reconstruction at our institution. Of these 104 knees, 30 were available for evaluation, but only 24 were included in this study (see flow chart for patient enrolment, Fig. 1).
The study group consisted of 24 patients (17 females and seven males) with a mean age at the time of surgery of 23 years (range 16–38). Patients were evaluated at a mean of 5 years (range 2–10) after surgery. The MPFL reconstruction was performed using one-bundle reconstruction (partial-thickness quadriceps or semitendinosus tendon graft) in 16 cases and double-bundle reconstruction with semitendinosus tendon autograft in eight cases.
To control for confounding variables, all cases were preoperatively evaluated for trochlear dysplasia according to the Dejour [4] classification, either severe (grade C or D) or nonsevere (grade A or B), because a correlation between severe trochlear dysplasia and MPFL reconstruction failure has been observed [13, 16]. Other major factors that contribute to chronic lateral patellar instability that could also be confounding variables are less important than trochlear dysplasia, and therefore, we did not consider them in our study [17, 35].
At the final follow-up, 20 patients had satisfactory results, while four had nonsatisfactory results defined as failed surgery. MPFL reconstruction surgery was considered to have failed when the instability, anterior knee pain, or both recurred to the extent that a new surgical reconstruction of the MPFL was required. Results were considered satisfactory when the patient had no pain (excepting sporadic discomfort) or instability; performed the same physical activities, including sports, as before the injury; and was subjectively satisfied with the surgical procedure.
CT acquisition
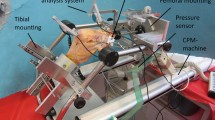
The operated knee was scanned with a high-spatial-resolution dynamic 256-detector row Brilliance iCT scanner (Philips Medical Systems, Eindhoven, the Netherlands) at five different knee flexion angles (0°, 30°, 60°, 90°, and 120°). Subjects were asked to be in a lateral position and to be relaxed. The flexion angle was determined by using a goniometer. The raw data sets were acquired under 64 × 0.6 mm collimation, rotation time 0.5 s, pitch 0.5, 120 kV, and automated mAs control. Lead aprons were used for all patients to shield their gonads. Images were reconstructed with 0.9 mm slice thickness, and a 3D high-resolution bone surface rendering for knee volumetric reconstruction was obtained at each knee angle.
Image analysis
The 3D surface rendering for knee reconstruction at 0° of knee flexion was chosen as a reference. To minimize technical errors in measurement, the femoral model at 0° of flexion was superimposed on each femoral model at 30°, 60°, 90°, and 120° of flexion using the surface-to-surface matching method [36]. The centre of the femoral and patellar tunnels was established (Fig. 2). The ideal femoral anatomic attachment point was determined by the method described by Fujino et al. [7] (Fig. 2). Sanchis-Alfonso et al. [23] have shown that the widely used method described by Schoettle et al. [24] to identify the femoral fixation point in MPFL reconstruction surgery is only an approximation and should not be the sole basis for identifying the femoral attachment location. The only way we can be sure of an anatomic femoral placement of the graft is to make an incision that is large enough to unequivocally identify the most important anatomic landmark, the adductor tubercle [23]. The method described by Fujino et al. [7] uses the adductor tubercle as a landmark to identify the femoral attachment of the MPFL. We believe that this method is the most accurate of the described methods, from an anatomic point of view. According to Fujino et al. [7], the femoral attachment of the MPFL is distal to the apex of the adductor tubercle and parallel to the long axis of the femur. In this study, the mean linear distance between the two points was 10.6 mm, and the position of the insertion site was consistent in all knees. In our study, the malposition of the femoral attachment was defined in relation to the ideal anatomic femoral attachment.
Anatomic femoral attachment (red circle) according to the method described by Fujino et al. [7]. Patellar attachments and nonanatomic femoral attachment performed during surgery (blue arrows). We defined the malposition of the femoral attachment in relation to the ideal anatomic femoral attachment
The length of the MPFL graft/virtual anatomic MPFL was defined as the linear distance between the centre of the femoral attachment site and the centre of the patellar attachment site (Fig. 3). Tateishi et al. [32] have demonstrated that the centre of the femoral drill hole position determines the graft length change pattern in patients with patellar instability. In the cases in which a patellar tunnel was not performed (four cases), a point that was 30 % of the distance from the superior pole of the patella [19] was marked, using the technique described by Yoo et al. [36]. Moreover, the length of the virtual native MPFL was calculated as the distance between the theoretical ideal anatomic femoral point and the centre of the patellar attachment performed during surgery (Fig. 3). The distance measured from the ideal anatomic femoral point to the patellar point served as a reference for calculating the relative length of the reconstructed MPFL. The length of the MPFL graft and the virtual native MPFL was measured at five different knee flexion angles. According to Smirk and Morris [27], length pattern changes are isometric when there is <5 mm of length change throughout the range of motion.
