Abstract
Purpose
To evaluate patient-specific factors, including the mechanism of injury, time from the injury, activity level after the initial trauma, re-injury and body mass index (BMI), as risk factors for meniscal and chondral injuries accompanying anterior cruciate ligament (ACL) rupture.
Methods
A retrospective review of young adult patients with complete ACL rupture was performed between 2007 and 2011. The presence of meniscal tears and/or chondral injury, and the mechanism of injury, time from the injury, activity level after the initial trauma, re-injury and BMI were recorded. The data were analysed for associations between patient-specific factors and the prevalence of meniscal and chondral injuries.
Results
A total of 293 patients were included. Increasing time from the injury, active daily life and re-injury were risk factors associated with meniscal injuries (p < 0.05). Independent risk factors associated with meniscal injuries included active daily life (OR = 4.66, 95 % CI 2.21–9.86, p < 0.0001) and re-injury (OR = 7.68, 95 % CI 3.24–18.22, p < 0.0001). Contact injury, increasing time from the injury, active daily life and re-injury were risk factors associated with chondral injuries (p < 0.05). Independent risk factors associated with chondral injuries included contact injury (OR = 2.54, 95 % CI 1.27–5.10, p < 0.01), active daily life (OR = 2.62, 95 % CI 1.35–5.08, p < 0.01) and re-injury (OR = 4.18, 95 % CI 2.09–8.35, p < 0.001). The incidence of re-injury was associated with the activity level (p < 0.001) and increased with increasing time from the injury (r = −0.698, p < 0.001).
Conclusions
An increased risk of meniscal tear (especially medial meniscus) was strongly associated with an active daily life and re-injury. The combination of contact injury, active daily life and re-injury substantially increased the risk of cartilage injury. Patients with increasing time from the injury and active daily life exhibited a higher risk of re-injury, implying a higher prevalence of intra-articular damage.
Level of evidence
Cross-sectional study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anterior cruciate ligament (ACL) is the primary restraint to anterior tibial displacement [2]. The causes of ACL damage include non-contact injuries (NCI), for example due to deceleration, jumping and cutting manoeuvres, and contact injuries (CI) induced by external forces, such as those resulting from car accidents and high falls; the former mechanism is more common. At present, reconstruction surgery is the most widely accepted method for dealing with ACL rupture and has been proved to be safe and effective. However, it has been reported that the development of knee degeneration is significantly faster in patients with ACL rupture than in others [5]. Some studies have shown that accelerated knee degeneration may be related to meniscal tears and chondral lesions associated with ACL rupture [12, 19, 20]. Moreover, severe meniscal and chondral injuries can lead to traumatic arthritis and functional disturbances.
Anterior cruciate ligament (ACL) rupture is strongly associated with meniscal and chondral injuries [10, 15, 16]. In patients with ACL rupture, it has been reported that the incidence of intra-articular injuries increases with the time from the injury to reconstruction surgery [17, 20, 21]. With time, the rate of medial meniscal tears clearly increases, and the repair rate decreases [6]. Age and gender also influence the incidence of meniscal and cartilage injuries, with increasing age and male gender associated with a higher incidence [3, 16, 17, 19].
Other factors not fully considered in previous studies may also be relevant, such as body weight, recurrent episodes of knee instability, and the activity level after the initial injury. Dumont et al. [4] showed that in paediatric patients, body weight was strongly associated with medial meniscal tears. However, this study considered only the weight of the patient and did not take body size into account. In addition, there have been no reports regarding the influence of weight in adult patients. Another study reported that recurrent episodes of instability following ACL rupture contributed to meniscal and chondral injury, but no specific data were shown to directly support such effects [3]. Similarly, in a previous study, the activity level after the initial injury was not fully taken into account [21]. In most studies of adult patients, the age was not clearly defined, resulting in the recruitment of predominantly middle-aged and even elderly patients. It is well known that the elderly are more likely to suffer from knee degeneration than younger individuals, even without ACL rupture. In addition, none of these studies considered the influence of the initial mechanism of injury.
The purpose of the present study was to determine whether the prevalences of meniscal and chondral injuries accompanying ACL rupture are influenced by certain patient-specific factors that have yet to be fully assessed in previous studies, including the mechanism of injury, the time from the injury, the activity level, re-injury and body mass index (BMI). The hypothesis of this study was that several factors, including CI, increasing time from the injury, active daily life, explicit re-injury and higher BMI, would be associated with a greater number of meniscal tears and more severe articular cartilage lesions seen at the time of knee arthroscopy. An additional hypothesis was that ACL-deficient patients with a longer time from the injury and/or with an active daily life would have a greater frequency of re-injury.
