Abstract
Purpose
Tibial acceleration during the pivot shift test is a potential quantitative parameter to evaluate rotational laxity of anterior cruciate ligament (ACL) insufficiency. However, clinical application of this measurement has not been fully examined. This study aimed to measure and compare tibial acceleration before and after ACL reconstruction (ACLR) in ACL-injured patients. We hypothesized tibial acceleration would be reduced by ACLR and tibial acceleration would be consistent in the same knee at different time points.
Methods
Seventy ACL-injured patients who underwent ACLR were enrolled. Tibial acceleration during the pivot shift test was measured using an electromagnetic measurement system before ALCR and at the second-look arthroscopy 1 year post-operatively. Tibial acceleration was compared to clinical grading and between ACL-injured/ACL-reconstructed and contralateral knees.
Results
Pre-operative tibial acceleration was increased stepwise with the increase in clinical grading (P < 0.01). Tibial acceleration in ACL-injured knee (1.9 ± 1.2 m/s2) was larger than that in the contralateral knee (0.8 ± 0.3 m/s2, P < 0.01), and reduced to 0.9 ± 0.3 m/s2 post-operatively (P < 0.01). There was no difference between ACL-reconstructed and contralateral knee (n.s.). Tibial acceleration in contralateral knees was consistent pre- and post-operatively (n.s.).
Conclusion
Tibial acceleration measurement demonstrated increased rotational laxity in ACL-injured knees and its reduction by ALCR. Additionally, consistent measurements were obtained in ACL-intact knees at different time points. Therefore, tibial acceleration during the pivot shift test could provide quantitative evaluation of rotational stability before and after ACL reconstruction.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pivot shift test [10, 11] is routinely performed to assess rotational laxity of the knee in a clinical setting and may also be used to detect residual rotational laxity in anterior cruciate ligament (ACL)-reconstructed knees in which anterior laxity has been successfully reduced. Owing to the clinical impact of the rotational knee laxity on knee function [20, 27] and long-term osteoarthritis [18], meticulous evaluation of the rotational laxity is highly desirable, especially for follow-up after ACL reconstruction.
Although several quantitative evaluation systems for the pivot shift test have been developed [5–8, 14, 16, 17, 21, 25, 26, 28–30, 32, 35], the clinical benefits of those systems have not been verified [31]. Tibial acceleration during the pivot shift test can be measured by a non-invasive system such as the electromagnetic system [14] or the accelerometer [4, 29, 30, 32], and was reported to have the best correlation to the clinical grading among several knee kinematics measurements [24]. In this context, the potential utility of the acceleration measurement for follow-up after treatment can be highly expected. The previous studies [14] indicated the quantitative measurement of tibial acceleration in the only ACL-deficient and ACL-intact knees using the electromagnetic system, but tibial acceleration of ACL-reconstructed knees has not been ever reported and is still unknown. Thus, the ability to detect differences in acceleration before and after surgical treatment should be confirmed, and consistent measurements should be achieved in the same knee at different time points. Therefore, the purpose of this study was to measure and compare tibial acceleration during the pivot shift test before and after ACL reconstruction in patients with ACL injury. We hypothesized that tibial acceleration during the pivot shift test would be reduced by ACL reconstruction and that tibial acceleration measurements would be consistent in the same knee at different time points.
Materials and methods
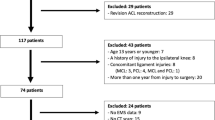
Patients with unilateral ACL injury who were scheduled to undergo ACL reconstructions between 2007 and 2011 in our hospital were prospectively enrolled in the study. Patients who had fractures, cartilage injuries, posterolateral corner injuries, and other knee ligament injuries, including medial collateral ligament and posterior cruciate ligament injuries in the ipsilateral or contralateral knee, were excluded. After obtaining informed consent for participation, a total of 70 patients (39 male/31 female, 28.4 ± 10.7 years old) were selected (Table 1). Informed consent was obtained from all individual participants included in the study.
