Abstract
Purpose
To evaluate the clinical outcome of the combined reconstruction of the medial patellofemoral ligament (MPFL) and medial patellotibial ligament (MPTL) for patellar instability with patella alta.
Methods
A total of 108 patients underwent a combined reconstruction of the MPFL and MPTL, and 58 patients were included in this study. The clinical results were evaluated and compared using the International Knee Documentation Committee (IKDC) scores, Kujala scores, and visual analogue scale (VAS) scores. The tibial tuberosity–trochlear groove (TT–TG) distance, three indices of patellar height (Insall–Salvati ratio, modified Insall–Salvati ratio, and Caton–Deschamps index), and patellar shift and tilt were defined preoperatively and at the 12- and 24-month follow-up visits.
Results
At the 12- and 24-month follow-up visits, 86.2% (50/58) and 87.9% (51/58) of the subjective outcomes were excellent, 5/58 (8.6%) and 4/58 (6.9%) were good, 1/58 (1.7%) and 2/58 (3.4%) were fair, and 2/58 (3.4%) and 1/58 (1.7%) were poor. There were significant improvements in the IKDC scores, from 51.9 ± 13.8 preoperatively to 80 ± 19.2 (P < 0.05) at 12 months and 85 ± 13.9 (P < 0.05) at 24 months; Kujala scores, from 55.1 ± 15.2 preoperatively to 82.6 ± 14.9 (P < 0.05) at 12 months and 89.5 ± 10.2 (P < 0.05) at 24 months; and VAS scores, from 58 ± 11 preoperatively to 12 ± 5 (P < 0.05) at 12 months and 11 ± 4 (P < 0.05) at 24 months. The patellar tilt, patellar shift, Insall–Salvati ratio, modified Insall–Salvati ratio, Caton–Deschamps index, and TT–TG distance all decreased significantly compared with the preoperative values, and there were no significant differences between the values at the 12- and 24-month follow-ups.
Conclusion
The results of this study show that a combined reconstruction of the MPFL and MPTL is an effective treatment for patellar instability with patella alta. This article emphasizes the combined effect of MPFL and MPTL instead of MPFL alone and provides an effective option for the treatment of recurrent patellar dislocation with patella alta.
Level of evidence
Case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellar instability is a common knee disorder encountered in children and adolescents. The predisposing factors for patellar dislocation are multifactorial, and include patellar shape, patella alta, patellar tilt, trochlear dysplasia, and an excessive tibial tuberosity–trochlear groove (TT–TG) distance [37, 41, 43]. The medial ligaments responsible for maintaining the stability of the patellofemoral joint are the medial patellofemoral ligament (MPFL), medial patellotibial ligament (MPTL), and the medial patellomeniscal ligament (MPML). An MRI study revealed that injury to the MPFL occurred in 98.6% of patients with an acute patellar dislocation [4]. Reconstruction of the MPFL has become one of the major interventions in the past years for the treatment of patellofemoral instability [23]. However, the observed complication rate is high, and clinical failure, which is presented by the persistence of objective or subjective instability, occurs in 12% of cases [38]. In addition, it is difficult to resolve the problems associated with patella alta using an isolated MPFL reconstruction [1]. Biomechanical research has demonstrated that the MPFL accounts for 50–60% of the medial soft-tissue restraining force against lateral patellar subluxation or dislocation in the first 30° of flexion, whereas the MPTL is an important secondary stabilizer [11, 14]. Philippot et al. found that the contribution of the MPTL and MPML as a unit to resist lateral translation increased from 26% in extension to 46% at 90° of flexion and was responsible for 72% of patellar tilt and 92% of patellar rotation at 90° of flexion [33]. In a clinical study, Garth et al. observed the presence of clinical and arthroscopic subluxation in patients with isolated MPML lesions with the knee in extension [21]. Thus, the MPTL and MPML are important in maintaining normal kinematics of the patellofemoral joint in all ranges of motion, especially in extension and in higher degrees of flexion. In addition, many clinical studies have reported good results following an isolated reconstruction of the MPTL [3, 34, 45]. The recurrence of instability may be caused by progressive loosening due to increased stress on the reconstructed MPFL. The reconstruction of one of the secondary stabilizing ligaments could decrease the stress on the MPFL and thus improve functional outcomes [25]. Patella alta draws the patella out of the osseous confines of the trochlear groove, requiring increased knee flexion angles to engage the trochlea and decreasing its inherent stability, thereby placing more emphasis on the MPFL to act as a checkrein and hold the patella in a reduced position [18].