Materials and methods
A retrospective chart review was performed at a single institution for all young patients (18–40 years old) with a complete ACL rupture between 2007 and 2011. All patients were confirmed to have complete ACL rupture by arthroscopic examination. Patients with other combined ligament injuries or with previous surgery were excluded from the study. In addition, patients with congenital knee deformities or recurrent arthralgia before the initial injury were also excluded. This study did not include patients with ACL avulsion fractures, irrespective of the site of the involvement.
Data collection
For each patient, data concerning the mechanism of injury, the time from the injury, the activity level after the initial trauma, re-injury and BMI were collected. The mechanism of injury was defined as the circumstance in which the injury occurred, for example sudden deceleration, wounding by a projectile or crushing by a heavy object. For analysis of the mechanism of injury, patients were divided into 2 groups: a NCI group (e.g., deceleration) and a CI group (e.g., falling or car accident). The time from the injury was calculated as the time from the date of the injury to the date of surgery; this was graded into 5 levels: acute stage (within 1 month), subacute stage (2–3 months), early stage (4–6 months), midterm stage (7–12 months) and late stage (longer than 12 months). The activity level was graded as active or inactive, according to the type of daily exercise undertaken after the initial injury; those patients regularly taking part in high-intensity sports (such as basketball, soccer, badminton and tennis) were defined as active, whereas those undertaking no exercise or only mild exercise (such as walking, jogging and low-speed cycling) were defined as inactive. Re-injury was defined as an explicit injury to the same knee introduced by joint instability after the initial injury and was recorded as “yes” or “no”, regardless of whether the injury occurred once or repeatedly; this approach was taken as few patients could accurately recall the exact number of re-injuries. For BMI analysis, patients were classified into 4 groups: low weight (BMI ≤20), normal (20–25), overweight (25–30) and obese (>30).
The presence of medial and/or lateral meniscal tears and of chondral lesions was confirmed and documented by two surgeons simultaneously. A full-thickness defect in the meniscus was considered a tear. The types and exact locations of the meniscal tears were not considered in order to simplify the study. Chondral lesions were graded using the Outerbridge classification [12] and documented in the surgery operative logs. If several chondral lesions were present, the grade for the most severe lesion was recorded; the exact site of the lesion was not taken into account (again, to simplify the study). This study was approved by the Institutional Review Board of West China Hospital, Sichuan University (ID 20120139).
Statistical analysis
Data analysis was performed using the SPSS for Windows v.14.0.0 statistical software program (SPSS Inc., Chicago, IL). The mechanism of injury, time from the injury, activity level, re-injury and BMI were analysed as independent variables, while the meniscal and cartilage injuries were analysed as dependent variables. The chi-square test was used to determine whether the mechanism of injury, time from the injury, activity level, re-injury and BMI were associated with the incidence and severity of meniscal and chondral injuries. Furthermore, the chi-square test was used to explore the relationship between the activity level and re-injury. Multifactor logistic regression was carried out to identify independent risk factors associated with meniscal and cartilage injuries. Associations were reported as odds ratios (ORs) with 95 % confidence intervals (CIs). Spearman’s rank correlation analysis and the trend chi-square test were conducted to investigate the relationship between time from the injury and re-injury. A value of p < 0.05 was considered to be indicative of statistical significance.
Results
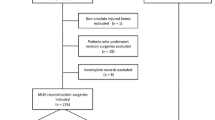
A total of 416 patients were confirmed by arthroscopic examination to have a complete ACL rupture between 2007 and 2011. Of these, 123 patients were excluded from the study: 61 with bone fractures or other ligament injuries, 2 with congenital knee deformities, 5 with knee diseases or recurrent arthralgia before the initial injury, 12 aged <18 years, and 43 aged more than 40 years. As a result, a total of 293 patients with complete information were identified and included in this study. All patients were diagnosed by one surgeon and treated by a medical team at a single centre. There were 228 (77.8 %) male and 65 (22.2 %) female patients, with a mean age of 28.6 years, and a mean time from the injury of 17.8 months.