Diagnosis of the ACL deficiency was made on the basis of clinical findings and magnetic resonance imaging (MRI), and was arthroscopically confirmed subsequently. ACL ruptures were categorized into either complete or partial tear. The diagnosis of partial ACL tears was made with a previously reported procedure [2]. Briefly, partial ACL tears were suspected during a physical examination in the outpatient clinic based on the presence of a hard endpoint or delayed hard endpoint during the Lachman test or a low-grade pivot shift test. MRI was also used as a diagnostic tool for partial ACL tears, as previously reported [36]. However, in the present study, the definitive diagnosis of partial ACL tears using MRI was difficult using our standard protocol; therefore, partial ACL tears were finally confirmed by an experienced surgeon using arthroscopic inspection during the reconstructive surgery. In these cases, an ACL augmentation procedure that preserved the remaining ACL bundle was performed for either the anteromedial bundle (AMB) or the posterolateral bundle (PLB). For patients with complete ACL tears, either anatomic single-bundle or double-bundle reconstruction was performed [9]. Consequently, 45 anatomic double-bundle reconstructions and 13 anatomic single-bundle reconstructions for ACL complete tears, and 12 augmentation procedures for ACL partial tears (2 AMB partial tears and 10 PLB partial tears) were performed. All patients followed the same post-operative programme. Jogging was permitted 4 months after surgery, with a gradual return to full sports activity, including competitive sports, 8 months after surgery [9].
The pivot shift test was performed, as described by Galway and MacIntosh [11], according to whom the hip was abducted and the knee was passively flexed from full extension with internal tibial torque and valgus stress applied manually to the knee. Two experienced surgeons were instructed to perform the pivot shift manoeuvres as similarly as possible before this study. Routine clinical grading of the pivot shift test was determined by the examiner according to the International Knee Documentation Committee (IKDC) forms: none (−), glide (+), clunk (++), or gross (+++) [13].
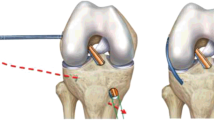
Tibial acceleration during the pivot shift test was measured using an electromagnetic device (Liberty, Polhemus, Colchester, VT, USA, Fig. 1a, b) as previously described [14, 19]. This system consists of a transmitter that produces an electromagnetic field and three electromagnetic receivers. Two of the receivers were firmly attached on the thigh and the calf with a plastic brace and were used to track the femoral and tibial motion, respectively. Each femoral and tibial coordinate system was configured based on the three-dimensional position data of anatomic landmarks that were digitized by the third receiver, providing six degree-of-freedom knee kinematics according to Grood and Suntay [12]. The electromagnetic device had a root-mean-square accuracy of 0.76 mm for position and 0.15° for orientation when it was used within 106 cm of a transmitter-to-receiver separation and when there was no interference from magnetic materials [33]. Knee kinematics data were acquired with 240 Hz during the pivot shift test, and the tibial acceleration was then calculated from the tibial anteroposterior translation over time. The peak acceleration for the tibial posterior shift, or reduction movement, was utilized as the representative value for the tibial acceleration during the pivot shift test [14]. The three times intra-examiner repeatability of the tibial acceleration measurement during pivot shift test was 0.2 m/s2 [14]. The quantitative measurement and manual clinical grading of the pivot shift test was repeated in both knees at the time of ACL reconstruction and second-look arthroscopy that was performed at the time of removal of the screw at 1 year after reconstructive surgery. All measurements were performed under general anaesthesia. There was no case of re-injury in the study during follow-up. The study was approved by the Institutional Review Board (IRB) in the hospital.
Statistical analysis
Statistical analysis was performed using a statistical software package (StatView 5.0, Abacus Concepts Inc., Berkeley, CA, USA). The one-way analysis of variance (ANOVA) was used to compare each value of tibial acceleration, and post hoc analysis was performed using Fisher’s protected least significance difference test. P value <0.05 was considered statistically significant. A priori power analysis showed that at least 64 subjects were required to compare the value among four groups using ANOVA with an effect size of 0.5, a power of 0.90, and an alpha error of 0.05.
Results
For the pre-operative clinical grading in the pivot shift test, 4 patients’ condition was classified as none (−), 30 patients’ as glide (+), 33 patients’ as clunk (++), and 3 patients’ as gross (+++). On the other hand, there were 68 patients whose condition was classified as none (−) and 2 patients whose condition as glide (+) at the 1-year follow-up (Table 2). Pre-operative tibial acceleration during the pivot shift test in each clinical grading was 0.9 ± 0.4, 1.3 ± 0.6, 2.2 ± 0.8, and 5.2 ± 2.7 m/s2, respectively, which was increased stepwise with the increase in clinical grading of the pivot shift test (P < 0.01, Fig. 2).
