Abstract
The paper describes the concepts of primary and secondary restraints to knee joint stability and explains systematically how the tibia is stabilised against translational forces and rotational torques in different directions and axes, and how those vary across the arc of flexion–extension. It also shows how the menisci act to stabilise the knee, in addition to load carrying across the joint. It compares the properties of the natural stabilising structures with the strength and stiffness of autogenous tissue grafts and relates those strengths to the strength of graft fixation devices. A good understanding of the biomechanical behaviour of these various structures in the knee will help the surgeon in the assessment and treatment of single and multi-ligament injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The kinematics of the knee joint is controlled by muscles and ligaments: active and passive stabilisers, respectively. These structures guide the motion and resist unwanted displacements and rotations between the bones. This review will concentrate on the passive stability afforded to the knee by the ligaments and joint capsule. When ligaments are stretched, the tensile forces produced in them keep the joint stable. This means that ligamentous injuries can cause mechanical instability which, in turn, can trigger the development of osteoarthritis (OA) due to the altered loading experienced in the joint during activities of daily living (ADLs). Anatomical and tension-free surgical reconstruction of these injuries is therefore vital and the biomechanics must be correctly understood to achieve good outcomes. The literature is dominated by studies of anterior cruciate ligament (ACL) injury and its reconstruction, but there are many other soft tissue injuries that can occur in the knee, including multi-ligament injuries. The level of restraint that a ligament provides to the knee joint can be divided into two types: primary and secondary. Primary restraints are aligned such that they are well able to resist translations or rotations in particular directions; e.g. the ACL is a primary restraint to anterior drawer of the tibia. Secondary restraints can also resist motion but are less well aligned; e.g. the medial collateral ligament also resists anterior tibial drawer. Any surgical reconstruction of these restraints must be considerate of both types to efficiently restore joint kinematics following injury, partly because unrepaired damage to one ligament will usually allow abnormally large forces to fall onto other ligaments, and that may, in turn, lead to chronic stretching out and some recurrence of instability.
Knee laxity defined
Measurements or assessments of laxity at the knee are usually describing how the proximal tibia can be moved, away from its normal equilibrium position, in relation to the distal femur. Laxity refers to the knee’s ability to translate or rotate in a particular direction, and can be measured either as the translation or the rotation produced by an applied force or torque, or the force or torque required to translate or rotate the knee by a certain amount. The knee can move in six degrees of freedom (DoF)—three translations and three rotations [14]. In the clinic, knee instability is a subjective symptom which disables the patient, such as ‘giving-way’, but instability also can have a defined meaning in engineering terms, which refers to increased joint laxity for a given displacing load in one or more of these directions due to pathology or injury.
The biomechanics of clinical assessment
Clinical assessment is used prior to surgery to check for increases in knee laxity, helping to diagnose ligament injuries, and after surgical intervention in order to evaluate the success of reconstruction procedures. It is vital that the correct type of test is chosen for the suspected injury(ies). There are two broad types of test: ‘static’, which is uniaxial, and ‘dynamic,’ which tests the knee in more than one direction [41].
Static testing
Static clinical tests are quick, simple and easy to perform consistently by different surgeons across different patients. However, they must be used with caution—there is always more than one restraint in any particular direction being tested (primary and secondary; Fig. 1) so it can be difficult to isolate the structure(s) that has been injured. In the case of the Lachman test, in an ACL-deficient knee, care must be taken not to overload the secondary restraint (the superficial MCL; sMCL) during the test. There is a plethora of static assessments available to the clinician, discussed further in the next paper.
