Abstract
The complex biomechanics of the human knee joint are the result of an equilibrium of forces exerted by its surrounding soft tissue structures. When one of these forces is removed, as is the case when a ligament ruptures, a redistribution of forces occurs and the biomechanical properties of the knee are altered. One of the most frequently diagnosed knee ligament ruptures is that of the anterior cruciate ligament (ACL). Such a rupture causes increased laxity of the knee joint as well as a complex rotational and translational instability whereby many patients describe a feeling that their knee is slipping, or “giving way.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Biomechanical assessment of knee
- Knee ligament ruptures
- Three-dimentional assessment of knee ligament
- 3D knee ligament assessment
- Anterior cruciate ligament ruptures
The complex biomechanics of the human knee joint are the result of an equilibrium of forces exerted by its surrounding soft tissue structures. When one of these forces is removed, as is the case when a ligament ruptures, a redistribution of forces occurs and the biomechanical properties of the knee are altered. One of the most frequently diagnosed knee ligament ruptures is that of the anterior cruciate ligament (ACL). Such a rupture causes increased laxity of the knee joint as well as a complex rotational and translational instability whereby many patients describe a feeling that their knee is slipping, or “giving way” [1].
The ACL has been one of the most studied structures of the musculoskeletal system. Despite the abundance of literature, there is little consensus amongst orthopaedic surgeons as to the specific biomechanical effect of an ACL rupture on knee joint function [2]. However, in order to provide effective treatment, it is important that the mechanisms of an injury and the resulting pathomechanics be identified [3]. As such, biomechanical studies of the impact of ACL injuries remain a hot topic and are the subject of much debate. They provide important information that cannot be obtained through current clinical evaluations.
In 2008, Chan et al. [4] proposed a new paradigm, « Orthopaedic sport biomechanics », where the role of biomechanics in orthopaedics is threefold: (1) it helps in the prevention of musculoskeletal sport-related injury and trauma, (2) it provides an objective quantitative assessment to evaluate the immediate outcome of treatment, either operative or conservative, (3) it acts as an objective tool to monitor the long-term rehabilitation progress, and to indicate if an athlete is adequately recovered to a satisfactory level for returning to sports.
Given the ACL’s important role in the 3D stability of the knee joint [5], particularly in internal tibial rotation [6, 7], identifying the pathomechanics of an ACL rupture requires the ability to record knee bone movements in 3D [8, 9]. To do so, one must be able to follow the bones with sufficient precision despite skin movement artifacts, and to represent this movement in an anatomical coordinate system that is highly reproducible.
For the past 20 years, our research group has been working on the precise recording and in vivo analysis of 3D kinematics of the knee, with an emphasis on the effect of an ACL rupture. This chapter presents the non-invasive methodology used to obtain precise and reliable recordings of knee bone movements as well as its use in establishing the biomechanical impact of an ACL rupture on regular paced gait. This is followed by an analysis of the kinematics of the pivot shift test, a clinical test that reproduces the functional instability of the knee. Finally, the implications of 3D biomechanical analyses of the knee are discussed.
Recording 3D Knee Kinematics
Marker Attachment
The recording of human movement is generally achieved by fixing motion capture devices or markers (active or passive) to different body segments. There are a number of technologies available that allow for high spatial and temporal precision when recording movement. As such, it is theoretically possible to quantify very subtle changes in knee joint kinematics. However, in practice, the skin displacement relative to the underlying bones introduces significant measurement errors. Many authors have raised this issue and quantified the effect of skin displacement artifacts [10–16]. For movements of smaller amplitude, e.g. axial rotation of the tibia, the error due to such artifacts has been shown to surpass the actual motion of the bones [12].
In order to limit these errors, different strategies have been proposed for the fixation of motion-capture devices or markers to the lower limb. These solutions can be separated into three categories: optimization of skin mounted markers, percutaneous fixations and external attachment systems. This section provides a brief summary of each of these categories and presents the solution used by our research group.
Skin Mounted Marker Optimization
The first category involves an optimization of the simplest method for attaching motion capture devices: fixing them directly to the skin. This is usually done using a double-sided tape and obviously does nothing to reduce skin displacement artifacts. The optimization consists in fixing a large number of markers over the thigh and shank. Algorithms are then used to approximate the true bone movements based on the fact that in the absence of skin displacement, there should be no relative movement between the different markers.
Many different methodologies and algorithms have been proposed. Some studies have shown significant reductions in skin displacement artifacts [11, 17, 18], while others found these artifacts to remain substantial after application of the algorithm [19–21]. Overall, this method has shown promise, but results vary widely from one study to the next. The main challenge for these algorithms stems from the fact that the source of movement of the skin is the same as that of the bones; frequencies are thus similar [14]. Furthermore, it is possible for all the skin-mounted markers to move without actual bone movement. Strategies relying on algorithms to reduce artifacts from skin-mounted markers are also ill suited for clinical evaluation because of the time and energy necessary to fix a large number of markers.
Percutaneous Fixation
Percutaneous pins, or intra-cortical pins, are generally stainless steel cylinders with diameters that vary from 2.5 to 3.6 mm [22]. They are screwed into the cortical bone at depths up to 20 mm. Electromagnetic sensors or reflective markers are mounted on the pins using a fixation device. The use of such pins is obviously the method that allows for the most precise measurement of bone movements. No study of their accuracy has been published, as this is the method that is considered to be the gold standard in evaluating knee joint kinematics. As such, many authors have conducted studies where knee joint kinematics were simultaneously recorded by percutaneous pins and by another attachment system to evaluate to precision of the latter [12, 16].
Despite being considered the gold standard, the use of percutaneous pins does not guarantee 100 % accuracy. In addition to the error of the motion capture technology, the tendons and the skin surrounding the pins may, in some cases, cause the pins to bend or become dislodged. Some studies have reported the exclusion of up to 54 % of their subjects because of such dislodgement [12, 16, 22]. In the absence of such complications, percutaneous pins remain the most accurate method for measuring bone movements. However, their use brings obvious drawbacks related to their invasive nature. Local or general anesthesia must be administered to the subjects and the fixation of the pins can be time consuming. As such, their use is restricted to research or peri-operative evaluation.
External Attachment Systems
The final category for reduction of skin displacement artifacts is composed of several different non-invasive systems that attach to the lower limb and onto which reflective markers or electromagnetic sensors are mounted. They are said to be non-invasive because they contact the skin without penetrating it.
The most widespread amongst such systems consists of rigid plastic plates that are fixed to the shank and thigh, usually at mid-segment. This method is commonly referred to as the Cleveland Clinic method (Fig. 39.1). When one of the markers is fixed to a pin that is perpendicular to the rigid plate, it is called the Helen Hayes method [15].