While it has been widely published that patella alta is commonly associated with patellar instability, it remains unclear whether MPFL and MPTL reconstruction corrects patella alta. In the present study, we present a technique that combines the reconstruction of the MPFL and MPTL to treat patients with patellar instability and patella alta, and evaluate the patients’ clinical outcomes. It was hypothesized that the combined reconstruction of the MPFL and MPTL can provide a better clinical outcome in respect to improvement in IKDC and Kujala scores for patients with patella alta. The purpose of this study was to evaluate the short-term clinical and radiographic outcomes of combined reconstruction of the MPFL and MPTL in a population with patella alta.
Materials and methods
The study was approved by the ethics committee and all participants provided informed consent. A prospective study was performed with all patients who underwent a combined MPFL and MPTL reconstruction by the senior author, without further treatment with lateral retinaculum release, trochleoplasty, or osteotomy. Patients who met the following criteria were included: (1) at least two lateral patellar dislocations; (2) failure of a nonoperative treatment programme; (3) evaluation of the TT–TG distance > 20 mm; (4) diagnosis of patella alta by Insall–Salvati ratio criteria > 1.2; and (5) 18 years at the time of surgery. Patients were excluded if they had any of the following: (1) concomitant cruciate ligament reconstruction; (2) multiligament knee injury; (3) obligatory patella dislocation in flexion; (4) previous patellofemoral realignment procedure; (5) history of ligamentous knee injury; (6) grade III or IV chondral injury to the knee; or (7) unstable contralateral knee joint (patellofemoral joint and tibiofemoral joint) or ligament injury evaluated by magnetic resonance imaging (MRI). Between September 2009 and July 2014, a total of 108 patients (108 knees) with patellar instability consented to undergo a combined MPFL and MPTL reconstruction rather than an alternative surgical stabilization.
Fifty patients were excluded according to the criteria: 28 patients had undergone a previous realignment surgery in the same knee, 18 patients had grade III or IV chondral injuries, 2 patients had other ligamentous injuries, and 10 patients had congenital dislocations. Finally, 58 patients met the inclusion and exclusion criteria and were included in the study.
Surgical technique
All procedures were performed by the senior author. An examination was performed under anaesthesia to test patellofemoral joint instability.
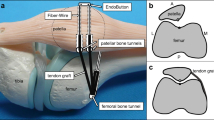
First, arthroscopy was routinely performed to complete a detailed assessment of the patellar instability and deal with other intra-articular injuries. The semitendinosus was harvested from a 3–4-cm oblique incision with an open-ended tendon stripper, while its distal attachment was kept intact. The harvested semitendinosus tendon was cleaned of soft tissue. The free end of the tendon was sutured using a finger-trap suture technique. A second incision was made on the medial border of the patella. The graft was then percutaneously transferred to the second incision on the medial edge of the patella. The graft was fixed to the tibial periosteum approximately 1.5 cm distal to the joint line with the knee at 80° of flexion prior to placing a 2.3-mm bioabsorbable anchor (Smith & Nephew, Endoscopy, Andover, MA) loaded with one strand of No. 2 FiberWire (Smith & Nephew), at a similar tension to the patellar ligament, so that it approximated the position of the MPTL. A third incision was made in the region between the adductor tubercle and the medial epicondyle. The semitendinosus tendon was passed through a tunnel between layers 2 and 3 of the medial retinaculum, reaching the area around the medial epicondyle. A 2.4-mm guide pin was placed in the medial aspect of the femur at the site of origin of the native MPFL. A tunnel was drilled over the guide pin to a depth of 30 mm and to a diameter equal to that of the graft between the medial epicondyle and the adductor tubercle. The graft was then passed through this tunnel. The graft was fixed to the midpoint between the adductor tubercle and the femoral insertion of the medial collateral ligament via a similar diameter interference screw at 30° of flexion and with slight medial pressure on the patella. The tenseness of the reconstructed MPFL and MPTL was then assessed with the knee in full extension and at 90° of flexion. The MPTL slackened in full extension (Fig. 1a), while the MPFL was in higher tension (Fig. 1b). When the knee was placed at 90° of flexion, the tension of the MPTL and MPFL were reversed (Fig. 1c, d).