Primary and secondary restraints. In this example, it can be seen that the ACL, the primary restraint to anterior translation of the tibia, is well aligned to an anterior drawer force. In the case of an injured or absent ACL, the superficial MCL (sMCL) will resist the same force, but it must be loaded to a much higher level to resist the anterior translation load because it is less well suited to this role (shown by the direction and length of the force vectors). The primary restraint is stretched proportionally more than the secondary restraint, so it is also more likely to be ruptured
Dynamic testing
Dynamic clinical assessment aims to mimic clinical behaviour, examining the knee’s laxity in more than one direction. It can be more powerful than simple static assessment, but it is less well controlled than static testing, tending to be more subjective, depending on how the clinician performs and interprets the test [5]. The best known of these tests is the ‘pivot-shift’ which assesses ACL injury and anterolateral laxity in the knee. This test has been criticised for being very surgeon subjective (in both its procedure and interpretation), but is accepted as providing a closer correlation with the clinical symptoms of dynamic instability (‘giving-way’) than do the static laxity tests. Work is being done to better standardise the pivot-shift technique and quantify its outcome [18, 31, 42].
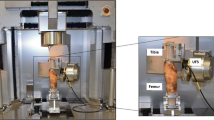
Ideally, all six DoF of the knee would be assessed for proper diagnosis of multi-ligament injuries in the clinical setting, with quantification of primary and secondary motions, as they can be in the laboratory [22, 23, 37, 43] (Fig. 2), at multiple angles of knee flexion. This is obviously very difficult to achieve without unacceptable invasiveness, so the above tests must be used with caution and in combination with each other to achieve a proper diagnosis.
The clinical relevance of mechanical and structural properties of ligament
Understanding the mechanical and structural properties of ligamentous tissue is important in order to properly appreciate how they behave when loaded in the knee during ADLs and how to best to reconstruct them when things go wrong. The primary role of ligaments is to transmit tensile forces along their length and so biomechanical testing of these soft tissues is usually done uniaxially. One can either assess the structural properties of the bone–ligament–bone complex, e.g. the femur–ACL–tibia, or the mechanical properties of the ligament tissue on its own. The latter can be difficult to measure for ligaments, especially the ACL which has an extremely short intra-articular portion. One must consider the material properties when choosing a graft for reconstruction and fixation method (Table 1). However, the ultimate load of the bone fixation has been shown to be the weakest link in ligament reconstruction, generally yielding at below 1800 N of force [1, 24, 45]. Initial fixation of grafts is critical so that there can be adequate healing of the graft to the bone at each end, and no slippage of the graft from its fixation under the cyclic tensile loads imposed by rehabilitation.
The cruciate ligaments
The cruciate ligaments are sometimes described as being two of the links in a mechanism called a four-bar linkage, with the knee joint’s path of motion determined by the location of the insertions of the linkages and their lengths. This single path of motion only accounts for sagittal knee translation and does not take into account the stretching or slackening of ligaments during knee flexion–extension, any component of motion out of the sagittal plane (such as tibial internal–external rotation), and the inherent laxity that is normal in a knee. In addition, it ignores the fact that one of the main functions of the knee is to cope with differing joint kinematics caused by changing muscle actions as we walk and run across diverse terrains.
Functional biomechanics
The ACL is the primary restraint to anterior translation of the tibia and prevents hyperextension of the knee. It also controls rotation in early flexion (the ‘screw-home’ mechanism [16]). The ACL is generally considered to consist of two main bundles of fibres: the anteromedial and the posterolateral bundles.
The posterior cruciate ligament (PCL) is the primary restraint to posterior translation of the tibia. It also consists of two bundles: anterolateral and posteromedial. While the posteromedial PCL is tight, the anterolateral PCL is slack in extension and vice versa in the flexed knee [47]. It also resists internal rotation of the knee in deep flexion.
The cruciate ligaments provide most of the resistance to anterior–posterior drawer translations of the knee, controlling its mechanical stability across the full flexion cycle; the secondary structures provide minimal resistance to these movements. This means that cruciate ligament injury leads to a high level of altered joint function and, in turn, the possibility of early-onset OA.
The biomechanics of cruciate ligament injury and reconstruction
ACL
There is a long, somewhat cyclical, history of ACL reconstruction research. The information available in the literature and the choices to be made preceding reconstruction could be baffling. It is generally believed that there is a high prevalence of knee OA in people who have injured their ACL; this, combined with the high incidence of ACL injury [55], explains the wealth of ACL research in the literature.