Different variations of the Cleveland Clinic and Helen Hayes methods (From Manal et al. [15], with permission)
Manal et al. [15] evaluated the accuracy of 6 variations of such attachments for measuring axial tibial rotations during gait. They found it to be about ±4° using the most accurate variation (Fig. 39.1b). Given that the range of axial tibial rotation averages approximately 9°, this is a significant error. Ferber et al. [23] later used this variation of the attachment system to evaluate the test-retest reliability of this attachment system to record knee joint kinematics during running. For many kinematic parameters, intra-class correlation coefficients (ICCs) were found to be below 0.75, which is considered to be the limit of acceptability [24].
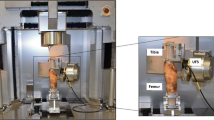
Other research groups have developed their own, more elaborate attachment systems and used them in recording lower limb gait kinematics [25–27]. The system developed and used by our research group is now called the KneeKGTM (Emovi inc., Montreal, Canada). First described by Sati et al. [28] under the name of exoskeleton, this system includes a femoral and a tibial component (Fig. 39.2). The design of the femoral component was inspired by a fluoroscopic study that showed that the amplitude of skin displacement about the knee varies greatly depending on the exact location [10]. The study identified two locations where the displacement is minimal. The femoral component attaches to these anatomical locations. It is composed of a rigid arch with spring-loaded forms at each extremity, effectively forming a clamp. The medial extremity of this clamp inserts between the vast medialis and the sartorius muscle tendon; the lateral extremity inserts between the femoral biceps and the ilio-tibial band (ITB). Both extremities rest atop the femoral condyles. A medial condyle support pad and a stabilizing plaque that is attached to a Velcro strap, placed around the proximal thigh, prevent rotation of the system about the clamp’s contact points.
The accuracy of the KneeKGTM was evaluated by a fluoroscopic study. Radio-opaque beads were fixed to the femoral component, which was installed on three different subjects who performed active flexion/extension under fluoroscopy. Average errors were found to be −0.4° in abduction/adduction and −2.3° in tibial rotation [28]. A subsequent study of five subjects, with a similar methodology, found that the quadratic error is diminished by a factor of 4.3 for abduction/adduction and by a factor of 6.2 for axial tibial rotation when compared with skin mounted markers [29]. Both these studies evaluated the accuracy of the KneeKGTM using non weight-bearing knee flexions.
The intra- and inter-observer reliability of the KneeKGTM were evaluated to insure that when the system was removed and reinstalled, similar results were obtained regardless of the examiner who installed it [30]. In the intra-observer setting, a single observer installed the system and recorded the gait kinematics three times each for 12 different subjects. Reliability was found to be high, with intra-class correlation coefficients (ICC) between 0.88 and 0.94 for knee rotations. The average standard measurement error (SEM) was below 1° for rotations about all three axes. In the inter-observer setting, three observers each installed the system twice on all 12 subjects. Similar to the intra-observer data, the ICCs from the inter-observer measurements were between 0.89 and 0.94, with all SEMs below 1°.
Movement Representation
Euler Angles Versus Helical Axis Definition
After knee movement has been measured precisely and reliably, it is necessary to represent it in a meaningful way. It has been suggested that the unambiguous description of spatial motion is more difficult than its measurement [31]. Because the knee is not a hinge and movement about that joint does not occur in a 2D plane, it is difficult to represent knee kinematics. Typically, 2 methods are used to study 3D kinematics of the knee: Euler angles [32] and helical axes [33].
Even though the knee is not gyroscopic, the Euler angle method is the most widely employed. With this method, it is possible to describe a 3D movement as 3 successive rotations about three different axes defined in space: flexion/extension, abduction/adduction and internal/external tibial rotation. These axes can be fixed or floating, and represented locally or globally. The major advantage of this method is that it is easier to interpret the results clinically with anatomical descriptions of movements. With this method, it is also possible to compute anteroposterior (AP), proximodistal (PD), and mediolateral (ML) translations.
However, the main disadvantage of the Euler angle method is that it is very sensitive to anatomical reference axes definition. Small errors (1–2 mm in the definition of points used to build the coordinate system) cause errors in orientation as well as in kinematic amplitude on the order of 2°. When coordinate systems are built on subjects, errors in landmark definition can be on the order of 30 mm. These large errors make it difficult, even impossible, to compare results [19]. Also, it is not clear if differences in bone geometry affect the kinematic patterns that are generated. For this reason, we do not know the 3D kinematics of the normal knee. Each knee has a kinematic representation associated with a given local coordinate system.
The helical axes method [33] uses the 3D position of each bone to describe the movement of the knee between 2 moments in time as a unique rotation and a unique translation about a finite rotation axis. Therefore, when employing this method to describe knee kinematics, we need to define the time period during which we want to express the rotation and translation of one bone with respect to the other. The main advantage of this method is that it is independent of an anatomical coordinate system definition. However, the use of helical axes to describe joint movements is not well understood by the clinical community [32]. Also, the method is sensitive to noise in the measurement and to the time period used for computation of the finite rotation axis.
We chose to follow the recommendation of the International Society of Biomechanics (ISB) by representing knee movements using Euler angles, which allow for better clinical interpretation. We therefore needed to define anatomical coordinate systems associated with the femur and tibia.
Anatomical Coordinate Systems
Anatomical landmarks need to be identified in order to establish the bone-embedded coordinate systems. These landmarks can be defined by a pointer or by fixing markers directly over them. This technique generates errors of many mm or even a few cm. To diminish imprecision when building coordinate systems, we have developed a method that uses fewer anatomical landmarks to define the reference coordinate system than other methods in the literature [34].
This coordinate system is called the Functional Postural (FP) method and was first described by Hagemeister et al. [35] The joint centers are defined as follows.
- Ankle joint center (AJC)::
-
The midpoint between the medial and lateral malleoli.
- Hip joint center (HJC)::
-
The center of the femoral head. It is identified from a recording of hip circumduction using a pivot algorithm, as proposed by Siston and Delph [36].
- Knee joint center (KJC)::
-
The midpoint between the medial and lateral epicondyles, projected onto the mean axis of knee flexion/extension
The PD axes of the tibia and femur are respectively defined by the vectors joining the KJC to the AJC and the KJC to the HJC. The subject is then placed in a reference guide with his frontal plane aligned with that of the guide. The sagittal plane is then defined during a movement of slight flexion/extension, alternating between approximately 10° of flexion and maximum extension. It is defined as the plane whose normal vector is the cross product of the normal vector of the frontal plane with the vector joining the HJC and the AJC. The neutral position of the knee joint is defined at the moment when the PD axes of the tibia and femur are aligned in the sagittal plane. In this position, the AP axes of the tibia and femur are defined as perpendicular to the normal vector of the sagittal plane and their PD axes. Finally, the ML axes of each of the bones are the axes that complete the orthonormal sets (Fig. 39.3).
