Abstract
Purpose
Anterior knee pain is a major reason for unsatisfied patients after total knee arthroplasty (TKA). Since malposition and increased retropatellar peak pressure are supposed to contribute to pain, we conducted this in vitro study to analyse the influence of mediolateral tibial component position on tibiofemoral and patella kinematics as well as retropatellar pressure.
Methods
Eight fresh frozen cadaver specimens were tested after a fixed-bearing TKA. To evaluate the influence of mediolateral tibial component position, special inlays with 3 mm of medialization and lateralization were constructed. For the analysis, a weight-bearing knee rig under a loaded squat from 20° to 120° of flexion was used. Tibiofemoral and patella kinematics were measured with an ultrasonic-based three-dimensional motion analysis system. Additionally, retropatellar pressure distribution was registered with a pressure-sensitive film.
Results
Alteration of mediolateral tibial component position by 3 mm did not reveal a significant influence on retropatellar peak pressure (7.5 ± 2.5 vs. 7.2 ± 2.6 MPa). Regarding tibiofemoral kinematics, 3-mm medialization of the tibial baseplate significantly increased lateral femoral rollback and femorotibial external rotation. Medialization of 3 mm also significantly increased the relative medial patella shift and decreased lateral patella tilt.
Discussion
Medialization of the tibial baseplate came along with more lateral rollback and external femorotibial rotation. For the positioning of the tibial baseplate, rotational alignment seems to be more important than mediolateral orientation. Since retropatellar peak pressure remained rather unchanged, the tibial baseplate should be placed by the surgeon looking for a maximal tibial coverage without overhang.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For patients with advanced osteoarthritis of the knee, total knee arthroplasty (TKA) is the surgical therapy of choice [2, 5]. Since decades, this is a routine procedure with continuous improvements regarding implant design, material choice as well as surgical technique [28]. It is still not possible, however, to recreate the natural kinematics of the knee, leaving up to 18 % of patients unsatisfied after receiving a TKA [9, 30, 40]. Some 9 % of TKA revisions are performed due to knee pain [31]. Besides aseptic loosening, polyethylene (PE) wear, and instability, anterior knee pain is one of the main causes for post-operative pain affecting up to 12 % of patients [6, 37, 38]. This high number is supposedly caused by an increased post-operative retropatellar pressure [12, 19].
Since post-operative knee kinematics influences stability, aseptic loosening due to PE wear, and anterior knee pain, positioning of the implants is crucial for a successful TKA [14, 22, 26, 42].
For the tibial component, sizing is often difficult resulting in frequent (61 %) mediolateral oversizing [4, 13] leading to post-operative pain and decreased flexion [3, 21]. On the contrary, a reduced coverage of the medial proximal tibia with missing medial cortical support can lead to local bone resorption [15].
To our knowledge, there are neither in vitro nor clinical studies on the impact of mediolateral positioning of the tibial component. It was hypothesized that according to the functional medial displacement of the tibial tubercle [10, 29, 36], a slight lateralization of the tibial component would lead to a medial shift of the patella along with a decreased retropatellar pressure and superior patella tracking [1, 39].
Therefore, the purpose of this study was to examine the in vitro influences of a medialization and lateralization of the tibial baseplate on tibiofemoral and patella kinematics as well as retropatellar pressure after TKA using a knee rig model on cadaver specimens. The results can give guidance to surgeons on intraoperative tibial component alignment.
Materials and methods
For this in vitro study, eight fresh frozen human knee specimens (age 58.9 ± 11.7 years (range 47–82); 3 females, 5 males; height: 176.9 ± 5.9 cm; weight: 81.5 ± 10.6 kg) were used. Exclusion criteria were severe bone deformity like valgus or varus deviations ≥10°. The specimens were prepared preserving the surrounding soft tissue (including capsule, ligaments, and tendons) and shortened 20 cm proximal and 15 cm distal to the joint line. Onto which the prepared tendons metallic finger traps (Bühler-Instrumente Medizintechnik GmbH, Tuttlingen, Germany) were fixed using suture material (FibreWire, Arthrex, Munich, Germany). Additionally, the fibula head and the proximal tibia were connected with a 4.5-mm screw. Afterwards, the shortened ends of the tibial and the femoral bone were embedded into metallic pots using epoxy resin (Rencast FC53, Huntsman, Basel, Switzerland).
