Abstract
Since biomechanical studies have shown that the medial patellofemoral ligament (MPFL) is the main restraint against lateral patella displacement, reconstruction of the MPFL has become an accepted method of restoring patellofemoral stability and numerous techniques were described. Due to biomechanical examinations and clinical results, an anatomical double-bundle reconstruction of the “sail-like” MPFL is a reasonable method for achieving stability during complete extension and lower flexion degree. This method also serves to avoid rotation of the patella, providing immediate stability throughout the normal range of motion. However, until today, an aperture fixation technique at the patellar insertion with two bundles has not been described previously. This technique can provide an immediate stability to allow an early rehabilitation with full range of motion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The medial patellofemoral complex, consisting of the medial patellofemoral ligament (MPFL) and the medial patellotibial ligament, is the main passive stabiliser of the patellofemoral joint. Since it has been shown that rupture of the MPFL is the main pathological consequence of patellar dislocation [4], and biomechanical studies have demonstrated that the MPFL is the main restraint against lateral patellar displacement, reconstruction of the MPFL has become a widespread technique for restoration of patellofemoral stability. An additional reason that MPFL reconstruction became as popular is the fact that distal realignment procedures such as transfer of the tibial tuberosity or release at the lateral patellar retinaculum/capsule have provided inadequate restoration of patellofemoral stability in every patient, frequently leading to increased mediolateral instability, increased patellofemoral pressure or arthritic degeneration [5, 6].
Therefore, numerous techniques for reconstruction of the medial patellofemoral complex have been described with promising clinical results [8]. However, since it is known that a non-anatomical reconstruction of the MPFL can lead to non-physiologic patellofemoral loads and kinematics [1], the goal of a surgical intervention must be an anatomical reconstruction. Since the femoral insertion of the MPFL has been evaluated anatomically [1], biomechanically [14] and radiologically [12], the complications of increased patellofemoral pressure in flexion associated with non-anatomic femoral graft fixation that is too anterior/proximal [1] can be avoided. Upon careful observation of the anatomical shape of the original MPFL, it is apparent that the patellar insertion is much wider than the femoral one. Additionally, Amis et al. have proven double-bundle structure provides a more stable proximal and distal ligamentous structure [1]. Respecting this anatomic condition, a double-bundle reconstruction at the patellar side is reasonable to restore native ligamentous morphologic and biomechanical properties; moreover, this method lessens the patellar rotation during flexion—extension movement that may occur during single-bundle reconstruction. Under these conditions, the double-bundle reconstruction, described earlier [11] shows very satisfying clinical results. As we know from ACL reconstruction, direct anatomical/aperture fixation [2] provides the highest time-zero fixation by avoiding elongation of the graft or “bungee” effect, resulting in the possibility of early rehabilitation with full range of motion. In a similar manner, these concepts may be applied to MPFL reconstruction.
Although most of the actual surgical techniques utilise a free tendon graft to reconstruct the MPFL as the only method for anatomic double-bundle graft fixation, an all aperture fixation has not yet been described.
Recent studies have described an anatomical double-bundle reconstruction, using an aperture fixation at the femoral insertion [11, 15], while the patellar fixation remains relatively indirect resulting in the eventual risk of post-operative micromotion and subsequent loosening. Patellar graft fixation has been described with either an anchor system, attaching the graft into a bony rim [11] or by tying the attached graft sutures to each other at the lateral patellar edge [15]; however, this method may potentially result in graft slippage by degloving [2].
Until today, only one technique described anatomical patellar fixation by looping graft through bone tunnels without any additional fixation device [3]. This technique appears to produce stable fixation at the patella. However, in soft bone, a widening of the tunnel could occur in the long-term; moreover, in patients with a short gracilis graft, the tendon length may not be long enough to reach the anatomical femoral insertion.
The double-bundle technique described here offers an aperture fixation at the patella and the femur, providing a high initial stability on both insertions, resulting in improved bony ingrowth, and consequently, an earlier return to full range of motion.
Surgical technique
Harvesting and preparing of the gracilis tendon
After completion of the arthroscopy, a 2-cm-long oblique incision is performed at the pes anserinus. After incising the sartorius aponeurosis, the gracilis tendon is harvested and used as an autograft. The load to failure force of the Gracilis graft—even as a single bundle—exceeds the failure to load of the MPFL (208 N) [1]. The usable part of the tendon should be at least 18 cm long. After harvesting the tendon with the stripper and removing the muscle tissue, the doubled tendon diameter is determined and both ends are whip-stitched with an absorbable braided suture over a length of 15 mm.
Preparing the soft-tissue layer
A 2-cm skin incision is performed from the superomedial corner to the end of the medial margin of the patella, where the patellar MPFL insertion is located [9, 14] (Fig. 1). As the MPFL is situated central to the vastus medialis obliquus (VMO) in the second layer of the medial patellofemoral complex [9], the central part of the VMO is identified and a scissor is brought along to the medial femoral epicondyle in between the VMO and the joint capsule, cautiously avoiding any injury to the joint. After the opened scissors are removed, a right-angle clamp is brought into the separated layer and the tip is directed towards the skin in the area of the adductor tubercle, where the femoral MPFL insertion is located. Then a small longitudinal skin incision is performed over the tip in 30° knee flexion, the position where the graft will be finally fixed. Finally, in preparation for passing the final graft, a suture loop is inserted in between the second and the third layers using the right-angle clamp.