Inter- and Intra-tester Variability
To test inter- and intra-tester variability for the calibration procedure, the following protocol was performed. The attachment system was first installed on each subject, and three testers performed the above-described calibration procedure on four subjects. Each tester repeated the procedure 5 times. Then, the subjects walked on a treadmill at a comfortable speed for 3 min, and finally, 30 gait cycles were recorded. The mean of these 30 cycles was used to compute the kinematic parameters (flexion/extension, abduction/adduction and internal/external rotation of the tibia as well as A-P translation as a function of percentage of the gait cycle) in association with the 15 calibration procedures. The resulting 15 curves were compared for each subject using an adjusted coefficient of multiple determinations. Figure 39.4 presents an example of the kinematic parameters calculated with 5 calibration procedures performed by 1 tester on 1 subject.
The results show that the calibration method allows the measurement of 3D knee kinematics with good reproducibility. Mean errors generated by the calibration procedure are 1.1° in flexion/extension, 1.1° in abduction/adduction, 0.8° in internal/external tibial rotation, and 2.6 mm in A-P translation.
Gait Analysis
Following an ACL injury, gait analysis has been shown to provide beneficial information for assessing knee stability [37] and functional impairments [38] under dynamic conditions. Numerous studies have already reported that patients with an ACL deficiency present altered 3D knee kinematics [9, 38–43] and 3D knee joint moments [38, 44–46]during gait. In these studies, 3D biomechanical patterns of the knee are presented over a full gait cycle, which is divided into a stance phase and in a swing phase. These phases represent 60 % and 40 % of the total gait cycle (GC), respectively. During the stance phase, sub-phases occur as follow: the initial contact (1–2 % of the GC), the loading phase (1–10 % of the GC), the mid stance phase (10–30 % of the GC), the terminal stance phase (30–50 % of the GC) and the pre-swing phase (50–60 % of the GC) [47].
Gait Biomechanics
Kinematics
To identify knee biomechanical deficiencies following an injury, a good understanding of “normal” patterns is required, since they serve as a reference to compare the pathological patterns [48]. Numerous studies have published “normal” knee biomechanical patterns during gait. Typically, the knee arcs of motion during walking in the sagittal, frontal and transverse planes are approximately 70°, 5° and 9°, respectively [47]. However, a qualitative review of these studies unveils a lack of correspondence in normal 3D knee kinematic patterns. These discrepancies are generally found in the frontal and transverse plane. The variation in methodologies used to record 3D joint kinematics between studies is potentially responsible for these differences [49].
Kinetics
During gait, the knee joint is continuously submitted to important moments and forces that influence the joint kinematics in all three planes of movement. Since joint kinetics cannot be measured in vivo, we must first record the joint kinematics and the ground reaction forces to compute these forces and moments [50] using calculations of inverse dynamics. The internal joint forces and moments applied by the joint’s soft tissue structures (muscles and ligaments) must constantly counteract the external forces and moments acting upon the knee. For example, during gait, the limb must alternately counterbalance moments that tend to extend and flex the knee joint. Quantifying knee joint kinetics allows a better understanding of functional adaptations following an injury such as an ACL tear [51].
ACL-Deficient Gait
The scientific literature relating to gait adaptations in ACL-deficient patients is abundant. However, a consensus on which gait compensatory mechanism is adopted by these patients remains to be established [52]. In fact, it was suggested that different biomechanical adaptations could be adopted within an ACLD population [43] and that gait adaptation changes over time [38]. To date, two main gait compensatory mechanisms have been proposed: (1) the quadriceps avoidance gait and (2) the hamstring facilitation strategy. Furthermore, only a restricted number of studies have looked at knee biomechanical patterns associated with the role of the ACL (i.e. anteroposterior translation and internal/external axial rotation). The following section will present a brief review of theses adaptations and biomechanical deficiencies and relate them to the results of our studies.
We conducted a 3D knee biomechanical assessment of 29 chronic ACLD patients and 15 healthy participants during treadmill walking. The 3D knee biomechanics were recorded using the KneeKGTM and a VICON optoelectronic system (Oxford Metrics, Oxford, UK). Joint centers and coordinate systems were defined using the FP method and the biomechanical patterns were computed using the ISB convention [32].
Quadriceps Avoidance Gait
Quadriceps avoidance gait is defined by the absence of the external knee flexor moment during the mid stance phase of the gait cycle [45]. Since this external joint moment tends to flex the knee while the body is progressing forward, an eccentric contraction of the quadriceps is typically required to counterbalance this moment. Berchuck et coll. 1990 [45] suggested that ACLD patients adopt this compensatory mechanism by reducing the quadriceps contraction. The rationale behind this hypothesis is that ACLD patients tend to avoid the anterior traction of the proximal tibia provoked by the quadriceps contraction, which could lead to AP instability. One study did show a decrease in quadriceps muscle activity during stance phase [53] and several other studies [38, 51, 54, 55] identified a decrease in the external knee flexor moment in ACLD patient.
However, not all of the scientific community endorses this compensatory mechanism theory. In fact, recently published studies refute the very presence of these changes [42, 52, 56]. In our study, ACLD patients did not exhibit a quadriceps avoidance gait pattern (Fig. 39.5). This is supported by several studies demonstrating no EMG changes in the quadriceps muscle activity [52, 57–59]. In contrast with the quadriceps avoidance gait theory, some authors suggest that a reduction of the external knee flexor moment could be related to other biomechanical adaptations. Indeed, some believe that this gait adaptation could be associated with higher knee flexion angles [38, 45, 55]. Others suggest it could be linked to an increased external hip flexor moment [43, 55, 60], which would decrease the tension in the quadriceps. These controversial results underline the lack of consensus concerning this knee biomechanical adaptation [61].
Roberts et al. [52] suggested that the presence of the quadriceps avoidance gait pattern could be linked to methodological considerations since most of the studies reporting this strategy used a simpler linked segment model to compute knee joint moments. In our study, joint moments were computed using inverse dynamics with the wrench notation and quaternion algebra [62].