a A virtual anatomic MPFL (red lines) was created on the three-dimensional model. The length of the graft was defined as the linear distance between the centre of the femoral attachment site (red circle) and the centre of the patellar attachment site. b MPFL graft (blue lines) in a case with a double-bundle reconstruction with hamstring tendon autograft. Note that although we use a 3D model, the measurement is in 2D. (1) Proximal bundle, (2) distal bundle
Our study was approved by the Institutional Review Board at our institution (Hospital Universitario y Politécnico La Fe, Valencia, Spain, ID # 2013/0341), and informed consent was obtained from all patients.
Statistical analysis
All values were expressed as the mean ± SD. The differences in length among the different knee flexion positions in both virtual native and operated MPFL were analysed using a paired Student’s t test. The level of significance was set at p < 0.05 in all instances. All statistical analyses were performed using SPSS software, version 17 Institute (Cary, NC, USA).
Results
3D-CT reconstructions corroborated a nonanatomic MPFL femoral attachment site in all 24 MPFL reconstructed knees. In 4 of the 24 cases (17 %), the clinical result at the final follow-up was considered a failed surgery: three cases due to severe anterior knee pain and one case with recurrence of lateral patellar instability. Of the failed cases due to pain, two had a grade A trochlear dysplasia and one had a grade B dysplasia. No correlation existed between the severity of trochlear dysplasia and the failure of MPFL surgery due to pain. In the case that failed because of persistent instability, the trochlear dysplasia was a grade C, and the malposition of the femoral fixation point was very noticeable (Fig. 4).
Knee flexion had a significant effect on the length of the path between the femoral and patellar attachments of the MPFL. The measurements of the lengths of the anatomic virtual MPFL, the nonanatomic MPFL with a satisfactory result, and the nonanatomic MPFL with a nonsatisfactory result (severe pain) at 0°, 30°, 60°, 90°, and 120° of knee flexion are summarized in Table 1.
The length of the anatomic virtual MPFL increased during flexion from 0° to 30°, decreased nonsignificantly from 30° to 60°, and decreased significantly from 60° to 120°. Its maximum length was 56.4 ± 6.8 mm at 30° of knee flexion and was not statistically greater than the length measured at 0° (n.s.) or 60° (n.s.) of knee flexion. However, the lengths at 0°, 30°, and 60° were statistically greater than at 90° and 120° (p < 0.001) of knee flexion (Table 1; Fig. 5). This pattern was considered as the in vivo MPFL standard dynamic length change. We observed a graft length change from 0° to 30° of knee flexion of 2.8 ± 1.6 mm. The length change at 60° of knee flexion was 3.7 ± 2.5 mm; at 90°, it was 10.0 ± 3.6 mm; and at 120°, it was 16.1 ± 4.9 mm, always compared with its maximum length. The anatomic virtual MPFL was isometric between 0° and 30° in all cases. In 20 cases (83 %), the ligament was isometric from 0° to 60° of knee flexion. Beyond 60° of knee flexion, the graft became progressively lax, and the isometry was lost.
Curves representing the mean length with different knee flexion angles (0°, 30°, 60°, 90°, and 120°) of the virtual anatomic MPFL, a nonanatomic MPFL reconstruction with satisfactory result, and a nonanatomic MPFL reconstruction with a nonsatisfactory result (severe anterior knee pain). Note the length change pattern of the anatomic virtual MPFL (red line), the nonanatomic MPFL reconstruction with satisfactory result (blue line), and the nonanatomic MPFL reconstruction with severe anterior knee pain (black line)
The length of the nonanatomic reconstructed MPFL with a satisfactory result was decreased during flexion from 0° to 120°. Its maximum length was 51.6 ± 4.6 mm at 0° of knee flexion, but it was not statistically greater than the length measured at 30° (n.s.) of flexion. However, the lengths at 0° and 30° were statistically greater than those at 60°, 90°, and 120° (p < 0.01) of knee flexion (Table 1; Fig. 5). We observed a graft length change from 0° to 30° of knee flexion of 2.4 ± 1.5 mm. The length change at 60° was 7.5 ± 2.9 mm; at 90°, it was 14.2 ± 5.2 mm; and at 120°, it was 18.7 ± 6.1 mm, always compared with its maximum length. The nonanatomic MPFL reconstruction with satisfactory results was isometric between 0° and 30° in all cases. Only in four cases (20 %) was the ligament isometric from 0° to 60° of knee flexion. However, beyond 60° of knee flexion, the graft became progressively lax and the isometry was lost.
