Abstract
Purpose
Although the occurrence of early osteoarthritis (OA) is commonly associated with a history of anterior cruciate ligament (ACL) reconstruction, its exact prevalence in these patients remains unknown. The goal of this study was to review the current literature on long-term radiographic outcome after autologous ACL reconstruction and subsequently perform a meta-analysis to obtain evidence-based prevalences of OA at a mean of 10 years after surgery. In addition, this report aimed at identifying the relationship between meniscal status and the occurrence of radiographic OA in the ACL reconstructed knee.
Methods
A systematic review of the literature was performed in PubMed MEDLINE, EMBASE and Cochrane Library databases to identify all studies concerning radiographic outcome after autologous ACL reconstruction with a follow-up of minimum 10 years. Meta-analyses were performed to obtain the average prevalence of OA and the difference between patients with and without meniscectomy. Considered study estimates were the log-transformed odds and odds ratios, the latter expressing the effect of meniscectomy on OA.
Results
A total of 16 studies could be included for meta-analysis, accounting for 1554 ACL reconstructions performed between 1978 and 1997. Of these knees, 453 (28 %) showed radiological signs of osteoarthritis (IKDC grade C or D). Furthermore, 50 % of the patients with meniscectomy had osteoarthritis, compared with 16 % of the patients without meniscectomy. The combined odds ratio for meniscectomy equals 3.54 (95 % CI 2.56–4.91).
Conclusions
The main finding of this meta-analysis is that the prevalence of radiographic knee OA after ACL reconstruction is lower than commonly perceived. However, associated meniscal resection dramatically increases the risk for developing OA.
Level of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The occurrence of osteoarthritis (OA) is often thought as a near-inevitable consequence after anterior cruciate ligament (ACL) injury, with prevalences of 50–80 % reported a decade after the initial trauma [24, 49]. ACL injuries often present with associated knee lesions: a concomitant meniscal tear is seen in 25–65 % of the cases, while chondral lesions have been noted in approximately 25 % of the ACL-injured knees at the time of initial presentation [26]. Whereas most authors agree on the deleterious effect of a (partial) meniscectomy with regard to the premature development of osteoarthritis (OA) after ACL reconstruction [5, 27], the role of chondral injuries sustained during the index trauma is less clear. Shelbourne et al. [48] found no difference in OA prevalences in a group of subjects presenting with chondral injuries at the time of ACL reconstruction compared to a control group without cartilage lesions.
Since long, however, ACL tears are often quoted as being responsible for a large percentage of the “young patients with old knees” [24, 50]. Although surgical ACL reconstruction using tendon grafts has become the current standard of care to treat the functionally unstable ACL-deficient knee [49], controversy remains to exist regarding the effect of ACL reconstruction on the development of knee OA in this generally young population. Current literature contains a number of reports suggesting that the prevalence of OA remains unchanged whether or not the ACL is surgically reconstructed [20, 25], but Daniel et al. [7] even detected an increased incidence of OA in the ACL reconstructed group. On the other end of the spectrum, some authors seem to maintain excellent results a decade after ACL reconstruction, with reported OA prevalences of 2–3 % [20, 40].
As current controversy on the occurrence of OA after ACL reconstruction has been fuelled by rather small, heterogeneous and retrospective case series and expert opinions [5, 25, 31, 32, 41, 43], the goal of this study was to compile and systematically review the current literature on long-term outcome after autologous ACL reconstruction and subsequently perform a meta-analysis to obtain evidence-based prevalences of (radiographic) OA. In addition, this manuscript aims at unravelling the relationship between meniscal status and the occurrence of OA in the ACL reconstructed knee.
Materials and methods
This meta-analysis was set up and reported according to the recommendations proposed by the PRISMA statement [33].
Search strategy
A systematic review of the literature was performed in order to identify all studies concerning the long-term outcome after autologous ACL reconstruction in the human knee. “Long-term” outcome was defined as a mean follow-up of minimum 10 years. The PubMed MEDLINE, EMBASE and Cochrane Library databases were searched from their earliest entry points to October 2010, including articles published online as “Epub ahead of print”. The computerized search was performed using combinations of the following search terms: “anterior cruciate ligament or ACL”, “reconstruction”, “autologous”, “treatment”, “long-term”, “outcome”, “follow-up”, “results” and “(osteo)arthritis or osteoarthrosis”.