Hamstring Facilitation Strategy
In the past few years, several biomechanical studies have found that ACLD patients adopt a hamstring facilitation strategy. The rationale behind this compensatory mechanism theory is that higher hamstring muscle activity will act as an agonist to the injured ACL by generating a posterior traction of the proximal tibia. Numerous studies have shown a significant increase hamstring muscles activity [52, 53, 57, 59]. Furthermore, many studies have identified biomechanical changes that could be linked to this adaptation strategy. First, ACLD patients have been shown to walk with a higher knee flexion angle during the terminal stance phase [53, 58, 63–65]. Interestingly, the knee flexion angle during the stance phase was positively correlated with the duration of hamstring activity [57]. Additionally, ACLD patients have been found to display higher hamstring activity in the swing to stance transition [66]. The findings of our study are in agreement with these kinematic compensations. Indeed, Fig. 39.6 shows the knee flexion/extension pattern over a full gait cycle for the ACLD group and the control group. The ACLD group walked with significantly higher knee flexion angles at initial ground contact, during the terminal stance phase and at the end of the swing phase. The asterisks (*) show where statistical differences (P < 0.05) were identified.
Biomechanical Deficiencies Associated with the Role of the ACL
Studies quantifying the AP translation and internal-external axial rotation of the knee are scarce. This is mainly due to the high level of error associated with the measurement of these small amplitude translations and rotations. Nevertheless, an increased anterior translation of the tibia in the transition between a non-weightbearing and weightbearing condition was reported in ACLD patients [67]. Furthermore, two studies using an electrogoniometer to quantify the kinematics of ACLD knees during gait showed an increase in anterior tibial translation [9, 68]. However, given the error associated with the measurement of proximal AP translation of the tibia [14], these results should be considered with caution.
Although only a few papers were published on the impact of an ACL tear on the knee axial rotation, contradictions emerge between studies. Some authors identified an increase in external tibial rotation with regards to the femur during gait [9, 52]. Others found a shift towards internal tibial rotation [40, 41]. Our study is in agreement with the latter. Whereas previous papers showed that this shift occurs throughout the gait cycle, our results only identified statistical differences in the swing to stance transition and during the beginning of the loading phase (Fig. 39.7).
The identified decrease in external tibial rotation in ACLD patients at the end of the swing phase, where the knee reaches near full extension, was also reported in previous studies [40, 68]. These results support previous findings that the screw home mechanism is altered after an ACL injury [69]. This altered axial tibial rotation could also be explained by the lack of knee extension at the end of the swing phase.
Three-dimensional biomechanical evaluations have allowed a better understanding of the impact of an ACL injury on the function of the knee joint. The large number of studies on this subject underlines the importance of such evaluations as complements to orthopaedic physical assessments in helping to improve current treatments for ACL injuries.
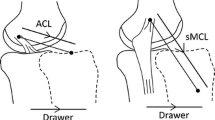
Analysis of the Pivot Shift Phenomenon
During a clinical evaluation, an ACL-deficient knee will generally present an increase in joint laxity, especially in the AP axis. This uniaxial laxity is relatively easy to evaluate using clinical examinations. The most sensitive of these examinations is the Lachman test, whereby the clinician applies an anterior force to the tibia while holding the femur in place. The amount of anterior displacement is very useful in diagnosing an ACL rupture [70–73] but it shows no correlation to subjective criteria of knee joint function [74–78]. The pivot shift test is a dynamic clinical test that reproduces the 3D rotational instability felt by patients who describe feeling that their knee is giving way. The pivot shift grade correlates with reduced patient satisfaction, partial giving way, full giving way, difficulty cutting, difficulty twisting, activity limitation, reduced overall knee function, reduced sports participation, and Lysholm score [74]. Subjects with higher-grade pivot shift tests had less satisfaction, more limitations and lower knee function.
A meta-analysis found that the Lachman test is more sensitive but less specific than the pivot shift test [70]. In other words, a positive pivot shift test indicates an ACL rupture and a negative Lachman test rules it out.
Although it is obviously important to diagnose an ACL rupture, it is often the level of knee joint function that is of most interest and that clinicians aim to restore. Both tests are important parts of a clinical evaluation but serve different purposes. The pivot shift test’s specificity makes it a valuable complement to the Lachman test in establishing a diagnosis, but more importantly, the pivot shift test is the only test which can be used to assess the level of knee joint function and predict long term outcome. As such, many studies conclude that the objective of reconstructive surgery should be to eliminate the presence of a pivot shift and not only to diminish AP laxity [39, 79–81].
Clinical Examination
The pivot shift test is performed with the patient supine and the examined leg lifted off the examining table by a clinician. A gentle valgus force is applied to the knee and the knee is flexed in a controlled manner with slight internal rotation of the tibia. In the ACL-deficient knee, as flexion occurs, the tibia translates anteriorly and rotates internally. The joint is subluxed at this point. As the knee is flexed past 30°, soft tissues and joint geometry cause the joint to reduce [82]. This is the pivot shift.
The clinician attributes the grade of the pivot shift relying on his interpretation and experience as being 0 (absent), 1 (glide), 2 (clunk) or 3 (gross) [83]. The nature of this grading scale renders it poorly repeatable [84]. Indeed, it has been shown that different clinicians frequently attribute different grades to a same patient [85]. No objective method for evaluating the pivot shift test currently exists, despite several attempts in the literature [86–91]. In the absence of an objective pivot shift measurement tool, it is difficult for less experienced clinicians to attribute a grade with a sufficiently high level of confidence for it to be used in determining the course of treatment.
Recording the Pivot Shift
The KneeKGTM attachment system, presented in Sect. 2.1.3, was designed for use on a standing subject. Its femoral component, which rests atop the femoral condyles, falls out of place when a subject is placed in a supine position. For this reason, an adapted version of this system was developed to record the kinematics of the pivot shift. The rigid arc of the femoral component is replaced by an elastic Velcro strap (Fig. 39.8a). This strap allows for inward pressure to be applied and it prevents the attachment from falling out of place when the subject is supine. The purpose of the rigid plates is to improve the attachment’s stability and to allow for fixation of the motion capture sensors.
The tibial component is composed of a rigid plate that is held over the tibia with an elastic Velcro strap, immediately distal to the tibial tuberosity (Fig. 39.8b). It is short in length to allow a clinician to manipulate the lower limb without displacing it. A preliminary study conducted with three subjects wearing this attachment system showed it to be as reliable as the KneeKGTM for gait analysis.
The FP method, which is used to establish the anatomical axes, was also adapted to for the pivot shift test. The joint rotations were passively applied on the supine subject by the examiner.
Kinematics of the Pivot Shift
The reduction phase of the pivot shift occurs when the subluxed tibia returns to its normal position. This reduction has been described as a combination of posterior translation and external tibial rotation. With the development of methodologies to record the 3D kinematics of the pivot shift, many studies have investigated these features and how they relate to the grade of the pivot shift established by a clinician. One of the objectives of such studies is to develop an objective grading scale where, for example, some combination of both axial tibial rotation and posterior translation would be taken as a pivot shift score and the grade would be established from these scores.