The initial question after ACL injury might be whether surgery is required at all. There is some evidence to suggest that conservative treatment for ACL injury (physiotherapy, bracing of the knee) can give acceptable results in lower-demand patients [30]. It might also be considered whether the damage to the ligament is repairable. It is sometimes possible to repair a torn ACL, but care must be taken; has the ligament retained its mechanical properties—i.e. is the ligamentous tissue still elastic in nature, or may the scarred tissue be vulnerable to creep elongation, which results in ‘stretching-out’?
When reconstructing a rupture too severe to be repaired, there are several key decisions to be made by the surgeon that could affect the biomechanics of the ACL-reconstructed knee. Should the reconstruction be single bundle or double bundle [12], for example? There is some evidence to suggest that the more technically demanding double-bundle procedure leads to a more stable knee, as measured by clinical assessment and in laboratory studies [23, 29, 54]; it may also have a lower revision rate, but it is still unclear whether the number of bundles has a long-term clinical effect. The location of the femoral and tibial tunnels will also affect the kinematic outcome of the procedure [21, 49]. The type of graft is another decision that must be made: autograft, allograft, xenograft and synthetic graft are all options. Autografts are the most commonly used and are usually hamstrings tendon or bone–patellar tendon–bone (BPTB). There is some evidence that suggests a BPTB graft leads to a more stable knee after reconstruction and a lower revision rate, but there is insufficient evidence to conclude which is better in terms of long-term functional performance and OA progression [20, 33, 38]. The alternatives to autogenous tissue grafts are usually considered in situations where there is a lack of availability of autogenous grafts, such as with multiple ligaments needing to be reconstructed, or in revision surgery. Finally, graft fixation method must also be decided upon: the literature includes many studies of graft fixation strength, but this interest has passed in the light of reliability of modern reconstruction methods, where failure is most commonly associated with malpositioned graft tunnels.
PCL
A search on PubMed reveals around five times as many articles relating to the ACL than the PCL. This may be because the PCL is injured less frequently than the ACL, but might also be because a PCL injury can be harder to diagnose or be less disabling. However, the PCL is critical for normal kinematic function of the knee, and although many patients may not suffer symptomatic instability acutely, longer-term knee degeneration suggests that such injuries should be accurately diagnosed and treated [51]. As with ACL reconstruction, there is a choice of single- or double-bundle procedures, with the single-bundle procedure usually replacing the anterolateral bundle, because that is the strongest part of the PCL [46] and is the dominant restraint across the arc of knee flexion. It has been demonstrated in the laboratory that the double-bundle reconstruction is biomechanically superior, leading to a more stable knee than the single-bundle procedure, in both posterior drawer and internal and external rotation [58], although superior clinical performance has not yet been demonstrated, mainly due to a lack of robust clinical studies [44].
The lateral aspect of the knee
The anterolateral structures
There has been a recent flurry of interest in the anterolateral structures, and the anterolateral ligament, in particular, in the academic literature and the mainstream media [8, 9, 11, 13, 40, 57]. But the idea of using anterolateral constructs around the knee to help to control rotatory laxity is not a new concept. Extra-articular tenodeses to treat rotatory instability after ACL injury have been described in the literature for decades [6, 32].
Biomechanically, it makes a great deal of sense that some kind of lateral, extra-articular structure is responsible for controlling the rotational laxity of the knee, rather than the centrally placed ACL, with one analogy being that of trying to stop a spinning wheel by gripping it on its peripheral rim, as opposed to via its central hub [2]. It follows that damage to these structure(s) should be repaired to restore that rotatory laxity. However, anterolateral tenodeses fell from use because of a perception that they were associated with later degenerative changes in the lateral compartment of the knee, but much of that evidence was collected from an era prior to modern methods of intra-articular ACL reconstruction, or treatment post-surgery, and there has been a recent increase in interest in the idea of anterolateral reconstructions. More biomechanical evidence is required to determine which structures are responsible for rotatory stability and how best to reconstruct them.