With respect to meniscal injuries, there were statistically significant differences between groups in terms of the time from the injury, the activity level and re-injury (p < 0.05, Table 1). Increasing time from the injury, an active daily life and explicit re-injury were associated with a higher incidence of meniscal injury. Patients with an increased time from the injury were more likely to have a meniscal injury (p < 0.05), with the incidence ranging from 30/66 (45.5 %) to 83/98 (84.7 %). Notably, the incidence of medial meniscal injury ranged from 11/66 (16.7 %) in the acute group to 67/98 (68.4 %) in the late group (p < 0.05). Similarly, patients with an active daily life and/or explicit re-injury were also more likely to have a meniscal injury (p < 0.05): the incidence was 30/107 (37.4 %) in the inactive group versus 155/186 (83.3 %) in the active group; and 60/140 (42.9 %) in the non-re-injury group versus 135/153 (88.2 %) in the re-injury group. Multifactor logistic regression identified active daily life (OR = 4.66, 95 % CI 2.21–9.86, p < 0.0001) and re-injury (OR = 7.68, 95 % CI 3.24–18.22, p < 0.0001) as independent risk factors associated with meniscal injuries.
With respect to cartilage injuries, there were statistically significant differences between groups in terms of the mechanism of injury, the time from the injury, the activity level and re-injury (p < 0.05, Table 1). CI, increasing time from the injury, an active daily life and explicit re-injury were associated with an increased incidence and severity of cartilage injury. Patients with CI were more likely to have a cartilage injury than those with NCI (p < 0.05); the respective incidences were 142/224 (63.4 %) and 53/69 (76.8 %). Similarly, patients with an increased time from the injury were more likely to have a cartilage injury (p < 0.05), with the incidence ranging from 28/66 (42.4 %) to 86/98 (87.8 %). Furthermore, the injury tended to be more severe in patients with an increased time from the injury, with the incidence of Grade III and IV lesions ranging from 0 in the acute group to 24/98 (24.5 %) in the late group (p < 0.05). Moreover, patients with an active daily life and explicit re-injury were more likely to have cartilage lesions (p < 0.05): the incidence was 45/107 (42.1 %) in the inactive group versus 150/186 (80.6 %) in the active group; and 65/140 (46.4 %) in the non-re-injury group versus 130/153 (85 %) in the re-injury group. Multifactor logistic regression identified the following independent risk factors associated with cartilage injuries: CI (OR = 2.54, 95 % CI = 1.27–5.10, p < 0.01), active daily life (OR = 2.62, 95 % CI = 1.35–5.08, p < 0.01) and explicit re-injury (OR = 4.18, 95 % CI = 2.09–8.35, p < 0.001).
The active group had a higher incidence of re-injury than the inactive group (p < 0.0001, Table 2), with a relative risk (RR) value of 7.5. There was a statistical correlation between the time from the injury and re-injury (r = −0.698, p < 0.001). Moreover, it was found that patients with a time from the injury of longer than a month were more likely to suffer from instability re-injuries: the RR values of re-injury were 19.9 for the early group and 29.3 for the late group, when compared with the acute group.
Discussion
The most important finding of this study was that patients with an increased time from the injury and/or with an active daily life had a higher incidence of re-injury, which may have induced severe meniscal and chondral injuries. ACL injuries among young people are most commonly introduced by high-intensity sports such as football, skiing and gymnastics [9, 18]. However, with the increasing use of machinery, ACL injuries caused by CI, such as car accidents, are becoming more common. Our results revealed that there were more patients in the NCI group (224 cases, 76.5 %) than in the CI group (69 cases, 23.5 %). However, many patients with CI were excluded from the study due to the presence of other ligament injuries or bone fractures. Therefore, the actual number of cases in the CI group may have been much higher than that determined in our study.
The two main underlying causes of intra-operatively observed meniscal and cartilage injuries are age-related joint degeneration and intra-articular injury associated with ACL rupture. The primary focus of this study was on the latter. Since older patients are generally more likely to suffer from meniscal and chondral injuries arising from joint degeneration, this study excluded patients over 40 years of age in order to minimize interference from confounding factors. The treatment of children with ACL rupture differs greatly from that of adults because of the immaturity of their bones, and hence, patients under 18 years of age were also excluded.
With regard to the mechanism of injury, there were no statistically significant differences between groups in the incidence of meniscal tears, implying that meniscal injuries are only associated with the body position and direction of the force at the time of the injury, and not with the cause (CI or NCI). However, with regard to chondral lesions, the incidence and severity in the CI group was significantly higher than that in the NCI group. This suggests that chondral lesions are more likely following the exertion of injurious forces through direct contact.