Recent studies have found that the 3D kinematics of the pivot shift vary too much between subjects for such a simple score to be used. Although the amplitude of posterior translation correlates to the clinical grade, values are very different for two subjects of a same grade. The axial tibial rotation is even more variable: some subjects present significant external rotations during the reduction phase while others show none at all [88], leading authors to question its relevance in measuring the pivot shift.
In a recent study, we recorded the knee joint kinematics of 127 pivot shift tests and investigated the correlation with the clinical grade established by the clinician who performed the test [30, 92, 93]. Figure 39.9 presents a typical recording of a grade 3 pivot shift. A spike in linear velocity and acceleration is clearly visible during the reduction phase.
Kinematics of a typical grade 3 pivot shift (Adapted from Labbe et al. [30], with permission.)
To further investigate the kinematic features of the pivot shift that are related to its clinical grade, we conducted a principal component analysis (PCA). The objective of PCA is to reduce the number of features while retaining as much of the variation present in the original dataset as possible. To do so, it transforms a large number of features into a smaller number of uncorrelated features, called principal components (PCs). The first PC accounts for the largest amount of variability in the data and each of the subsequent PC accounts for the largest amount of the remaining variability.
We applied PCA on our full set of features, which was composed of the amplitude, velocity and acceleration of AP, ML and total translations, abduction/adduction and axial tibial rotation. The first PC accounted for 38 % of the overall variability between the pivot shift recordings and the first four PCs accounted for a total of 69 %. To verify which PCs contained variability that is useful in grading the pivot shift, we calculated their correlation to the clinical grades. The first PC had a Spearman’s rank correlation coefficient of 0.55 while the next three had coefficients of −0.09, 0.04 and 0.01, respectively [92]. These values show that only the first PC is related to the pivot shift grade.
Next, we calculated the factor loadings of the original features on the first PC. Loading factors are correlations between the features and the PCs. Features with a high loading factor are representative of the component [94]. Table 39.1 shows the features with factor loadings that are superior to 0.5 on the first PC.
These results show that the translational component of the pivot shift is indeed more closely related to the grade than its rotational component. Moreover, the acceleration and velocity of the translations have a higher correlation to the grade than the actual amplitude of those translations. Other authors have also found the acceleration to be an important feature of the pivot shift [87, 89]. This makes sense since the existing subjective scale describes the pivot shift grades using terms such as “clunk” and “gross clunk”, which infer a notion of suddenness rather than amplitude of displacement.
Recent studies in biomechanics have successfully classified kinematic data using machine learning methods [95–98]. We chose to use a support vector machine (SVM) approach using the grade established by the clinician as a gold standard. An SVM is a supervised learning method used for binary classification. To distinguish multiple classes, the method must be applied iteratively. This lends itself well to the grading of the pivot shift. In fact, the recordings can be first separated into that present a clunk (grade 2 and 3) and those that don’t (grades 0 and 1). As a second step, the recordings with a glide (grade 1) can be distinguished from those with no glide (grade 0). Finally, those presenting a clunk (grade 2) can be distinguished from those presenting a more obvious, gross clunk (grade 3).
The features that load on the first principal component were added to the SVM classifier in descending order of their factor loadings (Table 39.1). All of these features were used to separate grades 0 and 1 from 2 and 3, and to separate grade 2 from grade 3 recordings with maximum sensitivity. For separating grades 0 and 1, maximum sensitivity was attained using only the amplitude of tibial translation and the velocity of axial tibial rotation. It makes sense that the acceleration and velocity of the translation are not useful for this step as we are distinguishing between the absence and presence of a glide. There is no notion of clunk in these grades [93].
The SVM classifier established the same grade as the evaluating clinician 66 % of the time and was within one grade for 95 % of recordings (Table 39.2). Agreement between the clinicians and the classifier, as defined by a Cohen’s weighted Kappa, was κ = 0.68, which is considered to be substantial agreement [99]. Because of the subjective nature of the existing scale, which relies heavily on a clinician’s interpretation, is it to be expected that there be some disagreement with classification method. Nonetheless, such a method offers an objective alternative to grading the pivot shift and sheds new light on the features that are felt and subjectively evaluated when a clinician grades a pivot shift. These features could be used to develop a quantitative measure of the pivot shift on a continuous scale.
The assessment of the 3D kinematics of the knee during the pivot shift test helps to further understand the effect of an ACL rupture on knee joint function. More importantly, such instrumented evaluations could eventually be used to help the clinician diagnose the severity of an injury, evaluate its impact on a specific patient and choose the appropriate treatment.
General Discussion
In vivo measurement of small translations and rotations of the knee is a difficult task, especially in the frontal and transverse planes (abduction/adduction and internal/external tibial rotation). Precision is an important concern due to the fact that soft tissue movements introduce noise into the recordings of the underlying bone movements. Reinschmidt et al. [16] compared knee rotations in subjects whose kinematics were recorded via skin markers and bone pins inserted into the femur and tibia. They showed that average errors during running due to skin movements were about 21 % for flexion/extension, 63 % for internal/external tibial rotation, and 70 % for abduction/adduction. Since bone-embedded pins are not a solution that can be used in clinics on a routine basis, it is important to use a marker fixation method that limits skin displacement artifacts.
The method used to represent the movement in the anatomical axes of the knee is also of critical importance. In fact, small errors in the positioning of these axes generate large errors in rotation calculations [19]. One solution to improve reliability without the use of x-rays is to use a method that requires as few anatomical landmarks as possible to define the coordinate system. The method we used, the FP method, has been shown to yield reproducible data when repeated measures where performed by the same observer or by different observers. By using such a method, combined with a validated attachment system, we can record in-vivo knee biomechanics with maximum precision and reliability.
The resulting biomechanical assessments provide information on knee joint function that is not available through current clinical evaluations. This includes the normal joint kinematics, the kinematic impact of an injury and the extent to which different treatments restore normal joint kinematics. Such information allows healthcare professionals to evaluate the immediate and long-term outcome of treatment, establish the right time to return to sports participation and suggest injury prevention exercises. These are the three roles of biomechanics Chan’s Orthopaedic Sport biomechanics paradigm [4].
The results presented in this chapter suggest that two other roles should be added to this paradigm. Gait analysis has shown its potential in evaluating the impact of an injury on knee joint function. As such, biomechanics has the potential to allow health professionals to better understand the functional impact that an injury has on a specific patient and to tailor his treatment plan accordingly. The relation between altered knee joint kinematics and degenerative changes in the knee has been shown [100, 101]. Personalized biomechanical evaluations can have a significant impact on the development of rehabilitation programs and surgical treatments aimed at restoring the dynamic stability of a knee and preventing secondary injuries.