The iliotibial band
The iliotibial band (ITB) is a long band of fascia lata that originates at the gluteus maximus and passes over the lateral epicondyle of the femur to Gerdy’s tubercle. Because it also attaches onto to the distal femur and has fibres that connect to the patella, it plays a role in controlling varus and internal rotation of the knee [35], and thus has a role in the mechanism of the pivot shift [34], as well as ITB tension causing patella lateral tilt and reduced lateral stability [36].
The posterolateral knee
Up to 28, separate structures have been found in the posterolateral knee [25]. The three main ligamentous structures are the lateral collateral ligament (LCL), the popliteus tendon and the popliteofibular ligament (PFL).
The LCL controls varus rotation between extension and 30° flexion [50] and then starts to slacken in deeper flexion [53]. The popliteus muscle–tendon unit is a primary restraint to external rotation of the tibia and also contributes to anterior translational and varus rotational stability in early flexion [28]. The PFL connects the popliteal tendon to the head of the fibula [26] and thus forms a direct passive link from the femur to the head of the fibula. It is a secondary restraint to posterior translation and varus and external rotations [56]. It is taut when the LCL is slack in deeper flexion [53].
It can be seen that these structures, in combination, play an important role in controlling knee stability. Posterolateral knee injuries should not be ignored; chronic cases might even lead to reconstructions of the cruciate ligaments becoming overloaded and failing [25, 37].
The medial aspect of the knee
Medial collateral ligament (MCL)
The MCL can be split into the deep (dMCL) and superficial (sMCL) bands. The dMCL is connected to the medial meniscus and can itself be thought of as two parts: meniscotibial and meniscofemoral. It prevents valgus rotations and internal rotation when the knee is flexed and is also a secondary restraint to anterior tibial drawer and external rotation in early flexion. The sMCL is the primary restraint to valgus and external rotation and is the strongest component of the MCL complex [48]. Due to its much longer fibres, the sMCL will tend to remain intact, with the dMCL rupturing first, because the shorter dMCL fibres are subjected to a greater per cent elongation (tensile strain) (Fig. 3).
Posterior oblique ligament (POL)
The POL is a thickening of the posteromedial joint capsule [19]. It helps to stabilise the knee in internal rotation in extension and early flexion, but slackens with flexion. Its proximal attachment is around the adductor tubercle of the femur, from which its fibres pass in a posterodistal direction to the tibia.
Oblique popliteal ligament (OPL)
The OPL is the largest ligamentous structure in the posterior capsular part of the knee [27] and prevents hyperextension [39]. It connects the distal end of the semimembranosus muscle to the osseous or cartilaginous fabella and the lateral aspect of the PCL facet, just distal to the posterior root of the lateral meniscus [27].
The menisci and associated ligaments
Although not actually ligaments, the menisci fulfil a role of secondary translational and rotational restraint, partly because they insert into the tibia and are connected to the femur via several ligament structures, and also because they increase the congruity of the tibiofemoral joint and have limits to their mobility, particularly the medial meniscus. Menisci are secondary restraints to anterior drawer, via meniscocapsular and meniscotibial attachments such as the dMCL [3], and the meniscofemoral ligaments are PCL agonists and act as secondary restraints to tibial posterior drawer [15]. There is some evidence to suggest that early onset of OA is due to the meniscal injury which may occur in conjunction with an ACL tear, rather than an isolated ACL injury [7]. Lesions of the posterior aspect of the medial meniscus also occur alongside many ACL injuries, and repair of such lesions may be beneficial in restoring normal knee kinematics [52].
Muscular restraints
The muscles around the knee are active restraints, and they are the dynamic stabilisers that provide the loading to move the joint and are the reason that loads in the knee joint reach many times that of a person’s body weight during certain activities. The quadriceps, hamstrings and gastrocnemius muscles control both flexion/extension and internal–external rotation. However, they also cause anterior–posterior shear forces that are resisted primarily by the cruciate ligaments. Conversely, training the muscles may increase ‘dynamic stability’ and reduce the symptoms arising from ligament damage [4].