A nonanatomic MPFL with a satisfactory result was always shorter than an anatomic ligament (8.5 ± 6.3 %). A failed MPFL reconstruction was significantly shorter than an anatomic ligament (27.1 ± 13.3 %) (Table 1; Fig. 6). In the three cases of a failed MPFL reconstruction due to severe pain, the reconstruction was isometric from 0° to 120° of knee flexion (Figs. 5, 6).
The measurements of the length of the proximal and distal bundles of the anatomic virtual MPFL double-bundle reconstruction and the nonanatomic MPFL double-bundle reconstruction with a clinical satisfactory result at 0°, 30°, 60°, 90°, and 120° of knee flexion are summarized in Tables 2 and 3. No significant differences were found between the two patellar attachment sites in the length change pattern or in the ligament isometry for the double-bundle MPFL reconstruction (Figs. 7, 8).
Length change pattern of the graft in the eight cases of virtual anatomic double-bundle MPFL reconstruction. In all of these cases, the femoral fixation point is the virtual anatomic point determined using Fujino’s method. The two patellar fixation points are those made during the surgical procedure
Length change pattern of the graft in the eight cases of a nonanatomic double-bundle MPFL reconstruction with satisfactory result. In these cases, the femoral fixation point is the initial one made during the surgical procedure. The two patellar fixation points are also the ones made during the surgical procedure
Discussion
The most important finding of the present study was that the femoral attachment point is of utmost importance for MPFL graft length change during knee flexion and for relative graft length. Both factors will influence the long-term success and the failure rate of the MPFL reconstructive surgery.
To the best of our knowledge, only five studies evaluating the in vivo MPFL kinematics have been published [9, 11, 21, 30, 36]. However, all of them were performed in anatomically normal knees by 3D-CT [9, 21, 30, 36] or open MRI [11]. 3D-CT has also been used previously to noninvasively measure in vivo cruciate ligament length at different flexion angles [14, 20, 37]. Our study is the first to evaluate MPFL kinematics in patients with chronic lateral patellar instability. We evaluated both the kinematics of the graft used to reconstruct the MPFL as well as the virtual native anatomic MPFL kinematics. Regarding the length change pattern of the anatomic ligament during knee flexion, we found the greatest distance between attachment points at 30° of knee flexion, in accordance with previous studies [30, 36], and a significant approximation among the attachment points when the knee was flexed over 60°, in agreement with other authors [11, 36]. 3D-CT scan reconstruction offered an excellent definition of the bony anatomy, allowing for an accurate location of the MPFL femoral fixation site. Moreover, the wide gantry of the CT scan permitted higher angles of the knee than with MRI and facilitated scanning of tall patients. Finally, CT scan produced fewer postsurgical and metal artefacts than MRI. Although a disadvantage of CT is its use of ionizing radiation, no critical organs were within the scanning region; however, the risk of radiation-induced bone cancer is uncertain.
Although the ligament tension was not measured, several authors have demonstrated that a change in the ligament length reflects tension changes in this particular ligament [8, 18, 25, 31]. Therefore, we can infer that the native anatomic ligament is more tense during the first 30° of knee flexion and then loses a considerable amount of tension with higher degrees of knee flexion. As shown by previous studies [1, 3, 5, 10], this pattern shows that the MPFL contribution to resisting lateral patellar dislocation is greatest during the first 30° of knee flexion. Precisely after 30° of knee flexion, lateral patella stability depends more on the femoral trochlea than on the MPFL [5, 10]. A similar pattern in length change, in which the greatest separation of the attachment points occurs during the first 30° of flexion and a significant approximation of the femoral and patellar attachment points is seen at more than 30° of flexion, was found in MPFL grafts with nonanatomic femoral attachment points and a good clinical outcome. In contrast, this length change pattern is lost in reconstructive MPFL surgeries with nonanatomic femoral attachment points that have poor clinical results. In our cases with double-bundle reconstruction, no significant differences were seen between the two patellar attachment points in the length changes of the MPFL. This finding is in agreement with the results obtained by Yoo et al. [36] and with the study by Tateishi et al. [32], who found that the MPFL length changes depend on the femoral attachment site more than on the patellar attachment site. Therefore, the choice of the femoral attachment point is much more crucial for the success of the MPFL reconstructive surgery than the patellar attachment.