Prior to the ACL reconstruction, tibial acceleration during the pivot shift test was larger in the ACL-injured knee (1.9 ± 1.2 m/s2) than in the contralateral intact knee (0.8 ± 0.3 m/s2, P < 0.01). Meanwhile, ACL reconstruction significantly reduced tibial acceleration to 0.9 ± 0.3 m/s2 at the 1-year follow-up (P < 0.01), which was equivalent to that of the contralateral knee (n.s.). In addition, the acceleration measurement in the contralateral knees was consistent before ACL reconstruction and at the follow-up (0.8 ± 0.3 and 0.8 ± 0.3 m/s2, respectively, n.s.) (Table 3).
Discussion
The main findings of the present study were that larger rotational laxity in the ACL-deficient knee and its reduction to a normal level by ACL reconstruction were detected by measuring the tibial acceleration during the pivot shift test using the electromagnetic system. We demonstrated that rotational instability in the ACL-injured knees was reduced by ACL reconstruction. Additionally, consistent measurements were obtained in the ACL-intact knees at different time points, i.e. in pre- and post-operative assessments. Furthermore, tibial acceleration evaluated with the electromagnetic system was correlated with clinical grading of the pivot shift test similarly to previous reports [14], indicating the usefulness of the measurement of tibial acceleration.
Objective and meticulous assessment of the rotational laxity, or the pivot shift test, is eminently desirable to improve clinical care for patients with ACL injury. Meanwhile the result of the pivot shift test after ACL reconstruction is correlated with knee function, patient satisfaction [20, 27], and long-term osteoarthritis (OA) [18], and the clinical grading of the pivot shift test has been subjectively classified into only four grades of instability in a normal clinical setting. Over the last 10 years, tibial acceleration of the pivot shift test has been focused on because of its relationship to clinical grading [14, 24, 26, 30]. Labbe et al. [24] reported that the acceleration and velocity of the tibial translation were more related with clinical grading than with simple knee kinematics such as tibial translation and rotation, deepening the meaning of the current study findings.
Clinical impact and usability of the electromagnetic system for the pivot shift acceleration were appreciated in this study similarly to that reported in previous reports [14, 22]. A wide variety of biomechanical evaluations after ACL reconstruction have been conducted, from a highly controlled static test using a robotic system [38] to a dynamic functional test using radiostereometry (RSA) [37]. Although both evaluations can provide important feedback for the ACL treatment, these tests need extensive laboratory set-up and are not usable in the normal clinical setting. On the other hand, the pivot shift test is readily applicable in the clinical setting and could be a “bridge” between simple static biomechanical tests and functional dynamic kinematics tests [34]. In order to quantify the pivot shift test, several devices have been developed in addition to the electromagnetic system [6, 8, 14, 25], such as a navigation system [5, 7, 17, 26, 28, 35], an accelerometer [3, 4, 21, 29, 30, 32], and an image analysis using the iPad [16]. Kopf et al. [21] quantified the pivot shift phenomenon by using the accelerometer. Zaffagnini et al. [40] reported significant reductions after double-bundle ACL reconstruction regarding the posterior acceleration of tibial reduction during the pivot shift test (from 1600 ± 1200 to 450 ± 225 mm/s2, P < 0.05) [39], which supports our present findings. These reports and the present study indicate that acceleration could be one of the best key to quantify the pivot shift test. Moreover, some of these systems require rigid fixation with bone pins [3, 5, 7, 17, 26, 28, 32, 35], while other non-invasive systems including the electromagnetic system seem to be preferable for clinical use.