Preparing the femoral insertion site
To avoid non-physiological patellofemoral forces, the femoral MPFL insertion has to be very accurate. Therefore, a guide wire with an eyelet is placed slightly posterior to the midpoint of the medial epicondyle and the adductor tubercle and the entering point into the bone is marked with a clamp [9]. Then the guide-wire placement is controlled by a picture intensifier on a straight lateral view to obtain the correct anatomical femoral insertion; if the graft is placed too anterior or proximal, abnormal graft tensioning will lead to increased patellofemoral pressures during flexion [1]. Therefore, we use the radiographic landmark of the anatomical MPFL insertion which has been shown to be located slightly anterior to an elongation of the posterior femoral cortex in between the proximal origin of the medial condyle and the most posterior point of Blumensaat’s line [11]. If necessary, the guide-wire entry point is corrected before overdrilling to the contralateral cortex with a drill diameter 1 mm larger than that of the graft loop.
Preparing the patellar insertion site
To achieve aperture fixation at the patellar side, the free graft ends have to be fixated directly to the patella. Therefore, the medial patellar margin is prepared and two guide wires are drilled tangentially into the patella at the proximal and distal ends of the medial edge. The guide wires are subsequently overdrilled with a cannulated 4 mm drill to a depth of 20 mm.
Graft fixation
The two free sutured graft ends are fixed into the patellar holes one after each other, using a 4.75 × 15 mm Swivel Lock (Fa. Arthrex), achieving a direct anatomical graft fixation. To accomplish this, the graft sutures are pulled through the PEEK eyelet of the Swivel Lock, and pushed into the drill holes. Keeping the suture under tension, the graft ends are fixed with the 4.75 × 15 mm Swivel Lock screw (Fig. 2). In this way, a double-bundle aperture fixation at the patellar side is achieved, leaving the graft loop free (Fig. 3).
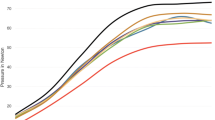
The suture loop is then used to pull the graft in between layers 2 and 3 to the femoral insertion. Next, a nitinol wire is inserted into the femoral drill hole and the suture loop of the graft is pulled laterally using the guide wire. Finally, while maintaining equal tension on both bundles, the graft is pulled into the femoral socket. Since biomechanical studies have shown that the MPFL has its maximal length and restraint against patella lateralisation in 30° of flexion (Fig. 4) [1], femoral fixation is performed in 30° of flexion with the lateral patellar edge positioned in line with the lateral trochlear border using a bioresorbable interference screw. An anatomical femoral insertion avoids an overcorrection, since an overtension of the graft can only occur if the femoral tunnel is placed too far anterior or proximal. In this case, the insertion point would move towards posterior in flexion, leading to a lengthening of the distance between patellar and femoral insertion, increasing the load onto the graft, and consequently, onto the patellofemoral joint.
If adequate medial restraint has been restored, lateral patellar dislocation should no longer be possible and routine skin closure is performed after reattaching the aponeurosis of the VMO back to the medial edge of the patella with resorbable sutures.
Postoperative treatment
Compared to other techniques, this aperture fixation with a biotenodesis screw at the patellar insertion provides an immediate stable tendon-to-bone fixation with an ultimate load to failure force at the patellar side higher than the 208-N needed to rupture an intact MPFL [1]. Weight bearing is allowed, however, no more than 20 kg until wound healing, while leg raising and quadriceps setting exercises can be started immediately with a free range of motion as tolerated.
Low impact activities such as running or cycling are allowed at 6 weeks post-op; full activity is permitted at 3 months.
Discussion
The most important finding and improvement in using the above-described technique was the possibility of an immediate full range of motion due to the aperture fixation at both sides. The benefit of anatomic graft positioning in ligament reconstruction has been known for a long time and has been clearly demonstrated in ACL reconstruction. Anatomical reconstruction of the MPFL is particularly important as biomechanical studies have demonstrated that the length change pattern of a MPFL reconstruction depends critically on the site of the femoral attachment; moreover, kinematics change significantly when the patellar or the femoral insertion has been off by only 5 mm [14]. Aside from tunnel placement, graft fixation is the other determining factor in ligament reconstruction [2]. Non-aperture fixation at either the femoral or patellar insertion can increase the risk of a delayed or insufficient tendon-to-bone healing, which may result in early loosening or slackening of the graft. To avoid this, a restricted range of motion is recommended by some surgeons; however, this may lead to arthrofibrosis, potentially necessitating an additional arthroscopic arthrolysis, carrying the additional risk of damage to the graft.
However, until today, only one technique describes a double-bundle aperture fixation at both sides where the graft is looped through a bone tunnel in the patella [3]. In this technique, the graft is shuttled through the patella and fixated press fit without any fixation devices, providing high initial fixation strength.