Selection
Searches were limited to studies published in English and French. Studies reporting on long-term outcome after ACL reconstruction without radiographic evaluation were excluded. Reports with a mean follow-up less than 10 years were excluded as well. In addition, each reference list from the identified articles was manually checked to verify that relevant articles were not missed for the current review.
Data extraction
Each study was evaluated for the following variables: study type; mean follow-up after ACL reconstruction; operative technique; time period of surgery; number of patients with radiographs at final follow-up; number of patients with meniscectomy prior to, at the time of or after ACL reconstruction within this group; number of patients with radiographic OA of operated knee. Relevant data from each included study were extracted and recorded on multiple worksheets.
Osteoarthritis
The definition of OA in this meta-analysis was exclusively based on radiological criteria, due to the obvious lack of reported data combining both clinical and radiological aspects of OA. Furthermore, the presence of different radiological classification systems for OA used in the studied reports (e.g., Kellgren and Lawrence, Ahlbäck, Fairbanks, IKDC…) necessitated the development of a conversion method for the various OA scores in order to allow subsequent statistical analysis. Due to its widespread use and reliability [30], the “IKDC radiographic grading system” [14] was chosen as the reference classification to which other scores were translated to best effort (see Table 1). With regard to OA, IKDC grade A and B were considered as being normal or nearly normal
, while IKDC grades C and D were considered to represent OA of the knee.
Some studies reported on the presence of OA in either the medial or lateral tibiofemoral compartment or in the patellofemoral joint, but most authors did not specify the localization of the degenerative changes. Therefore, it was decided to pool all available data in one general group of “knee OA”.
Meniscectomy
Many included reports mention a subpopulation of meniscectomized patients at final follow-up. The radiographic outcome of this subset of patients was studied separately in order to evaluate the impact of meniscectomy on the prevalence of OA. Although some authors specify the location of the meniscal resection, that is, in the medial or lateral compartment and most of them do not elaborate on the amount of meniscal resection, for the purpose of this meta-analysis all patients who underwent partial or total meniscectomy prior, at the time of or after surgery, were pooled together. Subjects treated with meniscal repair were appointed to the non-meniscectomy group, unless failure of the suture was reported during follow-up.
Statistical analysis
Meta-analyses were performed to obtain the average prevalence of OA and the difference between patients with and without meniscectomy. Considered study estimates are the log-transformed OA odds and odds ratios (and risk ratios), the latter expressing the effect of meniscectomy on OA. Differences between studies reflect true variability (“heterogeneity”) and sampling variability. Heterogeneity was quantified by the I² statistic [16], which is the percentage of total variation in study estimates that is due to heterogeneity and tested by Cochran’s χ²-test. The random-effects approach of DerSimonian and Laird [8] was used to take into account the heterogeneity in the combination of the results of the studies. A random-effects meta-regression [51] with the average length of follow-up per study is used to evaluate the relation with OA and to verify whether the effect of meniscectomy on OA depends on the average length of follow-up reported in the specific study. To illustrate the between-study heterogeneity, the observed proportion OA per study was plotted versus the number of patients in funnel plots with 99 % prediction limits around the overall proportion OA. These limits indicate the range wherein 99 % of the observed proportions are expected, if there were no heterogeneity. Prediction limits were constructed based on the binomial distribution with a continuity correction. P values smaller than 0.05 are considered significant. All analyses have been performed using SAS software, version 9.2 of the SAS System for Windows (SAS Institute Inc., Cary, NC, USA).
Results
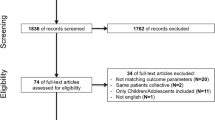
The computerized search using the aforementioned search terms delivered 211 studies describing outcome after ACL reconstruction. Abstracts and, if necessarily, full text articles were studied to detect the mean duration of follow-up. In this manner, 39 studies considering ACL injury (i.e., treated and non-treated) with a mean follow-up of more than 10 years were identified. After the exclusion of articles on conservative treatment, primary ACL repair (i.e., suture), isolated extra-articular, allograft and synthetic reconstructions, 24 studies could be withheld for in-depth analysis. Subsequently, 3 studies were excluded due to the presence of biasing concomitant surgical procedures in the ACL reconstructed knees (i.e., meniscal allograft transplantation and high tibial osteotomy). Two studies by the same research group [2, 4] were excluded because a later published report described the identical patient population with longer follow-up and was conversely included [39]. Unfortunately, another 3 manuscripts were excluded due to inaccurate or incomplete reporting on patient numbers or OA criteria at final follow-up [28, 52, 53]. Finally, 16 reports could be included for systematic review and meta-analysis [5, 9, 11, 15, 20–22, 25, 31, 32, 38–40, 43, 46, 47]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram [33, 34] depicts the number of studies identified, included and excluded as well as the reasons for exclusion (see Fig. 1).
The preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram17, depicting the number of studies identified, included and excluded as well as the reasons for exclusion. *Records excluded because mean follow-up equalled less than 10 years, or no radiographic analysis performed. †Reasons for exclusion of articles: conservative treatment, primary repair, isolated extra-articular reconstruction, synthetic or allograft reconstruction, presence of biasing concomitant procedures (i.e., osteotomy or meniscal allograft transplantation
Study characteristics
A total number of 1554 subjects could be included in this review. This number represents all patients available for radiographic examination at the time of follow-up, not at inclusion. Subjects per study ranged from 25 to 502 and mean follow-up ranged from 10 to 24.5 years, and 11 out of the 16 included papers had a mean follow-up between 10 and 12 years. One study exclusively studied female subjects [25], while another had a male/female ratio of 55/3 [46]. The effect of gender on long-term outcome after ACL reconstruction could not be assessed because the vast majority of papers did not publish separate results for male and female subjects. The presence or absence of associated meniscal lesions necessitating resection before, during, or after ACL reconstruction was mentioned in 11 out of 16 included articles, accounting for a total of 614 meniscectomized subjects on a total of 1264 (48.6 %). Only 5 of the included reports were set up as a prospective study, with the remaining 11 studies being retrospective in nature. The main study characteristics are summarized in Table 2.
Prevalence of osteoarthritis and relation with meniscectomy
The combined estimate for the prevalence of OA (IKDC C or D) from the random-effects meta-analysis on 1554 included knees equals 27.9 % (95 % CI 16.3–43.5 %). There is, however, a large amount of heterogeneity between the studies in the reported percentage of OA (see funnel plot Fig. 2), with >90 % of the variation being due to between-study heterogeneity, (I² = 95.8 %). Although there is a strong link between meniscectomy and OA, >90 % of the variation in separate analyses on patients with and without meniscectomy is attributable to between-study heterogeneity (I² = 92.7 and 95.3 %, respectively) (see Figs. 3, 4). Further, a meta-regression reveals that there is no evidence for a relation between OA and average length of follow-up, with the odds ratio (OR) expressing the effect of 1-year increase on the odds for OA equals 1.07 (95 % CI 0.89–1.30, p = n.s.). It should be noted, however, that the range of values for the average follow-up is restricted: 11 of the 16 included studies have an average length of FU between 10 and 12 years.
The combined estimate for the prevalence of OA from the random-effects meta-analysis equals 16.4 % (95 % CI 7.0–33.9 %) in patients without meniscectomy and 50.4 % (95 % CI 27.4–73.1 %) in patients with meniscectomy. The combined odds ratio equals 3.54 (95 % CI 2.56–4.91), meaning that the odds for having OA is 3.54 times higher after meniscectomy. The forest plot (see Fig. 5) reveals that the effect estimates range in the same order of magnitude.
Discussion
The major finding of this study is that the prevalence of OA after ACL reconstruction is probably lower than commonly thought. The purpose of this meta-analysis was to compile all available evidence on long-term radiographic outcome after ACL reconstruction, as to date controversy remains to exist due to a number of dispersed, heterogeneous retrospective case series and expert opinions. From the early days on, ACL rupture has been linked with the occurrence of premature OA in the injured knee [13, 17, 29]. Remarkably, contemporary ACL reconstruction techniques have not been able to change this common belief. Indeed, many still consider early OA as an almost inevitable consequence of ACL reconstruction, with reported OA prevalences between 50 and 100 % [18, 23]. This first-ever meta-analysis on ACL reconstruction and OA shows that the use of these dramatically high prevalences is not justifiable on the basis of the available evidence in current literature. On the contrary, our results indicate that the prevalence of knee OA after ACL reconstruction is significantly lower than commonly perceived. Indeed, the combined estimate from the random-effects meta-analysis equals 28 %, and the upper limit of the 95 % CI for this estimate is lower than 50 % (43.5 %). In this view, our results are in line with a recent systematic review on this topic by Oiestad et al. [37], stating that “we should discontinue reporting that subjects with ACL injury have a prevalence of knee OA between 50 and 100 %”. However, that paper was a systematic review on long-term outcome after ACL injury, not ACL reconstruction, thus pooling the results of patients who were either conservatively or surgically treated (by a variety of techniques and grafts). By ranking the included papers on the basis of their respective modified Coleman Methodological Score (CMS) [6], the highest rated studies reported low prevalence of knee OA for individuals with isolated ACL injury (0–13 %) and a prevalence of knee OA between 21 and 48 % for subjects with combined injuries [37].