Conclusions
Table 2 demonstrates just how complex the six-DoF movement of the knee joint is and how multi-ligament interactions keep the joint stable in multiple positions and activities. There is a wealth of information in the literature about soft tissue knee injuries and their repair and reconstruction. An appreciation of the contribution of the various structures to the normal biomechanics of the knee will help the surgeon to choose a logical approach to reconstructing single and multi-ligament injuries.
References
Aga C, Rasmussen MT, Smith SD, Jansson KS, LaPrade RF, Engebretsen L, Wijdicks CA (2013) Biomechanical comparison of interference screws and combination screw and sheath devices for soft tissue anterior cruciate ligament reconstruction on the tibial side. Am J Sports Med 41(4):841–848
Andrews JR, Carson WGJ (1987) The role of extra-articular anterior cruciate ligament stabilization. In: Jackson DW, Drez DJ (eds) The anterior cruciate deficient knee. New concepts in ligament repair. CV Mosby, St. Louis, pp 168–192
Arno S, Hadley S, Campbell KA, Bell CP, Hall M, Beltran LS, Recht MP, Sherman OH, Walker PS (2013) The effect of arthroscopic partial medial meniscectomy on tibiofemoral stability. Am J Sports Med 41(1):73–79
Barcellona MG, Morrissey MC, Milligan P, Amis AA (2014) The effect of thigh muscle activity on anterior knee laxity in the uninjured and anterior cruciate ligament-injured knee. Knee Surg Sports Traumatol Arthrosc 22(11):2821–2829
Bull AM, Earnshaw PH, Smith A, Katchburian MV, Hassan AN, Amis AA (2002) Intraoperative measurement of knee kinematics in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 84(7):1075–1081
Carson W Jr (1985) Extra-articular reconstruction of the anterior cruciate ligament: lateral procedures. Orthop Clin N Am 16(2):191–211
Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P (2012) Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc 21(9):1967–1976
Claes S, Luyckx T, Vereecke E, Bellemans J (2014) The Segond fracture: a bony injury of the anterolateral ligament of the knee. Arthroscopy 30(11):1475–1482
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223(4):321–328
Cooper DE, Deng XH, Burstein AL, Warren RF (1993) The strength of the central third patellar tendon graft: a biomechanical study. Am J Sports Med 21(6):818–824
Cruells Vieira EL, Vieira EÁ, Teixeira da Silva R, dos Santos Berlfein PA, Abdalla RJ, Cohen M (2007) An anatomic study of the iliotibial tract. Arthroscopy 23(3):269–274
Desai N, Björnsson H, Musahl V, Bhandari M, Petzold M, Fu F, Samuelsson K (2014) Anatomic single- versus double-bundle ACL reconstruction: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 22(5):1009–1023
Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA (2014) The anterolateral ligament: anatomy, length changes and association with the Segond fracture. Bone Joint J 96-B(3):325–331
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105(2):136
Gupte CM, Bull AM, Thomas RD, Amis AA (2003) The meniscofemoral ligaments: secondary restraints to the posterior drawer. Analysis of anteroposterior and rotary laxity in the intact and posterior-cruciate-deficient knee. J Bone Joint Surg Br 85(5):765–773
Hallen L, Lindahl O (1966) The “screw-home” movement in the knee-joint. Acta Orthop 37(1):97–106
Hamner DL, Brown C, Steiner ME, Hecker AT, Hayes WC (1999) Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am 81(4):549–557
Hoshino Y, Araujo P, Ahldén M, Samuelsson K, Muller B, Hofbauer M, Wolf MR, Irrgang JJ, Fu FH, Musahl V (2013) Quantitative evaluation of the pivot shift by image analysis using the iPad. Knee Surg Sports Traumatol Arthrosc 21(4):975–980