Another key element for obtaining a good clinical result in MPFL reconstruction is the correct graft length, which is closely linked to the location of the femoral attachment point. We have observed that a very short graft is associated with a poor clinical result. In this way, experimental studies [6] have shown that a short graft increases its tension with knee flexion, and this will eventually cause patellofemoral osteoarthritis.
Another controversial subject in MPFL surgery that is clinically relevant is the knee flexion angle at which the graft is fixed [22]. Theoretically, the graft should be fixed in the flexion angle at which its length is greatest. Our data suggest that the best flexion angle for fixation should be 30° in the cases with an anatomic femoral fixation point because this flexion angle is where the graft is longest.
Most authors consider that isometry does not exist during the entire flexion extension range [27, 28, 34], which is in agreement with the findings of our clinical series. However, in a recently published paper by Stephen et al. [29], the authors found that the MPFL was isometric from 0° to 110°. In our virtual anatomic MPFL reconstructions, we observed that the isometry was maintained from 0° to 60°, following the isometry criteria defined by Smirk and Morris [27]. As previously mentioned, the patella is most vulnerable to dislocation in the first 30° of knee flexion. Therefore, if the graft remains isometric from 0° to 30°, the patella will be protected from lateral dislocations [27]; it does not matter whether the graft loses tension with higher degrees of knee flexion. In our nonanatomic reconstructions with satisfactory clinical results, isometry was achieved from 0° to 30°, and the graft length was at least similar to the anatomic virtual ligament. In the cases in which surgery failed, this normal pattern of isometry was lost.
There is currently debate about the exact consequences of a nonanatomic MPFL reconstruction for the clinical results. There are only two papers that correlate the femoral fixation point during MPFL reconstruction surgery with clinical results. Servien et al. [26] found no negative effects of a nonanatomic femoral fixation point on the clinical results after a 2-year follow-up. A possible reason for this might be that the femoral fixation point was close enough to its ideal position to avoid having a negative effect. In our series, we found negative clinical consequences only with fixation points that were too anterior. Servien et al. [26] might also not have found a correlation between the nonanatomic femoral fixation point and the clinical result because of the short follow-up of their patients (2 years). This is particularly relevant with regard to the risk of developing osteoarthritis. A nonanatomic fixation point is a risk factor for surgery failure, as shown by Camp et al. [2], who observed that 80 % of patients had a new patella dislocation 4 years after surgery. In contrast, in our 5 or more years of follow-up of cases with nonanatomic femoral fixation points, no cases of new patellar dislocations were found.
Potentially meaningful clinical implications may be drawn from our findings in the context of MPFL reconstruction surgery. In a knee with a chronic lateral patellar instability, some degree of chondropathy of the medial facet of the patella is frequently found. If the graft we use to replace the MPFL in such a knee is more robust and rigid than the native MPFL, maintaining isometry during the entire range of motion of the knee would likely produce greater patellofemoral compression in a joint, causing the pre-existing medial patellar chondropathy to worsen. Therefore, in a knee with chronic lateral patellar instability, having ligament isometry just from 0° to 30° would be desirable. Thaunat and Erasmus [33] referred to this as “favourable anisometry”, which our goal of stabilizing the patella in the 0°–30° range would achieve.
One of the strongest points of our study is that it was conducted in vivo, preserving the effect that soft tissues and surrounding muscle forces have on the patellofemoral alignment. Also, in our study, the knees are from young patients, with anatomic stigmas of a knee with a chronic lateral patellar instability.