The question remains: can ACL reconstruction prevent the occurrence of early OA? To date, a direct proof to confirm or reject this statement stays difficult to deliver. One of the main issues in this debate is the lack of controlled, prospective studies on the long-term natural history of the ACL-deficient knee. The advent of modern ACL reconstruction in the 1980s was merely driven by the superior short- and mid-term results with regard to stability and knee function when compared to non-operative treatment. However, some early reports on conservative ACL treatment had already shown unfavourable long-term results with very high rates (i.e., 60–90 %) of early OA in the ACL-deficient knee. [3, 17, 45] To the contrary, other authors have reported much better functional and radiographic results after non-operative treatment. For example, Neumann et al. [36] treated ACL-injured patients with activity modification and physical therapy and reported a prevalence of only 15 % OA at 15 years of follow-up. The true natural history of these injuries may never be known due to the existence of asymptomatic ACL-deficient subjects or so-called copers, patient selection bias, or conservative treatment heterogeneity in published reports.
Additionally, this meta-analysis confirmed that meniscectomy should be considered as an important risk factor for developing OA after ACL reconstruction, with 42 % of patients showing radiographic OA compared to 19 % of patients with a preserved meniscal status (OR = 3.54). Recent cadaveric experiments by Musahl et al. [35] have confirmed the secondary stabilizing effect of both the medial and lateral meniscus in the ACL-deficient knee. These authors showed that the medial meniscus functions as an important secondary restraint to anterior tibial translation in the ACL-deficient knee (i.e., during the Lachman test), while the lateral meniscus has a relatively more important secondary restraining role to the combined axial and rotatory loads (i.e., during the pivot-shift examination). In this view, anterior or rotatory instability in the absence of a functional ACL results in excess shearing forces being applied at the meniscus, thus giving rise to meniscal damage, degenerative tears and pain necessitating resection of the meniscus. Most authors have reported higher rates of subsequent meniscal injuries after conservatively managed ACL ruptures when compared to ACL reconstructed knees, with incidences as high as 98 % in chronic ACL-deficient knees [18, 20]. Even in a recent RCT published in the New England Journal of Medicine questioning the need for prompt ACL reconstructive surgery [12], the conservatively treated cohort experienced 33 % more meniscal tears after the ACL injury. As this meta-analysis has clearly identified meniscectomy as the risk factor of utmost importance with regard to the development of early OA, the occurrence of OA can be directly related to the inability of the ACL-injured knee to protect its menisci. In other words, this meta-analysis supports the statement that “the key to lowering the risk of knee OA is decreasing the rate of meniscectomy” [42].
The limitations of this meta-analysis are as follows:
-
1.
One could argue that the existence of cartilage lesions at the time of ACL reconstruction is not taken into account in this meta-analysis, thus probably compromising interpretation of the results. Let alone the fact that the prevalence of chondral injuries at the time of ACL reconstruction is rarely reported in the included reports, multiple authors previously have not been able to find a correlation between an osteochondral injury diagnosed at primary arthroscopy after ACL injury and subsequent knee OA [36, 48].
-
2.
As stated before, a major difficulty arises when comparing long-term outcome studies after ACL reconstruction with regard to the varying OA classifications used in these reports. In order to facilitate meta-analysis, the Ahlbäck [1], Kellgren and Lawrence [19] and modified Fairbank[10] classifications were all translated into the IKDC radiographic grading [14], to the best effort. A particular difficulty arose with the interpretation of the K&L classification, especially with the description of K&L grade II, which has been notoriously inexact, due to initial description of the developers [44]. We decided, in accordance with Meuffels et al. [31] and Oiestad et al. [38] to consider K&L grade II as “osteoarthritis” (i.e., IKDC grade C), unless explicitly stated otherwise in the individual report.