The assessment of the kinematics of the pivot shift shows that biomechanics can also be an important tool as a diagnostic aid. Indeed, a recent study by Peeler et al. [102] showed the level of precision and validity of clinical exams for ACL ruptures performed by front line healthcare professionals (physiotherapists, sport therapists, general practitioners) to be much lower than had been previously reported. The authors speculate that this could be due to the difficulty in performing the manual clinical tests and the subjective bias related to grading such tests. This underlines the need for objective analytical methods that can aid in establishing a correct diagnosis.
Biomechanics already has the potential to be a useful tool in orthopaedics, as demonstrated by the examples in this chapter. With availability of improved methods for recording and analyzing bone movements, more and more studies are finding potential applications for prevention, diagnosis, impact assessment and evaluation of outcome of different joint injuries and ailments. The key to benefiting from the full potential of integrating 3D biomechanical assessments into orthopaedic practice is to have a multidisciplinary approach of dynamic interactivity and communication between specialists from different fields.
References
Bull AMJ, Amis AA. The pivot-shift phenomenon: a clinical and biomechanical perspective. Knee. 1998;5:141–58.
Bicer EK, Lustig S, Servien E, Selmi TA, Neyret P. Current knowledge in the anatomy of the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18(8):1075–84.
Bahr R, Krosshaug T. Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med. 2005;39:324–9.
Chan KM, Fong DT, Hong Y, Yung PS, Lui PP. Orthopaedic sport biomechanics - a new paradigm. Clin Biomech (Bristol, Avon). 2008;23 Suppl 1:S21–30.
Woo SL-Y, Adams D, Takai S. The human anteriorcruciate ligamentand its replacement: biomechanical considerations. In: Niwa S, Perren S, Hattori T, editors. Biomechanics in orthopedics. Tokyo: Springer; 1993. p. 13–30.
Girgis FG, Marshall JL, Monajem A. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop. 1975:216–31.
Furman W, Marshall JL, Girgis FG. The anterior cruciate ligament. A functional analysis based on postmortem studies. J Bone Joint Surg Am. 1976;58:179–85.
Favre J, Luthi F, Jolles BM, Siegrist O, Najafi B, Aminian K. A new ambulatory system for comparative evaluation of thee-dimansional knee kinematics, applied to anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2006;14:592–604.
Zhang LQ, Shiavi RG, Limbird TJ, Minorik JM. Six degrees-of-freedom kinematics of ACL deficient knees during locomotion-compensatory mechanism. Gait Posture. 2003;17:34–42.
Sati M, de Guise JA, Larouche S, Drouin G. Quantitative assessment of skin-bone movement at the knee. Knee. 1996;3:121–38.
Alexander EJ, Andriacchi TP. Correcting for deformation in skin-based marker systems. J Biomech. 2001;34:355–61.
Benoit DL, Ramsey DK, Lamontagne M, Xu L, Wretenberg P, Renstrom P. Effect of skin movement artifact on knee kinematics during gait and cutting motions measured in vivo. Gait Posture. 2006;24(2):152–64.
Holden J, Orsini J, Siegel K, Kepple T, Gerber L, Stanhope S. Surface movement errors in shank kinematics and knee kinetics during gait. Gait Posture. 1997;5:217–27.
Manal K, McClay Davis I, Galinat B, Stanhope S. The accuracy of estimating proximal tibial translation during natural cadence walking: bone vs. skin mounted targets. Clin Biomech (Bristol, Avon). 2003;18:126–31.
Manal K, McClay I, Stanhope S, Richards J, Galinat B. Comparison of surface mounted markers and attachment methods in estimating tibial rotations during walking: an in vivo study. Gait Posture. 2000;11:38–45.
Reinschmidt C, van den Bogert AJ, Nigg BM, Lundberg A, Murphy N. Effect of skin movement on the analysis of skeletal knee joint motion during running. J Biomech. 1997;30:729–32.
Andriacchi TP, Alexander EJ, Toney MK, Dyrby C, Sum J. A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. J Biomech Eng. 1998;120:743–9.
Waite JC, Beard DJ, Dodd CA, Murray DW, Gill HS. In vivo kinematics of the ACL-deficient limb during running and cutting. Knee Surg Sports Traumatol Arthrosc. 2005;13:377–84.
Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–92.
Cappozzo A, Catani F, Leardini A, Benedetti MG, Croce UD. Position and orientation in space of bones during movement: experimental artefacts. Clin Biomech (Bristol, Avon). 1996;11:90–100.
Cheze L, Fregly BJ, Dimnet J. A solidification procedure to facilitate kinematic analyses based on video system data. J Biomech. 1995;28:879–84.
Levens A, Inman V, Blosser J. Transverse rotation of the segments of the lower extremity in locomotion. J Bone Joint Surg. 1948;30:859–72.
Ferber R, McClay Davis I, Williams 3rd DS, Laughton C. A comparison of within- and between-day reliability of discrete 3D lower extremity variables in runners. J Orthop Res. 2002;20:1139–45.
Streiner DL, Norman GR. Health measurement scales : a practical guide to their development and use. New York: Oxford University Press; 2003.
Goujon H, Bonnet X, Sautreuil P, Maurisset M, Darmon L, Fode P, et al. A functional evaluation of prosthetic foot kinematics during lower-limb amputee gait. Prosthet Orthot Int. 2006;30:213–23.
Houck J, Yack HJ, Cuddeford T. Validity and comparisons of tibiofemoral orientations and displacement using a femoral tracking device during early to mid stance of walking. Gait Posture. 2004;19:76–84.
Marin F, Allain J, Diop A, Maurel N, Simondi M, Lavaste F. On the estimation of knee joint kinematics. Hum Mov Sci. 1999;18:613–26.
Sati M, de Guise JA, Larouche S, Drouin G. Improving in vivo knee kinematic measurements: application to prosthetic ligament analysis. Knee. 1996;3:179–90.
Ganjikia S, Duval N, Yahia LH, de Guise J. Three-dimensional knee analyzer validation by simple fluoroscopic study. Knee. 2000;7:221–31.
Labbe DR, de Guise JA, Godbout V, Grimard G, Baillargeon D, Lavigne P, et al. Accounting for velocity of the pivot shift test manoeuvre decreases kinematic variability. Knee. 2011;18(2):88–93.
Kinzel GL, Gutkowski LJ. Joint models, degrees of freedom, and anatomical motion measurement. J Biomech Eng. 1983;105:55–62.
Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–44.
Kinzel GL, Hall Jr AS, Hillberry BM. Measurement of the total motion between two body segments. I analytical development. J Biomech. 1972;5:93–105.
Cappozzo A. Gait analysis methodology. Hum Mov Sci. 1984;3:27–50.