Radiographs in anterior–posterior, sagittal, and sunrise view were taken from all specimens before and after the implantation. Preoperative radiographs were used to determine the degree of osteoarthritis and to exclude bone deformities. The post-operative radiographs ensured the correct positioning of the prostheses.
Implantation
For the experiments, a fixed-bearing, cruciate-retaining TKA (Columbus CR Aesculap, Tuttlingen, Germany) was implanted together by the two first authors A.S. and A.F. using a subvastus approach. To achieve ligament balancing, a tibia-first technique was performed. All tibial components were aligned to the medial third of the tibial tuberosity as this was identified as the best rotational positioning [23]. The tibial baseplate of the Columbus CR knee system has a symmetrical shape. All tibial baseplates were positioned in a manner to maximize tibial coverage without overhang [24].
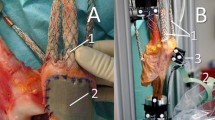
The medialization and lateralization of the tibial component was achieved by constructing different inlays using CAD data of the prosthesis and a CAD-Software (Catia V5 R19, Dassault Systems, France). The original inlay was defined as the neutral position. Additionally, two inlay variations with 3-mm medialization and 3-mm lateralization were produced out of the original ultra-high molecular weight polyethylene (UHWPE) by the manufacturer (Fig. 1). The inlays were made of standard UHWPE. The connection mechanism to the tibial baseplate and polyethylene was identical to the standard inlay (snap-fit mechanism).
Biomechanical test set-up
Before mounting the specimens onto the knee rig, the unresurfaced patella was prepared by removing osteophytes. A pressure-sensitive film (K-Scan 4000, Tekscan Inc., Boston, USA) with a resolution of 62 sensels per cm2 (totally 572 sensels) and a maximum pressure capacity of 1500 PSI (~10 MPa) was used to measure retropatellar pressure distribution. The film was fixed to the retropatellar surface with subcutaneous 1.0 suture material after gluing a peace of 0.125-mm Teflon tape (PTFE-tape) on the sensor to avoid shear forces. Before the measurements, the sensor film was calibrated according to the manufacturer’s instructions by applying a two-point load using a material testing machine (Z010, Zwick, Ulm, Germany).
The measurements were taken using a well-established knee rig with six degrees of freedom (DOF) [32–34]. The knee was flexed from 20° to 120° and extended back once again to 20°. The motion was mediated by a linear drive (Driveset M150, Systec GmbH, Muenster, Germany) with a constant velocity of 3°/s. The flexion angle was measured by two angle sensors (8820 Burster, Gernsbach, Germany) incorporated into the “hip unit” and the “ankle unit” of the knee rig. The rectus muscle force was induced using a second linear drive (Driveset M180, Systec GmbH, Muenster, Germany). A force sensor (8417-6002 Burster, Gernsbach, Germany) was installed near the tendon to measure the actual rectus force. Other muscle forces (medial vastus, lateral vastus, semitendinosus, and biceps femoris muscle) were simulated passively with 2-kg weights attached to each tendon.
The originated ground reaction force was detected by a force moment sensor (FN 7325-31 FGP Sensors, Cedex, France) with six DOF installed under the ankle unit. To achieve a constant ground reaction force of 50 N, the two linear drives (for motion generation and rectus force simulation) were operated by a LabVIEW code (version 8.6, National Instruments, Austin, TX, USA) on a personal computer using Real-Time and PID-Control Packages.
The tibial baseplate position on the tibiofemoral and patella kinematics was evaluated with an ultrasonic-based three-dimensional motion analysis system (Zebris CMS 20, Isny, Germany). Three miniature transmitters were attached to the femur, the patella, and the tibia (Fig. 2), to register the rotation and translation of the femur, the patella, and the tibia with a resolution of 0.1° and 0.1 mm. Sufficient measurement reliability for kinematics and retropatellar pressure was assured by test–retest analysis; the accuracy of the measurement system has been described in a former study [32]. To describe the relative motion of the patella, the definitions of Bull et al. [7] (flexion, rotation, tilt, and shift) were utilized. This study was approved by the ethical committee of University of Munich (LMU).
Statistical analysis
Absolute values (at 20° and 120° of flexion) and peak values of the kinematic data, rectus muscle, and retropatellar pressure were presented using mean ± standard deviation. Measurements with neutral tibia as well as tibial medialization and lateralization were compared using mixed effects models with a random intercept per specimen. The results of the mixed effect models were illustrated as the mean of the regression coefficients and a 95 % confidence interval. For the analyses, SPSS software (SPSS release 21.0, IBM, New York, USA) was used. Results with p < 0.05 were considered statistically significant.