-
3.
There is a considerable amount of variability between the studies in the reported prevalences of OA. The formal analysis and the funnel plot indicate that this variability largely exceeds the sampling variability, that is, reflects true differences (heterogeneity) between the studies, both in the combined group (all subjects irrespective of meniscectomy) and the subgroups.
Conclusion
In conclusion, this meta-analysis on the relation between ACL reconstruction and the development of OA has shown that the prevalence of OA is definitely lower than commonly perceived. However, associated meniscal resection dramatically increases the risk for developing OA (OR 3.54). This finding bears the inherent consequence of attempting a repair of meniscus injuries sustained at the time of ACL tear, as well as contemplating reconstruction of the ruptured ACL in order to protect the menisci from excessive shear forces, subsequent tearing and the premature development of OA. Moreover, in an era of questioning the cost-effectiveness of surgical procedures, the results of this study have the potential to justify current clinical practice regarding ACL-injured subjects. Finally, these results should be used as a baseline for upcoming long-term outcome studies on recent ACL techniques and to counsel ACL-injured patients in an evidence-based way.
References
Ahlback S (1968) Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 277(Suppl):272–277
Ait SST, Fithian D, Neyret P (2006) The evolution of osteoarthritis in 103 patients with ACL reconstruction at 17 years follow-up. Knee 13(5):353–358
Barrack RL, Bruckner JD, Kneisl J, Inman WS, Alexander AH (1990) The outcome of nonoperatively treated complete tears of the anterior cruciate ligament in active young adults. Clin Orthop Relat Res 259:192–199
Chol C, Ait SST, Chambat P, Dejourdagger H, Neyret P (2002) Seventeen year outcome after anterior cruciate ligament reconstruction with a intact or repaired medial meniscus. Rev Chir Orthop Reparatrice Appar Mot 88(2):157–162
Cohen M, Amaro JT, Ejnisman B, Carvalho RT, Nakano KK, Peccin MS, Teixeira R, Laurino CF, Abdalla RJ (2007) Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy 23(6):629–634
Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD (2000) Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 10(1):2–11
Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR (1994) Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med 22(5):632–644
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Drogset JO, Grontvedt T, Robak OR, Molster A, Viset AT, Engebretsen L (2006) A sixteen-year follow-up of three operative techniques for the treatment of acute ruptures of the anterior cruciate ligament. J Bone Joint Surg Am 88(5):944–952
Fairbank TJ (1948) Knee joint changes after meniscectomy. J Bone Joint Surg Br 30B(4):664–670
Fink C, Hoser C, Hackl W, Navarro RA, Benedetto KP (2001) Long-term outcome of operative or nonoperative treatment of anterior cruciate ligament rupture–is sports activity a determining variable? Int J Sports Med 22(4):304–309
Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS (2010) A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 363(4):331–342
Funk FJ Jr (1983) Osteoarthritis of the knee following ligamentous injury. Clin Orthop Relat Res 172:154–157
Hefti F, Muller W, Jakob RP, Staubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1(3–4):226–234
Hertel P, Behrend H, Cierpinski T, Musahl V, Widjaja G (2005) ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg Sports Traumatol Arthrosc 13(4):248–255
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Kannus P, Jarvinen M (1987) Conservatively treated tears of the anterior cruciate ligament. Long-term results. J Bone Joint Surg Am 69(7):1007–1012
Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC (2010) Factors involved in the development of osteoarthritis after anterior cruciate ligament surgery. Am J Sports Med 38(3):455–463
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS (2008) Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 16(5):442–448
Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C (2008) Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone autograft: a minimum 10-year follow-up. Am J Sports Med 36(7):1275–1282
Lerat JL, Chotel F, Besse JL, Moyen B, Binet G, Craviari T, Brunet-Guedj E, Adeleine P, Nemoz JC (1998) The results after 10–16 years of the treatment of chronic anterior laxity of the knee using reconstruction of the anterior cruciate ligament with a patellar tendon graft combined with an external extra-articular reconstruction. Rev Chir Orthop Reparatrice Appar Mot 84(8):712–727