Even though the intra-examiner repeatability of the acceleration measurement was quite acceptable [14, 24], the acceleration was still susceptible to the difference of test manoeuvres across examiners [23]. Kuroda et al. [23] demonstrated that the Lachman test is performed in a similar fashion but has a wide variation in the amount of tibial translation across surgeons, while the pivot shift test has variability in performance of the manoeuvre but could possibly be measured reliably by the tibial translation of the pivot shift and/or its acceleration. Hoshino et al. [15] demonstrated that standardized manoeuvre of the pivot shift test provided a more consistent acceleration measurement. In the present study, it was verified that the tibial acceleration measurement was consistent at different time points and between two different surgeons who were advised to perform the test in the same manner. Therefore, the acceleration measurement with a standardized testing procedure could overcome the problem of the variation of the pivot shift test manoeuvre.
Despite the important findings in this study, there are several limitations. First, ACL reconstruction involved ACL augmentation as well as anatomic single- and double-bundle reconstructions. However, our main focus was to evaluate the clinical usability of the rotational laxity measurement between pre- and post-surgical treatment for the ACL-injured knees and not to compare the different surgical techniques. As the clinical effects of those ACL reconstruction techniques have already been established [1, 9], those reconstruction techniques can be similarly used as the standard effective ACL reconstruction procedures in the current study. Second, the post-operative evaluation was performed at 1 year after reconstructive surgery; thus the long-term results might be different from the present results. Again, this study did not aim to test the clinical outcome of some ACL reconstruction procedures. Thus, the long-term, or at least 2-year follow-up does not seem to be necessary for this study purpose. Moreover, in our clinical routine, the second-look arthroscopy was scheduled at the time of tibial screw removal around 1 year after surgery, and the comparable evaluation of the pivot shift test under general anaesthesia could only be acquired in that time frame. Third, during the manually provoked pivot shift test, the speed of the procedure, the angle of hip abduction, and the magnitude of force applied to the knee were not exactly equal in each test or among examiners. However, the pivot shift test was performed by two experienced surgeons who were advised and instructed to perform the test in a consistent manoeuvre. A previous report demonstrated that instruction of a standardized pivot shift test procedure to multiple examiners significantly reduced their testing variability [15]. The inter-examiner variability was reduced as much as possible. Fourth, there was observer bias at the time of acceleration measurement in this study. However, when the examiner performed acceleration measurement and clinical grading of the pivot shift test, the examiner did not know the results of the acceleration because the acceleration was calculated later in another place after the six degree-of-freedom knee kinematics data were acquired in the operation room. Thus, the observer bias was supposed to be minimal.
The clinical relevance of this study is that tibial acceleration during the pivot shift test measured by the EMS can provide quantitative evaluation of rotational stability before and after ACL reconstruction.
Conclusion
Quantitative evaluation of the pivot shift test was done by using the electromagnetic measurement system under general anaesthesia, and the results revealed that the rotational instability observed in ACL-injured knees was reduced by ACL reconstruction at the time of second-look arthroscopy. Additionally, consistent measurements were obtained in the ACL-intact knees at different time points, before and after surgery. Therefore, tibial acceleration during the pivot shift test could provide quantitative evaluation of rotational stability before and after ACL reconstruction.
References
Adachi N, Ochi M, Uchio Y, Sumen Y (2000) Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg 120(3–4):128–133