Results
Simulated medialized and lateralized baseplate position had no significant influence on the ground reaction force. In contrast, the regression coefficient of the mixed effects model in relation to the rectus muscle force was altered significantly even though differences in average absolute values were within 30 N (medialization 685.6 ± 55.7 N vs. lateralization 711.2 ± 72.7 N). Regarding the retropatellar peak pressure, the mediolateral position of the tibial component had only a minor effect with no significant difference concerning the regression coefficient (Table 1). Compared to the retropatellar peak pressure of 7.3 ± 2.6 MPa in the neutral position, medialization of 3 mm led to a minor increase (7.5 ± 2.5 MPa), while lateralization of 3 mm showed a slight decrease in values (7.2 ± 2.6 MPa). The highest peak pressure differences were measured in high flexion angles (>80°).
Even though the retropatellar peak pressure remained rather unchanged, there was a significant difference in patella kinematic regarding regression coefficients of patella shift, patella rotation, and patella tilt (Table 1). Regarding patella shift at 120° flexion, the neutral position revealed a relative medial shift of 2.7 ± 2.6 mm compared to the position in 20° of flexion. Medialization of the tibia component increased relative shift to 4.3 ± 1.8 mm starting from a more lateral position, while lateralization decreased the relative shift to 1.6 ± 2.7 mm (Fig. 3). For patella rotation and patella tilt, the clinical relevant differences in absolute values in high flexion were only small. At 120° flexion, the mean difference in patella rotation between the three variants was 0.4° and regarding patella tilt also 0.4°. Patella flexion remained unchanged in all three variants (regression coefficient n.s., Table 1).
Similar to patella kinematics, the mediolateral position of the tibial component led to a significant alteration of the regression coefficient of the mixed effects model concerning the kinematic of the femorotibial joint (Table 1). Especially for the lateral compartment, the rollback increased with 3-mm medialization by an average of 2.3 mm and decreased with 3-mm lateralization by 1.5 mm compared to the neutral position in 120° flexion. In contrast, the alteration of rollback for the medial compartment was smaller in magnitude and in pointed in the opposite direction (Fig. 4). In 120° flexion, lateralization revealed 1.9 mm and medialization 1.2 mm less rollback of the medial condyle compared to the neutral position. Consequently, the medialized version revealed significantly more femorotibial external rotation in the tibia during one loaded squat with 7.0° ± 3.1° compared to the neutral version (4.1° ± 2.3°) and the lateralized version (3.9° ± 2.3°) (Table 1).
Discussion
The most important finding of this study was that the mediolateral position of the tibial component has no significant influence on retropatellar peak pressure. These measurements were contrary to the expected mechanical changes. Theoretically, a lateralization of the tibial component should lead to a kinematically derived medialization of the tibial tuberosity. This should consequently medialize the patella and reduce retropatellar pressure [10, 36]. This relationship could not be confirmed with the measurements taken in this study. Even though the mediolateral position of the patella was more lateral in extension when using a medialized tibial baseplate, the increased relative medial patella shift resulted in a similar patella position for all three tested variants in clinical more relevant flexion of the knee (Fig. 3). A reason for the increased relative shift could be observed in the elevated femorotibial external rotation of the medialized baseplate. Combining these kinematical effects could be used to explain the rather unchanged retropatellar pressure.
The influence of the mediolateral tibial baseplate position on the kinematic of the tibiofemoral joint was also unexpected. In particular, the increased lateral rollback combined with an enlarged femorotibial external rotation for the medialized variant is in tendency closer to the kinematical findings in a normal tibiofemoral joint [11]. Regarding absolute values, the rollback at the lateral compartment of the knee after a TKA with medialized baseplate was 9.7 ± 4.7 mm. This was still much smaller than previously determined in the normal active arc of flexion of the knee, which was found to be roughly 15 mm [11] but similar to measurement taken on a medial stabilized TKA [27].
An explanation for the kinematic alteration associated with the mediolateral baseplate position is difficult to find. However, ligament tension can alter knee kinematics [35], and a possible reason could be seen in the modified tensions of the collateral ligaments. Similar to measurements of ligament tension in malrotated tibial components [25], medialization of the baseplate could lead to increased tension of the medial collateral ligament and reduced tension of the lateral collateral ligament [20]. This shift of tension could stabilize the medial more than the lateral compartment, leading to a pronounced lateral rollback and an increased femorotibial external rotation.