Clinical outcome evaluation
Patients were evaluated preoperatively and at 6 weeks, 3 months, 12 months, and at a minimum of 24 months postoperatively. During the pre- and postoperative visits, one independent investigator performed the clinical outcome assessments and physical examinations. The investigator was not involved in the patients’ surgical treatment and was blinded to the clinical data. At each evaluation, patients were assessed for passive knee extension, active knee flexion, apprehension, return to work or school, and return to sports. Functional outcomes were assessed using IKDC scores [27], Kujala scores [28], Tegner scores [30], and VAS scores [42], and subjective outcomes were rated as excellent, good, fair, poor, or worse.
Radiological outcome evaluation
Patients underwent coronal and axial radiographs in addition to MRI preoperatively and postoperatively at the 12- and 24-month follow-up visits for the radiological outcome evaluation. The images were evaluated for the TT–TG distance and three indices of patellar height: the Insall–Salvati ratio [26], the modified Insall–Salvati ratio [22], and the Caton–Deschamps index [40]. The measurement of the patellar shift on axial imaging used in this study was suggested by Chia et al. [9]. Patellar tilt was measured according to the description by Beaconsfield et al. [6].
Ethical aspects
This study was ethically approved by the Chinese People’s Liberation Army General Hospital institutional review board (IRB) under the Reference Number (2011/0188).
Statistical analysis
Descriptive statistics for the location and scale of data distribution are presented as the mean ± standard deviation for normally distributed data and median [range (minimum–maximum)] for non-normal distributions. Data were analysed using repeated-measures analysis of variance (rANOVA) and a paired-sample t test as a post-hoc analysis in the case of normally distributed data. The Friedman test and the Wilcoxon signed-rank test were used for data analysis when the data were not normally distributed. A two-sided P value of < 0.05 indicated statistical significance. Data were analysed using the SPSS 19.0 software (SPSS, Inc., Chicago, Illinois). The planned sample size was based on the largest previous series of combined MPFL and MPTL reconstruction, which reported significant clinical improvements after ligament reconstruction [5, 25, 33].
Results
Of 108 potential patients, 58 patients (53.7%, 58 knees) were included in the study. All patients had a positive preoperative patellar apprehension test. The number of patellar dislocations ranged from two to seven. The mean age at surgery was 22.6 ± 4.9 years, and the mean follow-up period was 35.6 ± 10.8 months. The grade of trochlear dysplasia was classified using Dejour’s classification. Detailed and complete demographic data are shown in Table 1 [29]. No patients had a serious complication such as a wound infection, screw irritation, or graft failure.