Araki D, Kuroda R, Matsushita T, Matsumoto T, Kubo S, Nagamune K, Kurosaka M (2013) Biomechanical analysis of the knee with partial anterior cruciate ligament disruption: quantitative evaluation using an electromagnetic measurement system. Arthroscopy 29(6):1053–1062
Asai S, Maeyama A, Hoshino Y, Goto B, Celentano U, Moriyama S, Smolinski P, Fu FH (2014) A comparison of dynamic rotational knee instability between anatomic single-bundle and over-the-top anterior cruciate ligament reconstruction using triaxial accelerometry. Knee Surg Sports Traumatol Arthrosc 22(5):972–978
Berruto M, Uboldi F, Gala L, Marelli B, Albisetti W (2013) Is triaxial accelerometer reliable in the evaluation and grading of knee pivot-shift phenomenon? Knee Surg Sports Traumatol Arthrosc 21(4):981–985
Bignozzi S, Zaffagnini S, Lopomo N, Fu FH, Irrgang JJ, Marcacci M (2010) Clinical relevance of static and dynamic tests after anatomical double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 18(1):37–42
Bull AMJ, Earnshaw PH, Smith A, Katchburian MV, Hassan ANA, Amis AA (2002) Intraoperative measurement of knee kinematics in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 84(7):1075–1081
Citak M, Suero EM, Rozell JC, Bosscher MR, Kuestermeyer J, Pearle AD (2011) A mechanized and standardized pivot shifter: technical description and first evaluation. Knee Surg Sports Traumatol Arthrosc 19(5):707–711
Engebretsen L, Wijdicks CA, Anderson CJ, Westerhaus B, LaPrade RF (2012) Evaluation of a simulated pivot shift test: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 20(4):698–702
Fujita N, Kuroda R, Matsumoto T, Yamaguchi M, Yagi M, Matsumoto A, Kubo S, Matsushita T, Hoshino Y, Nishimoto K, Araki D, Kurosaka M (2011) Comparison of the clinical outcome of double-bundle, anteromedial single-bundle, and posterolateral single-bundle anterior cruciate ligament reconstruction using hamstring tendon graft with minimum 2-year follow-up. Arthroscopy 27(7):906–913
Galway HR, Beaupre A, MacIntosh DL (1972) Pivot-shift: a clinical sign of symptomatic anterior cruciate ligament insufficiency. J Bone Joint Surg Br 54:763–764
Galway HR, MacIntosh DL (1980) The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res 147:45–50
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105(2):136–144
Hefti F, Muller W, Jakob RP, Staubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1(3–4):226–234
Hoshino Y, Kuroda R, Nagamune K, Yagi M, Mizuno K, Yamaguchi M, Muratsu H, Yoshiya S, Kurosaka M (2007) In vivo measurement of the pivot-shift test in the anterior cruciate ligament-deficient knee using an electromagnetic device. Am J Sports Med 35(7):1098–1104
Hoshino Y, Araujo P, Ahlden M, Moore CG, Kuroda R, Zaffagnini S, Karlsson J, Fu FH, Musahl V (2012) Standardized pivot shift test improves measurement accuracy. Knee Surg Sports Traumatol Arthrosc 20(4):732–736
Hoshino Y, Araujo P, Ahlden M, Samuelsson K, Muller B, Hofbauer M, Wolf MR, Irrgang JJ, Fu FH, Musahl V (2013) Quantitative evaluation of the pivot shift by image analysis using the iPad. Knee Surg Sports Traumatol Arthrosc 21(4):975–980
Ishibashi Y, Tsuda E, Yamamoto Y, Tsukada H, Toh S (2009) Navigation evaluation of the pivot-shift phenomenon during double-bundle anterior cruciate ligament reconstruction: is the posterolateral bundle more important? Arthroscopy 25(5):488–495
Jonsson H, Riklund-Ahlstrom K, Lind J (2004) Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand 75(5):594–599
Kitamura N, Yokota M, Kondo E, Miyatake S, Nagamune K, Yasuda K (2013) Biomechanical characteristics of 3 pivot-shift maneuvers for the anterior cruciate ligament-deficient knee: in vivo evaluation with an electromagnetic sensor system. Am J Sports Med 41(11):2500–2506
Kocher MS (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32(3):629–634
Kopf S, Kauert R, Halfpaap J, Jung T, Becker R (2012) A new quantitative method for pivot shift grading. Knee Surg Sports Traumatol Arthrosc 20(4):718–723
Kubo S, Muratsu H, Yoshiya S, Mizuno K, Kurosaka M (2007) Reliability and usefulness of a new in vivo measurement system of the pivot shift. Clin Orthop Relat Res 454:54–58