Long-term studies have demonstrated a significant increase in the rate of damage to the menisci and articular cartilage with increasing time from the injury [14, 19]. In the acute stage (within 1 month after the injury), patients with ACL ruptures tend to avoid vigorous exercise because of knee swelling and pain, leading to a relatively low risk of re-injury. With extension of the time from the injury, daily exercise is gradually restored, and the risk of re-injury may rapidly increase accordingly. The medial meniscus is broader and larger than the lateral meniscus, and the posterior horn of the former is thicker than that of the latter. As a result, the rate of medial meniscal tears in patients with re-injury is higher than that in patients without re-injury, and this is especially the case for posterior horn tears [1, 13, 15, 21]. In contrast, the incidence of lateral meniscal tears is relatively stable in the various stages [3, 7, 11], implying that lateral meniscal tears alone typically emerge in the initial stage of the injury, and that subsequent re-injury leads to tears in the medial part or both sides of the meniscus. This is consistent with the findings of Chhadia et al. [3]. Similarly, the risk of chondral lesions was significantly higher in the re-injury group than in the non-re-injury group, possibly due to recurrent abrasion of the joint surfaces induced by knee instability.
The patients in the present study differed greatly in terms of their activity levels after the initial trauma. Based on our experiences, we considered those who regularly undertook vigorous exercise with a high requirement on the knee joint, such as basketball, soccer, badminton and tennis, as active, while those participating in only mild exercise were regarded as inactive. There was a significant difference between the active and inactive groups in terms of the incidence of re-injury, with the former having a notably higher incidence of re-injury. In addition, the two groups differed significantly in terms of the risk of meniscal tears. It is possible that vigorous activities may have led to a far higher rate of re-injury, followed by more meniscal tears. Moreover, the results indicated that there was a significant difference between active and inactive groups in terms of the risk of cartilage injuries. This implies that excessive exercise after injury may introduce more chondral lesions or increase the severity of the existing lesions.
Body mass index (BMI) is an important index that has been used widely in many studies. However, with respect to ACL injury, the reports to date have focused mainly on paediatric body weight, and none have considered adult body weight or BMI [4, 8, 22]. Our investigation of the relevance of BMI in adult patients with ACL injury thus provides novel insights. We found that the various BMI groups did not differ significantly in terms of the risks of meniscal and cartilage injuries, implying that BMI may not be important to the degeneration of ACL-deficient knees. This finding was contrary to our original assumption that, in general, patients with a higher weight would be more likely to suffer from knee degeneration, with this being the main reason why overweight patients with osteoarthritis are asked to lose weight. Our data indicate that degeneration secondary to ACL rupture may not be the same as age-related joint degeneration. One possible explanation for our observations is that overweight patients may exercise less than those with lower BMIs, such that the actual joint loads of overweight patients are not higher than those of patients with lower BMIs.
To the best of our knowledge, this is the first study to demonstrate a relationship between re-injury and meniscal or cartilage injuries in ACL-insufficient knees. Moreover, meniscal or cartilage injuries were found to be associated with the time from the injury, the activity level and re-injury. Treating physicians should be aware that patients with increased time from the injury and an active daily life may have a higher risk of re-injury, which may imply a higher prevalence of intra-articular injury. Our findings suggest that ACL injuries may need medical intervention as early as possible. Within 1 month after the initial trauma, there may be less secondary damage to the meniscus and cartilage, allowing patients to achieve better functional stability that slows joint degeneration.
This study has some limitations that are inherent to a retrospective review. Some data, such as the date of the initial trauma and the types of exercise, were self-reported, and this may have introduced some errors. The BMI was collected upon admission, and continuous changes in BMI were not taken into account. Time intervals were selected as an intuitive demarcation that yielded reasonable sample sizes. Another limitation was that the time of the re-injury was not considered. In addition, although attempts were made to control for potential bias, the presence of meniscal and chondral injuries before ACL rupture could not be completely excluded. A large sample size would allow for a more detailed analysis of re-injury. An additional limitation was that patients with a complete rupture of the ACL in our series were subjected to an arthroscopic examination; this could have introduced a selection bias by excluding patients without arthroscopic examination.