Clinical outcome evaluation
At the 12-month follow-up, 1 out of the 58 patients had a positive apprehension test and subluxation episodes during running. However, these symptoms did not recur in this patient between the 12- and 24-month follow-up visits. Overall, at the 12- and 24-month follow-up visits, 50/58 (86.2%) and 51/58 (87.9%) of postoperative outcomes were excellent, 5/58 (8.6%) and 4/58 (6.9%) were good, 1/58 (1.7%) and 2/58 (3.4%) were fair, and 2/58 (3.4%) and 1/58 (1.7%) were poor, respectively. Patients returned to work or school at a mean of 1.0 ± 0.7 months. At 12 months after surgery, 8/58 (13.8%) patients had not returned to sports due to psychological fear, but all patients had returned to physical activity by the 24-month follow-up visit. The time at which patients returned to sport occurred at a mean of 3.9 ± 2.5 months.
There were no significant differences in range of motion preoperatively or postoperatively at any follow-up period (Table 2). In addition, there were no significant changes in the mean values for range of motion during the postoperative follow-up.
The post-hoc comparison of the preoperative, 12 month postoperative, and 24 month postoperative measurements showed a significant difference between the preoperative and postoperative values (12 months and 24 months) for all scores (Kujala, IKDC, and VAS scores), but there were no significant differences between the values 12 and 24 months after surgery (Table 2). All four measures significantly improved postoperatively compared with before surgery.
Radiological outcome evaluation
At 4 month postoperative, MRI revealed a relatively lower signal intensity, similar to the anterior cruciate ligament, which indicated a satisfactory maturity of the graft (Fig. 2). The radiological outcome evaluation of the ipsilateral knee comparing preoperative and follow-up results is shown in Table 3. Similar to the clinical outcome evaluation, the radiological assessments revealed a significant difference between the preoperative and postoperative values (at 12 and 24 months) for patellar tilt, patellar height, and TT–TG distance, but no significant difference was found between these values at 12 versus 24 months after surgery.
Discussion
The most important finding of this study is that the combined reconstruction of the MPFL and MPTL improves the clinical results and provides good control of patellar dislocation for patients with patella alta.
This article aimed to present an alternative technique and its preliminary results. The technique described in this study had satisfactory results, demonstrating the possibility of combined MPFL and MPTL reconstruction for patella alta in patients with recurrent dislocations (Video 1). With the combined reconstruction, stabilization of the patella was possible without other associated procedures, such as a tibial tuberosity transfer (TTT).
Patellar dislocation is known to be multifactorial, with malalignment, patellofemoral dysplasia, patella alta, soft-tissue imbalance, and ligamentous laxity contributing to the variability in individual cases. More than 100 operative procedures for patellar dislocation have been developed over the past century, and various techniques have been proposed for the treatment of patellar instability with good but not completely satisfactory results. Operations to address these factors can be grouped into proximal soft-tissue balancing, distal bony procedures, and trochleoplasty. Decision-making is multifactorial, and clear guidelines for optimal treatment have not yet been determined. MPFL reconstruction has been popular in the past decade, as patients undergoing the procedure have had improved functional results and low redislocation rates [7, 8]. However, this treatment is not always used for recurrent dislocations in patients with patella alta.
The importance of the MPFL in controlling lateral patellar dislocation has been well documented in different biomechanical studies. The MPTL also plays an important role, less as a secondary medial patellar stabilizer than as helping the patellar tendon to limit the upward displacement of the patella during a strong quadriceps contraction [2]. Though the MPTL provides less stabilizing force, its absence can result in increased lateral patellar translation and even lateral subluxation. Integrity of both the MPFL and MPTL restored a higher degree of stability to the patellofemoral joint when compared with reconstruction of either the MPFL or MPTL in isolation [24, 25]. Therefore, the concept of reconstructing both ligaments was pursued.