The aim of this manuscript was, therefore, to describe a procedure for an anatomical double-bundle reconstruction of the MPFL, respecting not only the ligament shape and both the anatomical patellar and femoral insertion areas, but also an aperture fixation.
In recent studies, a tendon transfer is described either to the patella or to the femur for reconstructing the MPFL [10, 13]. However, using these techniques, not only is the transferred muscle weakened in its original motion, but also that neither the patella nor the femoral insertion can be reconstructed at its anatomical insertion, and the graft used is always a single-bundle graft despite the fact that the MPFL consists of a proximal and a distal bundle [1]. This also includes a single-point fixation at the patellar side, increasing the rotational moment of the patella in flexion–extension movement. In terms of the fixation itself, some techniques fix the graft to the surrounding soft tissue [7] and not to the patellar and/or femoral bone even though a ligament is a structure in between bones, and recent studies have proven the high resistance to failure of tendon–bone interfaces.
Since tendon-to-bone healing showed excellent results in ACL reconstruction with hamstring tendon grafts, the same tendon-to-bone fixation is used at both, the femoral and the patellar sides in our technique.
While tendon-to-bone tunnel healing is created on the femoral side using a biodegradable screw for fixing the graft loop, the free graft ends are now fixed directly and anatomically into the patella using a biotenodesis device. This technique seems to provide a higher load to failure strength than an earlier-described technique, where a laminar attachment of the graft was performed at the patellar side using two suture anchors [11], which may result in loosening of the knot during full range of motion testing, or the patellar bone may be too soft for a secure anchoring. Tying of the free graft ends to each other at the patellar edge [15] is comparable to a non-aperture indirect fixation in ACL surgery. With the suture anchor technique, a secure graft to bone healing cannot be provided in every case and loosening of the graft could occur.
Another technique, looping the graft through the patella provides a very high initial fixation strength and preliminary results are promising [3]. However, if micromotion in the patellar tunnels develops, it may lead to a slackening of the graft at later follow up. However, if the graft is very short, the femoral insertion cannot be reached and an overly anterior fixation has to be accepted, leading eventually to an increased patellofemoral pressure or loss of flexion.
The use of a free autograft in the above-described technique allows us to place the graft at the anatomical insertion with a sufficient length and to recreate the double-bundle structure of the MPFL as it was described in an anatomical study by Amis et al. [1]. This provides a higher stability, as the proximal bundle seems to stabilise in extension, while the distal bundle stabilises in flexion. Furthermore, the double-bundle reconstruction decreases patellar rotation in contrast to techniques where only a single-point fixation is performed, or the middle part of the quadriceps tendon is flipped medially [14]. Reproducing the anatomy of the native MPFL enables the reconstructed ligament to have an isometric function, and, therefore, avoid increased patellofemoral pressure in higher degrees of knee flexion [11]. We also estimate that in long-term follow-up, slackening of the graft will not occur due to an improved tendon-to-bone healing by using direct fixation at the femoral as well as at the patellar insertion.
References
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee 10:215–220
Brand J Jr, Weiler A, Caborn DN, Brown CH Jr, Johnson DL (2000) Graft fixation in cruciate ligament reconstruction. Am J Sports Med 28:761–774
Christiansen SE, Jacobsen BW, Lund B, Lind M (2008) Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy 24:82–87
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26:59–65
Elias JJ, Cech JA, Weinstein DM, Cosgrea AJ (2004) Reducing the lateral force acting on the patella does not consistently decrease patellofemoral pressures. Am J Sports Med 32:1202–1208
Elias JJ, Wilson DR, Adamson R, Cosgarea AJ (2004) Evaluation of a computational model used to predict the patellofemoral contact pressure distribution. J Biomech 37:295–302
Ellera Gomes JL, Stigler Marczyk LR, Cesar de Cesar P, Jungblut CF (2004) Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: a follow-up study. Arthroscopy 20:147–151
Nomura E, Inoue M (2003) Surgical technique and rationale for medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Arthroscopy 19:E47
Nomura E, Inoue M, Osada N (2005) Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc 13:510–515
Ostermeier S, Stukenborg-Colsman C, Wirth CJ, Bohnsack M (2007) Reconstruction of the medial patellofemoral ligament by tunnel transfer of the semitendinosus tendon. Oper Orthop Traumatol 19:489–501
Schottle PB, Romero J, Schmeling A, Weiler A (2008) Technical note: anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg 128:479–484
Schottle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35:801–804
Steensen RN, Dopirak RM, Maurus PB (2005) A simple technique for reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft. Arthroscopy 21:365–370
Steensen RN, Dopirak RM, McDonald WG 3rd (2004) The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med 32:1509–1513
Thaunat M, Erasmus PJ (2007) The favourable anisometry: an original concept for medial patellofemoral ligament reconstruction. Knee 14:424–428
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schöttle, P.B., Hensler, D. & Imhoff, A.B. Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc 18, 147–151 (2010). https://doi.org/10.1007/s00167-009-0868-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0868-z