However, there are references reporting better clinical results in regard to external femorotibial rotation with flexion after TKA [22]. It is not evident if a more natural kinematic movement of the tibiofemoral joint after TKA also reveals superior clinical results [16, 18]. A disadvantage of a medialized tibial baseplate is the increased tension of the medial collateral ligament as well as a potential medial overhang resulting in possible sources for post-operative pain [4]. Therefore, surgeons should place the tibial baseplate without overhang [24] and an adequate rotational alignment [23, 34].
Compared to previous studies with the same knee rig, it becomes evident that mediolateral position of the tibial component has less influence on retropatellar peak pressure than the rotation of the femoral or tibial component. A comparison with the measurements taken by Steinbrück et al. 2015 [34] on tibial components with 3° external and 3° internal rotation is especially interesting. Regarding maximal retropatellar peak pressure, the difference between 3° internal and 3° external rotation was 0.7 MPa (8.5 ± 2.3 vs. 7.8 ± 2.5 MPa). This result is more than two times higher compared to 3-mm medialization and 3-mm lateralization which resulted in a value of 0.3 MPa (7.5 ± 2.5 vs. 7.2 ± 2.6 MPa). Even though the patella significantly shifted medially during flexion with medialization of the tibial baseplate, the effect on the clinical more relevant [12, 19] retropatellar peak pressure was only minor. Together with findings of the former study [34] detecting no significant influence of rotational alignment on patella shift, it seems that patella shift has less influence on retropatellar peak pressure. This applies at least for the range of patella shift measured in this study (2.7 mm, range 1.6 vs. 4.3 mm).
A further aspect is patella tilt. External rotation as well as lateralization of the tibial component resulted in a significant lateral patella tilt. Both alterations should theoretically provoke an indirect medialization of the tibial tuberosity. Other than expected, not a medial but a lateral tilt of the patella was measured with the lateralized tibial baseplate. These findings are also supported by Nagamine et al. [29]. In their study, a medial transfer of the tibial tubercle by an average of 9.5 mm in a TKA model with 8.0° internal rotation of femur component also led to a more lateral patella tilt.
Looking at the results of the femorotibial rotation before and after TKA in a former study [32], a lower femorotibial external rotation after TKA could be demonstrated, which is also in accordance with in vivo studies [8, 17]. The kinematics of the medialized tibial component was more comparable to a natural knee in the same rig with a higher degree of external femorotibial rotation with flexion.
Similar to all in vitro studies with cadaver specimens examined in a knee rig, this evaluation has the limitation of a simulated load squat. In such a set-up, most activities of daily living, such as walking, rising from a chair, or climbing stairs, cannot be simulated. But nevertheless the results of this simulation can provide evidence about the influence of implant position on kinematics and retropatellar pressure during daily activities. We tested all modifications of implantation in between one specimen, and due to paired observations, statistical significance is supported. Although a higher number of specimens might have supported our results substantially.
Additionally, the results of this study only apply to TKA with fixed-bearing inlays. The results cannot be transferred to other TKA designs. In particular, posterior stabilized TKA would result in a different rollback and therefore different tibiofemoral and patella kinematics [41].
For reducing the risk of post-operative pain and local bone resorption, surgeons should place the tibial baseplate with regard to a maximal tibial coverage without overhang and an adequate rotational alignment to the medial third of the tibial tuberosity.
Conclusion
In conclusion, medialization of the tibial baseplate revealed more lateral rollback along with an external femorotibial rotation, which supposedly replicates more natural kinematics. Although a medial positioning of the tibial baseplate cannot be advised as retropatellar peak pressure remains unchanged, a risk of tibial malpositioning is predominant. For the positioning of the tibial baseplate, rotational alignment seems to be more important than mediolateral orientation.