The present technique was based on the reinforced reconstruction of two major contributors of patellar stability in the sagittal and coronal views after analysing the contribution of various knee structures in preventing lateral patellar displacement. The present technique did not lead to any additional complications, as the insertion of the semitendinosus tendon at the pes anserinus was abandoned. Since the semitendinosus receives the majority of its blood supply from vessels in the perimysium, the periosteal insertion, and surrounding tissue via vessels in the paratenon, the hamstring autograft received a sufficient blood supply from the central origin and retained its viability at all time periods with no signs of avascular–acellular necrosis [32, 44]. The graft’s mechanical properties are supplied by the revascularization, and its viability is crucial for the combined reconstruction surgery on account of a faster ligamentization. One study showed that preserving the insertions reduced damage to the local biology and promoted early and superior healing of the graft [35], which allowed rapid incorporation into the bone tunnels, minimized the risk of graft elongation, and preserved the mechanoreceptors in the graft tissue [35]. It may be argued that this technique of reconstruction may not be anatomical for the attachment of the MPTL. Non-anatomical reconstruction might alter patellar tracking or produce increased tension at certain areas on the patellar articular surface [20]. No clinical or radiological evidence of patellar maltracking was observed in the present study, but a longer follow-up period is required.
Isolated MPFL reconstruction is generally accepted for TT–TG distances < 20 mm, while a TTT procedure is recommended when this distance is > 20 mm [13]. A recent study by Stephen et al. [39] questioned this distance and found that patellar tracking and contact pressures can be restored to normal with isolated MPFL reconstruction up to a TT–TG distance of 15 mm, whereas those patients with TT–TG distances > 15 mm may benefit from an additional tibial tuberosity (TT) medialization procedure. Although medialization of the TT leads to a normalization of the Q-angle and the TT–TG distance, it does not influence instability near full extension, which is often the cause of failure [19]. Furthermore, a TTT procedure also increases medial patellofemoral pressure and can lead to medial patellofemoral arthrosis [15, 17]. In patients with a TT–TG distance of more than 15 mm, a distal realignment procedure is unnecessary when proximal realignment is performed [12, 36]. All patients enrolled in the study presented with TT–TG distances > 20 mm, showing that the combined technique was suitable for patellar stabilization. No functional limitations were observed. We speculated that the MPFL combined with the MPTL to control patellar height and the medial attachment of the semitendinosus tendon to the tibia gives the patellar tendon a theoretical medialization-like effect for patella alta.
The postoperative evaluation of the radiographs showed a normalization of patellar height and a significant reduction in patellar shift and patellar tilt. The improvement of patellar height was achieved by the anatomical reconstruction of the MPFL, which is an oblique structure that creates a passive restraint against the lateralization and proximalization vector of the quadriceps [31]. The patellotibial ligament was not reconstructed and may have acted as an additional tibial rein and pulled the patella distally. A favourable effect on patellar tracking was also observed, since the patellar tilt and height were significantly improved.
The current study confirmed that combined MPFL and MPTL reconstruction was associated with improved patellar height in the setting of patellar instability, indicating that these ligaments may work for medial patellar stabilization by directing the patella medially and distally into the trochlear groove [18]. The choice of fixing the MPFL in mild flexion was to medially guide the patella into the trochlear groove at the initial knee fixation. The principal role of the MPFL was to ensure that the patella tracked within the trochlear groove at 0–30° of knee flexion, while beyond 30° of flexion, the lateral wall of the trochlear groove blocked the patella from dislocation. Meanwhile, the MPTL, similar in function to the patellar tendon, could gradually pull the patella down and medially as the flexion increased; thus, the downward and inward force worked together to stabilize the patella during the whole flexion. While the actual patellar tendon length does not change after MPFL reconstruction, the measurement of patella alta does improve [18]. The MPFL acts as a checkrein and creates a more medial resting position of the patella; this new medialized resting state in and of itself may also lower the patella on the lateral radiograph despite a constant patellar tendon length [18]. The topic of patella alta as an independent risk factor or result of patellofemoral instability remains unclear, though many authors have previously reported that patients with patellofemoral instability have greater rates of patella alta [10], which may be due, in part, to the MPFL rupture itself. It is known that the MPFL is an obliquely oriented structure with an origin on the patella more proximal to the distal insertion on the femur [31]. Therefore, disruption of this important structure may itself contribute to patella alta as measured on injury radiographs, and has previously been reported as a “risk factor” despite the lack of longitudinal radiographic data.