Hughston JC, Eilers AF (1973) The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am 55(5):923–940
Irvine JN, Thorhauer E, Abebe ES, Tashman S, Harner CD (2014) ACL reconstruction: Is there a difference in graft motion for bone-patellar tendon-bone vs hamstring autograft at 6 weeks post-operatively? Orthop J Sports Med 2(2 suppl):2325967114S2325900044
Kawaguchi Y, Kondo E, Takeda R, Akita K, Yasuda K, Amis AA (2015) The role of fibers in the femoral attachment of the anterior cruciate ligament in resisting tibial displacement. Arthroscopy 31(3):435–444
Kennedy NI, LaPrade RF, Goldsmith MT, Faucett SC, Rasmussen MT, Coatney GA, Engebretsen L, Wijdicks CA (2014) Posterior cruciate ligament graft fixation angles, part 1: biomechanical evaluation for anatomic single-bundle reconstruction. Am J Sports Med 42(10):2338–2345
Kondo E, Merican AM, Yasuda K, Amis AA (2011) Biomechanical comparison of anatomic double-bundle, anatomic single-bundle, and nonanatomic single-bundle anterior cruciate ligament reconstructions. Am J Sports Med 39(2):279–288
Kousa P, Järvinen TLN, Vihavainen M, Kannus P, Järvinen M (2003) The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction: part I: femoral site. Am J Sports Med 31(2):174–181
LaPrade RF, Griffith CJ, Coobs BR, Geeslin AG, Johansen S, Engebretsen L (2014) Improving outcomes for posterolateral knee injuries. J Orthop Res 32(4):485–491
LaPrade RF, Ly TV, Wentorf FA, Engebretsen L (2003) The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med 31(6):854–860
LaPrade RF, Morgan PM, Wentorf FA, Johansen S, Engebretsen L (2007) The anatomy of the posterior aspect of the knee. J Bone Joint Surg Am 89(4):758–764
LaPrade RF, Wozniczka JK, Stellmaker MP, Wijdicks CA (2010) Analysis of the static function of the popliteus tendon and evaluation of an anatomic reconstruction the “fifth ligament” of the knee. Am J Sports Med 38(3):543–549
Li Y-L, Ning G-Z, Wu Q, Wu Q-L, Li Y, Hao Y, Feng S-Q (2014) Single-bundle or double-bundle for anterior cruciate ligament reconstruction: a meta-analysis. Knee 21(1):28–37
Linko E, Harilainen A, Malmivaara A, Seitsalo S (2005) Surgical versus conservative interventions for anterior cruciate ligament ruptures in adults. Cochrane Database Syst Rev (2). doi:10.1002/14651858.CD001356.pub3
Lopomo N, Zaffagnini S, Amis AA (2013) Quantifying the pivot shift test: a systematic review. Knee Surg Sports Traumatol Arthrosc 21(4):767–783
MacIntosh D, Darby T (1976) Lateral substitution reconstruction. J Bone Joint Surg Am 58:142
Maletis G, Inacio M, Desmond J, Funahashi T (2013) Reconstruction of the anterior cruciate ligament Association of graft choice with increased risk of early revision. Bone Joint J 95(5):623–628
Matsumoto H (1990) Mechanism of the pivot shift. J Bone Joint Surg Br 72(5):816–821
Merican AM, Amis AA (2009) Iliotibial band tension affects patellofemoral and tibiofemoral kinematics. J Biomech 42(10):1539–1546
Merican AM, Iranpour F, Amis AA (2009) Iliotibial band tension reduces patellar lateral stability. J Orthop Res 27(3):335–339
Miyatake S, Kondo E, Tsai T-Y, Hirschmann M, Halewood C, Jakobsen BW, Yasuda K, Amis AA (2011) Biomechanical comparisons between 4-strand and modified larson 2-strand procedures for reconstruction of the posterolateral corner of the knee. Am J Sports Med 39(7):1462–1469
Mohtadi NGH, Chan DS, Dainty KN, Whelan DB (2011) Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev (9):CD005960
Morgan PM, LaPrade RF, Wentorf FA, Cook JW, Bianco A (2010) The role of the oblique popliteal ligament and other structures in preventing knee hyperextension. Am J Sports Med 38(3):550–557