References
Amis AA (2007) Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc 15(2):48–56
Anderson JG, Wixson RL, Tsai D, Stulberg SD, Chang RW (1996) Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty 11(7):831–840
Bonnin MP, Saffarini M, Shepherd D, Bossard N, Dantony E (2015) Oversizing the tibial component in TKAs: incidence, consequences and risk factors. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3512-0
Bonnin MP, Schmidt A, Basiglini L, Bossard N, Dantony E (2013) Mediolateral oversizing influences pain, function, and flexion after TKA. Knee Surg Sports Traumatol Arthrosc 21(10):2314–2324
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63
Boyd AD Jr, Ewald FC, Thomas WH, Poss R, Sledge CB (1993) Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am 75(5):674–681
Bull AM, Katchburian MV, Shih YF, Amis AA (2002) Standardisation of the description of patellofemoral motion and comparison between different techniques. Knee Surg Sports Traumatol Arthrosc 10(3):184–193
Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A (2004) A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 428:180–189
Dunbar MJ, Robertsson O, Ryd L, Lidgren L (2001) Appropriate questionnaires for knee arthroplasty. Results of a survey of 3600 patients from The Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br 83(3):339–344
Elias JJ, Carrino JA, Saranathan A, Guseila LM, Tanaka MJ, Cosgarea AJ (2014) Variations in kinematics and function following patellar stabilization including tibial tuberosity realignment. Knee Surg Sports Traumatol Arthrosc 22(10):2350–2356
Freeman MA, Pinskerova V (2005) The movement of the normal tibio-femoral joint. J Biomech 38(2):197–208
Fuchs S, Skwara A, Tibesku CO, Rosenbaum D (2005) Retropatellar contact characteristics before and after total knee arthroplasty. Knee 12(1):9–12
Hartel MJ, Loosli Y, Delfosse D, Diel P, Thali M, Ross S, Kohl S, Eggli S (2014) The influence of tibial morphology on the design of an anatomical tibial baseplate for TKA. Knee 21(2):415–419
Howell SM, Hodapp EE, Vernace JV, Hull ML, Meade TD (2013) Are undesirable contact kinematics minimized after kinematically aligned total knee arthroplasty? An intersurgeon analysis of consecutive patients. Knee Surg Sports Traumatol Arthrosc 21(10):2281–2287
Innocenti B, Truyens E, Labey L, Wong P, Victor J, Bellemans J (2009) Can medio-lateral baseplate position and load sharing induce asymptomatic local bone resorption of the proximal tibia? A finite element study. J Orthop Surg Res 4:26
Ishida K, Matsumoto T, Tsumura N, Iwakura T, Kubo S, Iguchi T, Akisue T, Nishida K, Kurosaka M, Kuroda R (2014) No difference between double-high insert and medial-pivot insert in TKA. Knee Surg Sports Traumatol Arthrosc 22(3):576–580
Karrholm J, Jonsson H, Nilsson KG, Soderqvist I (1994) Kinematics of successful knee prostheses during weight-bearing: three-dimensional movements and positions of screw axes in the Tricon-M and Miller-Galante designs. Knee Surg Sports Traumatol Arthrosc 2(1):50–59
Kim YH, Yoon SH, Kim JS (2009) Early outcome of TKA with a medial pivot fixed-bearing prosthesis is worse than with a PFC mobile-bearing prosthesis. Clin Orthop Relat Res 467(2):493–503
Kulkarni SK, Freeman MA, Poal-Manresa JC, Asencio JI, Rodriguez JJ (2000) The patellofemoral joint in total knee arthroplasty: Is the design of the trochlea the critical factor? J Arthroplasty 15(4):424–429
Kuriyama S, Ishikawa M, Furu M, Ito H, Matsuda S (2014) Malrotated tibial component increases medial collateral ligament tension in total knee arthroplasty. J Orthop Res 32(12):1658–1666
Lemaire P, Pioletti DP, Meyer FM, Meuli R, Dorfl J, Leyvraz PF (1997) Tibial component positioning in total knee arthroplasty: bone coverage and extensor apparatus alignment. Knee Surg Sports Traumatol Arthrosc 5(4):251–257
Lutzner J, Kirschner S, Gunther KP, Harman MK (2012) Patients with no functional improvement after total knee arthroplasty show different kinematics. Int Orthop 36(9):1841–1847
Lutzner J, Krummenauer F, Gunther KP, Kirschner S (2010) Rotational alignment of the tibial component in total knee arthroplasty is better at the medial third of tibial tuberosity than at the medial border. BMC Musculoskelet Disord 11:57