Conclusion
Anterior cruciate ligament (ACL) rupture may introduce serious meniscal and cartilage injuries that can lead to accelerated knee degeneration. The findings of this study, focusing on young adult patients, indicated that an increased risk of re-injury was strongly associated with an increased time from the injury and an active daily life. An increased risk of meniscal tears (especially in the medial meniscus) was strongly associated with an active daily life and re-injury. Similarly, the combination of CI, active daily life and re-injury substantially increased the risk of cartilage injury. Physicians should consider the possibility of meniscal and chondral injuries when treating an ACL-insufficient knee in a patient with a longer time from the injury and an active daily life.
References
Bernstein J (2011) Early versus delayed reconstruction of the anterior cruciate ligament: a decision analysis approach. J Bone Joint Surg Am 93:e48
Butler DL, Kappa Delta Award paper (1989) Anterior cruciate ligament: its normal response and replacement. J Orthop Res 7:910–921
Chhadia AM, Inacio MC, Maletis GB, Csintalan RP, Davis BR, Funahashi TT (2011) Are meniscus and cartilage injuries related to time to anterior cruciate ligament reconstruction? Am J Sports Med 39:1894–1899
Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL (2012) Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med 40:2128–2133
Fithian DC, Paxton LW, Goltz DH (2002) Fate of the anterior cruciate ligament injured knee. Orthop Clin N Am 33:621–636
Fok AW, Yau WP (2013) Delay in ACL reconstruction is associated with more severe and painful meniscal and chondral injuries. Knee Surg Sports Traumatol Arthrosc 21:928–933
Gadeyne S, Besse JL, Galand-Desme S, Lerat JL, Moyen B (2006) Analysis of meniscal lesions accompanying anterior cruciate ligament tears: a retrospective analysis of 156 patients. Rev Chir Orthop Reparatrice Appar Mot 92:448–454
Granan LP, Bahr R, Lie SA, Engebretsen L (2009) Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian National Knee Ligament Registry. Am J Sports Med 37:955–961
Hootman JM, Dick R, Agel J (2007) Epidemiology of collegiate injuries for 15 sports: summary and recommendations of injury prevention initiatives. J Athl Train 42:311–319
Kaeding CC, Pedroza AD, Parker RD, Spindler KP, McCarty EC, Andrish JT (2005) Intra-articular findings in the reconstructed multiligament-injured knee. Arthroscopy 4:424–430
Keene GC, Bickerstaff D, Rae PJ, Paterson RS (1993) The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am J Sports Med 21:672–679
Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS (2008) Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 16:442–448
Lawrence JT, Argawal N, Ganley TJ (2011) Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med 39:2582–2587
Levy BA (2010) Is early reconstruction necessary for all anterior cruciate ligament tears? N Engl J Med 363:386–388
Maffulli N, Binfield PM, King JB (2003) Articular cartilage lesions in the symptomatic anterior cruciate ligament-deficient knee. Arthroscopy 19:685–690
O’Connor DP, Laughlin MS, Woods GW (2005) Factors related to additional knee injuries after anterior cruciate ligament injury. Arthroscopy 21:431–438
Piasecki DP, Spindler KP, Warren TA, Andrish JT, Parker RD (2003) Intraarticular injuries associated with anterior cruciate ligament tear: findings at ligament reconstruction in high school and recreational athletes. An analysis of sex-based differences. Am J Sports Med 31:601–605
Pujol N, Bianchi MP, Chambat P (2007) The incidence of anterior cruciate ligament injuries among competitive alpine skiers: a 25-year investigation. Am J Sports Med 35:1070–1074
Salata MJ, Gibbs AE, Sekiya JK (2010) A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med 38:1907–1916
Slauterbeck JR, Kousa P, Clifton BC et al (2009) Geographic mapping of meniscus and cartilage lesions associated with anterior cruciate ligament injuries. J Bone Joint Surg Am 91:2094–2103
Tandogan RN, Taser O, Kayaalp A, Taskiran E, Pinar H, Alparslan B, Alturfan A (2004) Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc 12:262–270
Yüksel HY, Erkan S, Uzun M (2006) The evaluation of intraarticular lesions accompanying ACL ruptures in military personnel who elected not to restrict their daily activities: the effect of age and time from injury. Knee Surg Sports Traumatol Arthrosc 14:1139–1147
Conflict of interest
No benefits or funds were received in support of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, G., Tang, X., Li, Q. et al. The evaluation of patient-specific factors associated with meniscal and chondral injuries accompanying ACL rupture in young adult patients. Knee Surg Sports Traumatol Arthrosc 23, 792–798 (2015). https://doi.org/10.1007/s00167-013-2718-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2718-2