Hagemeister N, Parent G, Van de Putte M, St-Onge N, Duval N, de Guise J. A reproducible method for studying three-dimensional knee kinematics. J Biomech. 2005;38:1926–31.
Siston RA, Delp SL. Evaluation of a new algorithm to determine the hip joint center. J Biomech. 2006;39:125–30.
Lam MH, Fong DT, Yung P, Ho EP, Chan WY, Chan KM. Knee stability assessment on anterior cruciate ligament injury: clinical and biomechanical approaches. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:20.
Wexler G, Hurwitz DE, Bush-Joseph CA, Andriacchi TP, Bach BR Jr. Functional gait adaptations in patients with anterior cruciate ligament deficiency over time. Clin Orthop. 1998:166–75.
Andriacchi TP, Briant PL, Bevill SL, Koo S. Rotational changes at the knee after ACL injury cause cartilage thinning. Clin Orthop Relat Res. 2006;442:39–44.
Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech. 2005;38:293–8.
Georgoulis AD, Papadonikolakis A, Papageorgiou CD, Mitsou A, Stergiou N. Three-dimensional tibiofemoral kinematics of the anterior cruciate ligament-deficient and reconstructed knee during walking. Am J Sports Med. 2003;31:75–9.
Knoll Z, Kocsis L, Kiss RM. Gait patterns before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12:7–14.
Torry MR, Decker MJ, Ellis HB, Shelburne KB, Sterett WI, Steadman JR. Mechanisms of compensating for anterior cruciate ligament deficiency during gait. Med Sci Sports Exerc. 2004;36:1403–12.
Alkjaer T, Simonsen EB, Jorgensen U, Dyhre-Poulsen P. Evaluation of the walking pattern in two types of patients with anterior cruciate ligament deficiency: copers and non-copers. Eur J Appl Physiol. 2003;89:301–8.
Berchuck M, Andriacchi TP, Bach BR, Reider B. Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am. 1990;72:871–7.
Bulgheroni P, Bulgheroni MV, Andrini L, Guffanti P, Castelli C. Walking in anterior cruciate ligament injuries. Knee. 1997;4:159–65.
Perry J. Gait analysis: normal and pathological function. Thorofare: SLACK Incorporated; 1992.
Whittle MW. Gait analysis: an introduction. Edinburgh/Toronto: Butterworth Heinemann Elsevier; 2007.
Chau T, Young S, Redekop S. Managing variability in the summary and comparison of gait data. J Neuroeng Rehabil. 2005;2:22.
Vaughan CL. Are joint torques the Holy Grail of human gait analysis ? Hum Mov Sci. 1996;15:423–43.
Andriacchi TP. Dynamics of pathological motion: applied to the anterior cruciate deficient knee. J Biomech. 1990;23 Suppl 1:99–105.
Roberts CS, Rash GS, Honaker JT, Wachowiak MP, Shaw JC. A deficient anterior cruciate ligament does not lead to quadriceps avoidance gait. Gait Posture. 1999;10:189–99.
Hurd WJ, Snyder-Mackler L. Knee instability after acute ACL rupture affects movement patterns during the mid-stance phase of gait. J Orthop Res. 2007;25:1369–77.
Noyes FR, Schipplein OD, Andriacchi TP, Saddemi SR, Weise M. The anterior cruciate ligament-deficient knee with varus alignment. An analysis of gait adaptations and dynamic joint loadings. Am J Sports Med. 1992;20:707–16.
Patel RR, Hurwitz DE, Bush-Joseph CA, Bach B, Andriacchi TP. Comparison of clinical and dynamic knee function in patients with anterior cruciate ligament deficiency. Am J Sports Med. 2003;31:68–74.
Rudolph KS, Eastlack ME, Axe MJ, Snyder-Mackler L. Basmajian Student Award Paper: movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;8:349–62.
Beard DJ, Soundarapandian RS, O’Connorc JJ, Dodd CA. Gait and electromyographic analysis of anterior cruciate ligament deficient subjects. Gait Posture. 1996;4:83–8.
Boerboom AL, Hof AL, Halbertsma JP, van Raaij JJ, Schenk W, Diercks RL, et al. Atypical hamstrings electromyographic activity as a compensatory mechanism in anterior cruciate ligament deficiency. Knee Surg Sports Traumatol Arthrosc. 2001;9:211–6.
Rudolph KS, Axe MJ, Buchanan TS, Scholz JP, Snyder-Mackler L. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9:62–71.
Ferber R, Osternig LR, Woollacott MH, Wasielewski NJ, Lee JH. Gait mechanics in chronic ACL deficiency and subsequent repair. Clin Biomech (Bristol, Avon). 2002;17:274–85.
Hart JM, Ko JW, Konold T, Pietrosimione B. Sagittal plane knee joint moments following anterior cruciate ligament injury and reconstruction: a systematic review. Clin Biomech (Bristol, Avon). 2010;25(4):277–83.
Dumas R, Aissaoui R, de Guise JA. A 3D generic inverse dynamic method using wrench notation and quaternion algebra. Comput Methods Biomech Biomed Engin. 2004;7:159–66.
Bulgheroni P, Bulgheroni MV, Andrini L, Guffanti P, Giughello A. Gait patterns after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1997;5:14–21.
Gao B, Zheng NN. Alterations in three-dimensional joint kinematics of anterior cruciate ligament-deficient and -reconstructed knees during walking. Clin Biomech (Bristol, Avon). 2010;25:222–9.
Lewek MD, Chmielewski TL, Risberg MA, Snyder-Mackler L. Dynamic knee stability after anterior cruciate ligament rupture. Exerc Sport Sci Rev. 2003;31:195–200.
Papadonikolakis A, Cooper L, Stergiou N, Georgoulis AD, Soucacos PN. Compensatory mechanisms in anterior cruciate ligament deficiency. Knee Surg Sports Traumatol Arthrosc. 2003;11:235–43.
Beynnon BD, Fleming BC, Labovitch R, Parsons B. Chronic anterior ligament deficiency is associated with increased anterior translation of tibia during the transition from non-weightbearing to weightbearing. J Orthop Res. 2002;20:332–7.
Marans HJ, Jackson RW, Glossop ND, Young C. Anterior cruciate ligament insufficiency: a dynamic three-dimensional motion analysis. Am J Sports Med. 1989;17:325–32.
Ellison AE. The pathogenesis and treatment of anterolateral rotatory instability. Clin Orthop Relat Res. 1980:51–5.
Scholten RJ, Opstelten W, van der Plas CG, Bijl D, Deville WL, Bouter LM. Accuracy of physical diagnostic tests for assessing ruptures of the anterior cruciate ligament: a meta-analysis. J Fam Pract. 2003;52:689–94.