However, the study has several limitations. First, a relatively small cohort was analysed. Secondly, despite attempts to limit potential confounding factors, it is not always possible to control some individual factors. Thirdly, grafts were analysed in non-weight-bearing conditions, and the effects of weight on the dynamics of the patellofemoral joint could therefore not be ascertained. The fourth weakness is that even though the study model was a 3D-CT knee, the measurements were in 2D and a ligament is not a strictly linear structure, but rather curvilinear. Fifth, the in vivo knee joint kinematics were only acquired in five flexion positions due to time and ionizing radiation exposure constraints. Moreover, if excessive tension was applied on the graft, the measured distance between the femoral and the patella fixation points could have been artificially shortened, which could have biased the final results. Finally, as far as we know, very few authors have used this methodology to evaluate the MPFL. Therefore, more studies will be necessary to validate this evaluation method and to confirm our results.
This study shows that a nonanatomic femoral fixation point is not always clinically responsible for persistent pain and instability after MPFL reconstruction.
Conclusion
Establishing an anatomic femoral fixation point during MPFL reconstruction is an easy and reproducible way to achieve an optimal pattern of change in graft length, isometry, and an ideal graft length. However, a nonanatomic reconstruction that reproduces isometry, the pattern for the change in length, and the length of a native MPFL will provide a satisfactory clinical result.
Change history
02 November 2018
Unfortunately, the author missed out to indicate the affiliation which is basic requirement as a part of his thesis. The affiliation is now updated here.
02 November 2018
Unfortunately, the author missed out to indicate the affiliation which is basic requirement as a part of his thesis. The affiliation is now updated here.
References
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee 10(3):215–220
Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ (2010) Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med 38(11):2248–2254
Conlan T, Garth WP Jr, Lemons JE (1993) Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 75(5):682–693
Dejour D, Le Coultre B (2007) Osteotomies in patellofemoral instabilities. Sports Med Arthrosc 15:39–46
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26(1):59–65
Elias JJ, Cosgarea AJ (2006) Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med 34:1478–1485
Fujino K, Tajima G, Yan J, Kamei Y, Maruyama M, Takeda S, Kikuchi S, Shimamura T (2015) Morphology of the femoral insertion site of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 23(4):998–1003
Good L (1995) In vitro correlation between tension and length change in an anterior cruciate ligament substitute. Clin Biomech (Bristol, Avon) 10(4):200–207
Graf M, Diether S, Vlachopoulos L, Fucentese S, Fürnstahl P (2014) Automatic string generation for estimating in vivo length changes of the medial patellofemoral ligament during knee flexion. Med Biol Eng Comput 52(6):511–520
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 349:174–182
Higuchi T, Arai Y, Takamiya H, Miyamoto T, Tokunaga D, Kubo T (2010) An analysis of the medial patellofemoral ligament length change pattern using open-MRI. Knee Surg Sports Traumatol Arthrosc 18:1470–1475
Hirschmann MT, Mathis D, Rasch H, Amsler F, Friederich NF, Arnold MP (2013) SPECT/CT tracer uptake is influenced by tunnel orientation and position of the femoral and tibial ACL graft insertion site. Int Orthop 37(2):301–309
Hopper GP, Leach WJ, Rooney BP, Walker CR, Blyth MJ (2014) Does degree of trochlear dysplasia and position of femoral tunnel influence outcome after medial patellofemoral ligament reconstruction? Am J Sports Med 42(3):716–722
Jeong WS, Yoo YS, Kim DY, Shetty NS, Smolinski P, Logishetty K, Ranawat A (2010) An analysis of the posterior cruciate ligament isometric position using an in vivo 3-dimensional computed tomography-based knee joint model. Arthroscopy 26(10):1333–1339
Kang HJ, Wang F, Chen BC, Su YL, Zhang ZC, Yan CB (2010) Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 18:1511–1516
Kita K, Tanaka Y, Toritsuka Y, Amano H, Uchida R, Takao R, Horibe S (2015) Factors affecting the outcomes of double-bundle medial patellofemoral ligament reconstruction for recurrent patellar dislocations evaluated by multivariate analysis. Am J Sports Med. doi: 10.1177/0363546515606102