Martin S, Saurez A, Ismaily S, Ashfaq K, Noble P, Incavo SJ (2014) Maximizing tibial coverage is detrimental to proper rotational alignment. Clin Orthop Relat Res 472(1):121–125
Matsuzaki T, Matsumoto T, Kubo S, Muratsu H, Matsushita T, Kawakami Y, Ishida K, Oka S, Kuroda R, Kurosaka M (2014) Tibial internal rotation is affected by lateral laxity in cruciate-retaining total knee arthroplasty: an intraoperative kinematic study using a navigation system and offset-type tensor. Knee Surg Sports Traumatol Arthrosc 22(3):615–620
Merican AM, Ghosh KM, Iranpour F, Deehan DJ, Amis AA (2011) The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19(9):1479–1487
Miyazaki Y, Nakamura T, Kogame K, Saito M, Yamamoto K, Suguro T (2011) Analysis of the kinematics of total knee prostheses with a medial pivot design. J Arthroplasty 26(7):1038–1044
Moran CG, Horton TC (2000) Total knee replacement: the joint of the decade. A successful operation, for which there’s a large unmet need. BMJ 320(7238):820
Nagamine R, Whiteside LA, White SE, McCarthy DS (1994) Patellar tracking after total knee arthroplasty. The effect of tibial tray malrotation and articular surface configuration. Clin Orthop Relat Res 304:262–271
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Bohler N, Labek G (2013) Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty 28(8):1329–1332
Steinbrück A, Schröder C, Woiczinski M, Fottner A, Müller PE, Jansson V (2013) Patellofemoral contact patterns before and after total knee arthroplasty: an in vitro measurement. Biomed Eng Online 12:58
Steinbrück A, Schröder C, Woiczinski M, Fottner A, Müller PE, Jansson V (2014) The effect of trochlea tilting on patellofemoral contact patterns after total knee arthroplasty: an in vitro study. Arch Orthop Trauma Surg 134(6):867–872
Steinbrück A, Schröder C, Woiczinski M, Müller T, Müller PE, Jansson V, Fottner A (2015) Influence of tibial rotation in total knee arthroplasty on knee kinematics and retropatellar pressure: an in vitro study. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3503-1
Steinbrück A, Woiczinski M, Weber P, Müller PE, Jansson V, Schröder C (2014) Posterior cruciate ligament balancing in total knee arthroplasty: a numerical study with a dynamic force controlled knee model. Biomed Eng Online 13:91
Stephen JM, Lumpaopong P, Dodds AL, Williams A, Amis AA (2015) The effect of tibial tuberosity medialization and lateralization on patellofemoral joint kinematics, contact mechanics, and stability. Am J Sports Med 43(1):186–194
van Kempen RW, Schimmel JJ, van Hellemondt GG, Vandenneucker H, Wymenga AB (2013) Reason for revision TKA predicts clinical outcome: prospective evaluation of 150 consecutive patients with 2-years followup. Clin Orthop Relat Res 471(7):2296–2302
Vince KG (2003) Why knees fail. J Arthroplasty 18(3 Suppl 1):39–44
Wagenaar FC, Koeter S, Anderson PG, Wymenga AB (2007) Conventional radiography cannot replace CT scanning in detecting tibial tubercle lateralisation. Knee 14(1):51–54
Wylde V, Learmonth I, Potter A, Bettinson K, Lingard E (2008) Patient-reported outcomes after fixed- versus mobile-bearing total knee replacement: a multi-centre randomised controlled trial using the Kinemax total knee replacement. J Bone Joint Surg Br 90(9):1172–1179
Zaffagnini S, Bignozzi S, Saffarini M, Colle F, Sharma B, Kinov PS, Marcacci M, Dejour D (2014) Comparison of stability and kinematics of the natural knee versus a PS TKA with a ‘third condyle’. Knee Surg Sports Traumatol Arthrosc 22(8):1778–1785
Zihlmann MS, Stacoff A, Romero J, Quervain IK, Stussi E (2005) Biomechanical background and clinical observations of rotational malalignment in TKA: literature review and consequences. Clin Biomech 20(7):661–668
Author information
Authors and Affiliations
Corresponding author
Additional information
Arnd Steinbrück and Andreas Fottner contributed equally to this work.
Rights and permissions
About this article
Cite this article
Steinbrück, A., Fottner, A., Schröder, C. et al. Influence of mediolateral tibial baseplate position in TKA on knee kinematics and retropatellar pressure. Knee Surg Sports Traumatol Arthrosc 25, 2602–2608 (2017). https://doi.org/10.1007/s00167-015-3843-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3843-x