Katz JW, Fingeroth RJ. The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries. Am J Sports Med. 1986;14:88–91.
Kim SJ, Kim HK. Reliability of the anterior drawer test, the pivot shift test, and the Lachman test. Clin Orthop Relat Res. 1995:237–42.
Liu SH, Osti L, Henry M, Bocchi L. The diagnosis of acute complete tears of the anterior cruciate ligament. Comparison of MRI, arthrometry and clinical examination. J Bone Joint Surg Br. 1995;77:586–8.
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:629–34.
Eastlack ME, Axe MJ, Snyder-Mackler L. Laxity, instability, and functional outcome after ACL injury: copers versus noncopers. Med Sci Sports Exerc. 1999;31:210–5.
Lephart SM, Perrin DH, Fu FH, Gieck JH, McCue FC, Irrgang JJ. Relationship between selected physical characteristics and functional capacity in the anterior cruciate ligament-insufficient athlete. J Orthop Sports Phys Ther. 1992;16:174–81.
Engstrom B, Gornitzka J, Johansson C, Wredmark T. Knee function after anterior cruciate ligament ruptures treated conservatively. Int Orthop. 1993;17:208–13.
Pollet V, Barrat D, Meirhaeghe E, Vaes P, Handelberg F. The role of the Rolimeter in quantifying knee instability compared to the functional outcome of ACL-reconstructed versus conservatively-treated knees. Knee Surg Sports Traumatol Arthrosc. 2005;13:12–8.
Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5-9 years after surgery. Acta Orthop Scand. 2004;75:594–9.
Tamea Jr CD, Henning CE. Pathomechanics of the pivot shift maneuver. An instant center analysis. Am J Sports Med. 1981;9:31–7.
Leitze Z, Losee RE, Jokl P, Johnson TR, Feagin JA. Implications of the pivot shift in the ACL-deficient knee. Clin Orthop Relat Res. 2005:229–36.
Galway HR, MacIntosh DL. The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res. 1980:45–50.
Hefti E, Müller W, Jakob R, Stäubli H. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–34.
Lane CG, Warren R, Pearle AD. The pivot shift. J Am Acad Orthop Surg. 2008;16:679–88.
Noyes FR, Grood ES, Cummings JF, Wroble RR. An analysis of the pivot shift phenomenon. The knee motions and subluxations induced by different examiners. Am J Sports Med. 1991;19:148–55.
Amis AA, Cuomo P, Siva Rama RB, Giron F, Bull AM, Thomas R, et al. Measurement of knee laxity and pivot-shift kinematics with magnetic sensors. Oper Techn Orthop. 2008;18:8.
Kubo S, Muratsu H, Yoshiya S, Mizuno K, Kurosaka M. Reliability and usefulness of a new in vivo measurement system of the pivot shift. Clin Orthop Relat Res. 2007;454:54–8.
Bull AM, Earnshaw PH, Smith A, Katchburian MV, Hassan AN, Amis AA. Intraoperative measurement of knee kinematics in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2002;84:1075–81.
Hoshino Y, Kuroda R, Nagamune K, Yagi M, Mizuno K, Yamaguchi M, et al. In vivo measurement of the pivot-shift test in the anterior cruciate ligament-deficient knee using an electromagnetic device. Am J Sports Med. 2007;35:1098–104.
Lopomo N, Zaffagnini S, Bignozzi S, Visani A, Marcacci M. Pivot-shift test: Analysis and quantification of knee laxity parameters using a navigation system. J Orthop Res. 2010;28:164–9.
Lane CG, Warren RF, Stanford FC, Kendoff D, Pearle AD. In vivo analysis of the pivot shift phenomenon during computer navigated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16:487–92.
Labbe DR, de Guise JA, Mezghani N, Godbout V, Grimard G, Baillargeon D, et al. Feature selection using a principal component analysis of the kinematics of the pivot shift phenomenon. J Biomech. 2010;43(16):3080–4.
Labbe DR, de Guise JA, Mezghani N, Godbout V, Grimard G, Baillargeon D, et al. Objective grading of the pivot shift phenomenon using a support vector machine approach. J Biomech. 2011;44(1):1–5.
Ho R. Handbook of univariate and multivariate data analysis and interpretation with SPSS. Chapman: Chapman & Hall/CRC; 2006.
Chan YY, Fong DT, Chung MM, Li WJ, Liao WH, Yung PS, et al. Identification of ankle sprain motion from common sporting activities by dorsal foot kinematics data. J Biomech. 2010;43:1965–9.
Lauer RT, Smith BT, Betz RR. Application of a neuro-fuzzy network for gait event detection using electromyography in the child with cerebral palsy. IEEE Trans Biomed Eng. 2005;52:1532–40.
Giansanti D, Macellari V, Maccioni G. New neural network classifier of fall-risk based on the Mahalanobis distance and kinematic parameters assessed by a wearable device. Physiol Meas. 2008;29:N11–9.
Lau HY, Tong KY, Zhu H. Support vector machine for classification of walking conditions of persons after stroke with dropped foot. Hum Mov Sci. 2009;28:504–14.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Andriacchi TP, Mundermann A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr Opin Rheumatol. 2006;18:514–8.
Scarvell JM, Smith PN, Refshauge KM, Galloway HR, Woods KR. Association between abnormal kinematics and degenerative change in knees of people with chronic anterior cruciate ligament deficiency: a magnetic resonance imaging study. Aust J Physiother. 2005;51:233–40.
Peeler J, Leiter J, MacDonald P. Accuracy and reliability of anterior cruciate ligament clinical examination in a multidisciplinary sports medicine setting. Clin J Sport Med. 2010;20:80–5.
Acknowledgments
The authors would like to acknowledge the participation of the clinicians in the different studies presented in this chapter: Dr Tim Heron and Dr Véronique Godbout, University hospital of University of Montreal, Dr Patrick Lavigne, Maisonneuve-Rosemont Hospital, Dr Guy Grimard, Ste-Justine Hospital, Dr Pierre Ranger and Dr Julio Fernandes, Sacré-Coeur Hospital and Dr David Baillargeon, Cité de la santé, Montréal.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer-Verlag London
About this chapter
Cite this chapter
Labbe, D.R., Fuentes, A., de Guise, J.A., Aissaoui, R., Hagemeister, N. (2016). Three-Dimensional Biomechanical Assessment of Knee Ligament Ruptures. In: Poitout, D. (eds) Biomechanics and Biomaterials in Orthopedics. Springer, London. https://doi.org/10.1007/978-1-84882-664-9_39
Download citation
DOI: https://doi.org/10.1007/978-1-84882-664-9_39
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-84882-663-2
Online ISBN: 978-1-84882-664-9
eBook Packages: MedicineMedicine (R0)