Mundasad S (2013) New ligament discovered in knee, Belgian surgeons say. http://www.bbc.co.uk/news/health-24826323
Musahl V, Seil R, Zaffagnini S, Tashman S, Karlsson J (2012) The role of static and dynamic rotatory laxity testing in evaluating ACL injury. Knee Surg Sports Traumatol Arthrosc 20(4):603–612
Musahl V, Voos J, O’Loughlin PF, Stueber V, Kendoff D, Pearle AD (2010) Mechanized pivot shift test achieves greater accuracy than manual pivot shift test. Knee Surg Sports Traumatol Arthrosc 18(9):1208–1213
Nesbitt RJ, Herfat ST, Boguszewski DV, Engel AJ, Galloway MT, Shearn JT (2014) Primary and secondary restraints of human and ovine knees for simulated in vivo gait kinematics. J Biomech 47(9):2022–2027
Peccin MS, Almeida GJM, Amaro JT, Cohen M, Soares BGO, Atallah ÁN (2012) Interventions for treating posterior cruciate ligament injuries of the knee in adults. Cochrane Database Syst Rev (2):CD002939
Petre BM, Smith SD, Jansson KS, de Meijer P-P, Hackett TR, LaPrade RF, Wijdicks CA (2013) Femoral cortical suspension devices for soft tissue anterior cruciate ligament reconstruction: a comparative biomechanical study. Am J Sports Med 41(2):416–422
Race A, Amis AA (1994) The mechanical properties of the two bundles of the human posterior cruciate ligament. J Biomech 27(1):13–24
Race A, Amis AA (1996) Loading of the two bundles of the posterior cruciate ligament: an analysis of bundle function in A–P drawer. J Biomech 29(7):873–879
Robinson JR, Bull AM, Amis AA (2005) Structural properties of the medial collateral ligament complex of the human knee. J Biomech 38(5):1067–1074
Salzler MJ, Harner CD (2014) Tunnel placement for the ACL during reconstructive surgery of the knee. J Bone Joint Surg Rev 2(4):e3
Sanchez AR, Sugalski MT, LaPrade RF (2006) Anatomy and biomechanics of the lateral side of the knee. Sports Med Arthroscopy Rev 14(1):2–11
Schulz M, Russe K, Weiler A, Eichhorn H, Strobel M (2003) Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg 123(4):186–191
Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R (2014) Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med 42:921–926
Sugita T, Amis AA (2001) Anatomic and biomechanical study of the lateral collateral and popliteofibular ligaments. Am J Sports Med 29(4):466–472
Tiamklang T, Sumanont S, Foocharoen T, Laopaiboon M (2012) Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev (11). doi:10.1002/14651858.CD008413.pub2
Vavken P, Murray MM (2013) ACL injury epidemiology. In: Murray MM, Vavken P, Fleming B (eds) The ACL handbook. Springer, New York, pp 3–17
Veltri DM, Deng X-H, Torzilli PA, Maynard MJ, Warren RF (1996) The role of the popliteofibular ligament in stability of the human knee: a biomechanical study. Am J Sports Med 24(1):19–27
Vincent J-P, Magnussen R, Gezmez F, Uguen A, Jacobi M, Weppe F, Ma Al-Saati, Lustig S, Demey G, Servien E, Neyret P (2012) The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc 20(1):147–152
Wijdicks CA, Kennedy NI, Goldsmith MT, Devitt BM, Michalski MP, Årøen A, Engebretsen L, LaPrade RF (2013) Kinematic analysis of the posterior cruciate ligament, part 2: a comparison of anatomic single- versus double-bundle reconstruction. Am J Sports Med 41(12):2839–2848
Woo SL-Y, Hollis JM, Adams DJ, Lyon RM, Takai S (1991) Tensile properties of the human femur-anterior cruciate ligament-tibia complex: the effects of specimen age and orientation. Am J Sports Med 19(3):217–225
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Halewood, C., Amis, A.A. Clinically relevant biomechanics of the knee capsule and ligaments. Knee Surg Sports Traumatol Arthrosc 23, 2789–2796 (2015). https://doi.org/10.1007/s00167-015-3594-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3594-8