Li RT, Lorenz S, Xu Y, Harner CD, Fu FH, Irrgang JJ (2011) Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. Am J Sports Med 39(12):2595–2603
Lohmander LS, Englund PM, Dahl LL, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35(10):1756–1769
Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50(10):3145–3152
Louboutin H, Debarge R, Richou J, Selmi TA, Donell ST, Neyret P, Dubrana F (2009) Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee 16(4):239–244
Magnussen RA, Mansour AA, Carey JL, Spindler KP (2009) Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg 22(4):347–357
Marcacci M, Zaffagnini S, Giordano G, Iacono F, Presti ML (2009) Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: A prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med 37(4):707–714
McDaniel WJ Jr, Dameron TB Jr (1980) Untreated ruptures of the anterior cruciate ligament. A follow-up study. J Bone Joint Surg Am 62(5):696–705
Mehta VM, Paxton LW, Fornalski SX, Csintalan RP, Fithian DC (2007) Reliability of the international knee documentation committee radiographic grading system. Am J Sports Med 35(6):933–935
Meuffels DE, Favejee MM, Vissers MM, Heijboer MP, Reijman M, Verhaar JA (2009) Ten year follow-up study comparing conservative versus operative treatment of anterior cruciate ligament ruptures. A matched-pair analysis of high level athletes. Br J Sports Med 43(5):347–351
Meystre JL, Vallotton J, Benvenuti JF (1998) Double semitendinosus anterior cruciate ligament reconstruction: 10-year results. Knee Surg Sports Traumatol Arthrosc 6(2):76–81
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012
Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38(8):1591–1597
Neuman P, Englund M, Kostogiannis I, Friden T, Roos H, Dahlberg LE (2008) Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury: a prospective cohort study. Am J Sports Med 36(9):1717–1725
Oiestad BE, Engebretsen L, Storheim K, Risberg MA (2009) Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med 37(7):1434–1443
Oiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, Fosdahl MA, Risberg MA (2010) Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 38(11):2201–2210
Pernin J, Verdonk P, Si STA, Massin P, Neyret P (2010) Long-term follow-up of 245 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med 38(6):1094–1102
Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J (2007) A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med 35(4):564–574
Reider B (2009) ACL & OA. Am J Sports Med 37(7):1279–1281
Richmond JC, Lubowitz JH, Poehling GG (2011) Prompt operative intervention reduces long-term osteoarthritis after knee anterior cruciate ligament tear. Arthroscopy 27(2):149–152
Salmon LJ, Russell VJ, Refshauge K, Kader D, Connolly C, Linklater J, Pinczewski LA (2006) Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med 34(5):721–732
Schiphof D, Boers M, Bierma-Zeinstra SM (2008) Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis 67(7):1034–1036
Segawa H, Omori G, Koga Y (2001) Long-term results of non-operative treatment of anterior cruciate ligament injury. Knee 8(1):5–11
Seon JK, Song EK, Park SJ (2006) Osteoarthritis after anterior cruciate ligament reconstruction using a patellar tendon autograft. Int Orthop 30(2):94–98
Shelbourne KD, Gray T (2009) Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med 37(3):471–480
Shelbourne KD, Jari S, Gray T (2003) Outcome of untreated traumatic articular cartilage defects of the knee: a natural history study. J Bone Joint Surg Am 85-A(Suppl 2):8–16
Spindler KP, Wright RW (2008) Clinical practice. Anterior cruciate ligament tear. N Engl J Med 359(20):2135–2142
Torg JS, Conrad W, Kalen V (1976) Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med 4(2):84–93
van Houwelingen HC, Arends LR, Stijnen T (2002) Advanced methods in meta-analysis: multivariate approach and meta-regression. Stat Med 21(4):589–624
von Porat A, Roos EM, Roos H (2004) High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis 63(3):269–273
Wu WH, Hackett T, Richmond JC (2002) Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: a long-term prospective study. Am J Sports Med 30(6):845–850
Acknowledgments
The authors would like to express their gratitude towards Steffen Fieuws from the Biostatistics and Statistical Bioinformatics Centre of the KULeuven for his expertise and assistance in the statistical analysis of the data.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Claes, S., Hermie, L., Verdonk, R. et al. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc 21, 1967–1976 (2013). https://doi.org/10.1007/s00167-012-2251-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2251-8