Matsushita T, Kuroda R, Oka S, Matsumoto T, Takayama K, Kurosaka M (2014) Clinical outcomes of medial patellofemoral ligament reconstruction in patients with an increased tibial tuberosity-trochlear groove distance. Knee Surg Sports Traumatol Arthrosc 22(10):2438–2444
Moritomo H, Noda K, Goto A, Murase T, Yoshikawa H, Sugamoto K (2009) Interosseous membrane of the forearm: length change of ligaments during forearm rotation. J Hand Surg Am 34(4):685–691
Nomura E, Inoue M, Osada N (2005) Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc 13(7):510–515
Nishimori M, Deie M, Adachi N, Nakamae A, Ishifuro M, Ochi M (2014) Simulated anterior cruciate ligament reconstruction using preoperative three-dimensional computed tomography. Knee Surg Sports Traumatol Arthrosc 22(5):1175–1181
Oka S, Matsushita T, Kubo S, Matsumoto T, Tajimi H, Kurosaka M, Kuroda R (2014) Simulation of the optimal femoral insertion site in medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3192-1
Sanchis-Alfonso V (2014) Guidelines for medial patellofemoral ligament reconstruction in chronic lateral patellar instability. J Am Acad Orthop Surg 22:175–182
Sanchis-Alfonso V, Ramirez-Fuentes C, Montesinos-Berry E, Aparisi-Rodriguez F, Martí-Bonmatí L (2015) Does radiographic location ensure precise location of the femoral fixation site in medial patellofemoral ligament surgery? Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3523-x
Schoettle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35:801–804
Seo YJ, Song SY, Kim IS, Seo MJ, Kim YS, Yoo YS (2014) Graft tension of the posterior cruciate ligament using a finite element model. Knee Surg Sports Traumatol Arthrosc 22(9):2057–2063
Servien E, Fritsch B, Lustig S, Demey G, Debarge R, Lapra C, Neyret P (2011) In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med 39:134–139
Smirk C, Morris H (2003) The anatomy and reconstruction of the medial patellofemoral ligament. Knee 10:221–227
Steensen RN, Dopirak RM, McDonald WG 3rd (2004) The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med 32:1509–1513
Stephen JM, Lumpaopong P, Deehan DJ, Kader D, Amis AA (2012) The medial patellofemoral ligament: location of femoral attachment and length change patterns resulting from anatomic and nonanatomic attachments. Am J Sports Med 40(8):1871–1879
Song SY, Pang CH, Kim CH, Kim J, Choi ML, Seo YJ (2015) Length change behavior of virtual medial patellofemoral ligament fibers during in vivo knee flexion. Am J Sports Med 43(5):1165–1171
Tan J, Xu J, Xie RG, Deng AD, Tang JB (2011) In vivo length and changes of ligaments stabilizing the thumb carpometacarpal joint. J Hand Surg Am 36(3):420–427
Tateishi T, Tsuchiya M, Motosugi N, Asahina S, Ikeda H, Cho S, Muneta T (2011) Graft length change and radiographic assessment of femoral drill hole position for medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19:400–407
Thaunat M, Erasmus PJ (2007) The favourable anisometry: an original concept for medial patellofemoral ligament reconstruction. Knee 14:424–428
Victor J, Wong P, Witvrouw E, Sloten JV, Bellemans J (2009) How isometric are the medial patellofemoral, superficial medial collateral, and lateral collateral ligaments of the knee? Am J Sports Med 37:2028–2036
Wagner D, Pfalzer F, Hingelbaum S, Huth J, Mauch F, Bauer G (2013) The influence of risk factors on clinical outcomes following anatomical medial patellofemoral ligament (MPFL) reconstruction using the gracilis tendon. Knee Surg Sports Traumatol Arthrosc 21(2):318–324
Yoo YS, Chang HG, Seo YJ, Byun JC, Lee GK, Im H, Song SY (2012) Changes in the length of the medial patellofemoral ligament: an in vivo analysis using 3-Dimensional computed tomography. Am J Sports Med 40(9):2142–2148
Yoo YS, Jeong WS, Shetty NS, Ingham SJ, Smolinski P, Fu F (2010) Changes in ACL length at different knee flexion angles: an in vivo biomechanical study. Knee Surg Sports Traumatol Arthrosc 18(3):292–297
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sanchis-Alfonso, V., Ramirez-Fuentes, C., Montesinos-Berry, E. et al. Femoral insertion site of the graft used to replace the medial patellofemoral ligament influences the ligament dynamic changes during knee flexion and the clinical outcome. Knee Surg Sports Traumatol Arthrosc 25, 2433–2441 (2017). https://doi.org/10.1007/s00167-015-3905-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3905-0