Kuroda R, Hoshino Y, Kubo S, Araki D, Oka S, Nagamune K, Kurosaka M (2012) Similarities and differences of diagnostic manual tests for anterior cruciate ligament insufficiency: a global survey and kinematics assessment. Am J Sports Med 40(1):91–99
Labbe DR, de Guise JA, Mezghani N, Godbout V, Grimard G, Baillargeon D, Lavigne P, Fernandes J, Ranger P, Hagemeister N (2010) Feature selection using a principal component analysis of the kinematics of the pivot shift phenomenon. J Biomech 43(16):3080–3084
Labbe DR, de Guise JA, Mezghani N, Godbout V, Grimard G, Baillargeon D, Lavigne P, Fernandes J, Ranger P, Hagemeister N (2011) Objective grading of the pivot shift phenomenon using a support vector machine approach. J Biomech 44(1):1–5
Lane CG, Warren RF, Stanford FC, Kendoff D, Pearle AD (2008) In vivo analysis of the pivot shift phenomenon during computer navigated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 16(5):487–492
Leitze Z, Losee RE, Jokl P, Johnson TR, Feagin JA (2005) Implications of the pivot shift in the ACL-deficient knee. Clin Orthop Relat Res 436:229–236
Lopomo N, Zaffagnini S, Bignozzi S, Visani A, Marcacci M (2010) Pivot-shift test: analysis and quantification of knee laxity parameters using a navigation system. J Orthop Res 28(2):164–169
Lopomo N, Signorelli C, Bonanzinga T, Marcheggiani Muccioli GM, Visani A, Zaffagnini S (2012) Quantitative assessment of pivot-shift using inertial sensors. Knee Surg Sports Traumatol Arthrosc 20(4):713–717
Lopomo N, Zaffagnini S, Signorelli C, Bignozzi S, Giordano G, Marcheggiani Muccioli GM, Visani A (2012) An original clinical methodology for non-invasive assessment of pivot-shift test. Comput Methods Biomech Biomed Eng 15(12):1323–1328
Lopomo N, Zaffagnini S, Amis AA (2013) Quantifying the pivot shift test: a systematic review. Knee Surg Sports Traumatol Arthrosc 21(4):767–783
Maeyama A, Hoshino Y, Debandi A, Kato Y, Saeki K, Asai S, Goto B, Smolinski P, Fu FH (2011) Evaluation of rotational instability in the anterior cruciate ligament deficient knee using triaxial accelerometer: a biomechanical model in porcine knees. Knee Surg Sports Traumatol Arthrosc 19(8):1233–1238
Milne AD, Chess DG, Johnson JA, King GJ (1996) Accuracy of an electromagnetic tracking device: a study of the optimal range and metal interference. J Biomech 29(6):791–793
Musahl V, Kopf S, Rabuck S, Becker R, van der Merwe W, Zaffagnini S, Fu FH, Karlsson J (2012) Rotatory knee laxity tests and the pivot shift as tools for ACL treatment algorithm. Knee Surg Sports Traumatol Arthrosc 20(4):793–800
Pearle AD, Kendoff D, Musahl V, Warren RF (2009) The pivot-shift phenomenon during computer-assisted anterior cruciate ligament reconstruction. J Bone Joint Surg Am 91(Suppl 1):115–118
Siebold R, Fu FH (2008) Assessment and augmentation of symptomatic anteromedial or posterolateral bundle tears of the anterior cruciate ligament. Arthroscopy 24(11):1289–1298
Tashman S, Collon D, Anderson K, Kolowich P, Anderst W (2004) Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med 32(4):975–983
Yamamoto Y (2004) Knee stability and graft function after anterior cruciate ligament reconstruction: a comparison of a lateral and an anatomical femoral tunnel placement. Am J Sports Med 32(8):1825–1832
Zaffagnini S, Marcheggiani Muccioli GM, Lopomo N, Signorelli C, Bonanzinga T, Musiani C, Vassilis P, Nitri M, Marcacci M (2012) Can the pivot-shift be eliminated by anatomic double-bundle anterior cruciate ligament reconstruction? Knee Surg Sports Traumatol Arthrosc 20(4):743–751
Zaffagnini S, Signorelli C, Lopomo N, Bonanzinga T, Marcheggiani Muccioli GM, Bignozzi S, Visani A, Marcacci M (2012) Anatomic double-bundle and over-the-top single-bundle with additional extra-articular tenodesis: an in vivo quantitative assessment of knee laxity in two different ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 20(1):153–159
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nagai, K., Hoshino, Y., Nishizawa, Y. et al. Quantitative comparison of the pivot shift test results before and after anterior cruciate ligament reconstruction by using the three-dimensional electromagnetic measurement system. Knee Surg Sports Traumatol Arthrosc 23, 2876–2881 (2015). https://doi.org/10.1007/s00167-015-3776-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3776-4