The risks involved were similar to those described for any MPFL reconstruction: overtightening of the graft leading to pain, restricted range of motion, medial subluxation, and patella baja. Elias et al. [15] highlighted the importance of appropriate MPFL tensioning when performing reconstructive procedures. They reported that the use of a graft with a resting length 3 mm shorter than an intact MPFL resulted in significantly increased compressive forces along the medial patellar facet at 30° and 40° of flexion [16]. MPFL over-tensioning should be avoided, as it could cause low medial patellar subluxation and increased pressure in the medial patellofemoral joint. The MPTL was adequately tensioned with fixation at 80° of knee flexion, and similar tension was achieved in the patellar ligament [24], because the tension of the MPTL was able to keep the patella in the intercondylar region at the beginning of 80° of knee flexion. The graft was tensioned only to maintain the patellar position and prevent excessive lateral translation. With adequate tension and positioning, the reconstructed MPFL should be looser in extension than in flexion. Insufficient graft tension may lead to recurrent instability, whereas overly aggressive tensioning may overload the medial patellofemoral joint, resulting in a poor functional outcome. To avoid this problem, appropriate patellar tracking was verified by flexing and extending the knee to confirm graft placement. These methods are advantageous in that it is possible to evaluate graft tensioning at different degrees of flexion, thus preserving the function of each ligament.
There were inherent limitations to this study. First, the generalizability of these results may be limited, as they represent the outcomes of one technique performed by a single surgeon. Second, without pre-injury radiographs, it is impossible to know whether patella alta was present prior to the initial injury (and represented a risk factor for initial patellofemoral dislocation), or if it was a result of the MPFL disruption itself and was noted on injury radiographs. A third limitation was that the study lacked a control group for comparison and a midterm follow-up period. A future randomized and long-term follow-up study to compare reconstruction of the MPFL versus reconstruction of both the MPFL and MPTL would be desirable. The clinical relevance of this technique is that it allows forces from two nearly vertical directions to control the track of the patella, and has the potential to reach a better functional outcome than MPFL reconstruction alone in the case of recurrent patellar dislocation with patella alta.
Conclusion
The results of this study show that a combined reconstruction of the MPFL and MPTL is an effective treatment for patellar instability with patella alta. However, a future randomized study with a long-term follow-up period is needed to compare the reconstruction of the MPFL with the combined reconstruction of the MPFL and MPTL.
References
Allen MM, Krych AJ, Johnson NR, Mohan R, Stuart MJ, Dahm DL (2018) Combined tibial tubercle osteotomy and medial patellofemoral ligament reconstruction for recurrent lateral patellar instability in patients with multiple anatomic risk factors. Arthroscopy. https://doi.org/10.1016/j.arthro.2018.02.049
Amis AA (2007) Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc 15:48–56
Aulisa AG, Falciglia F, Giordano M, Savignoni P, Guzzanti V (2012) Galeazzi’s modified technique for recurrent patella dislocation in skeletally immature patients. J Orthop Sci 17:148–155
Balcarek P, Ammon J, Frosch S, Walde TA, Schuttrumpf JP, Ferlemann KG et al (2010) Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity–trochlear groove distance. Arthroscopy 26:926–935
Baumann C, Pratte E, Sherman S, Arendt E, Hinckel B (2018) Reconstruction of the medial patellotibial ligament results in favorable clinical outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc 26:2920–2933
Beaconsfield T, Pintore E, Maffulli N, Petri GJ (1994) Radiological measurements in patellofemoral disorders. A review. Clin Orthop Relat Res 18–28
Bitar AC, Demange MK, D’Elia CO, Camanho GL (2012) Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med 40:114–122
Buckens CF, Saris DB (2010) Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability: a systematic review. Am J Sports Med 38:181–188
Chia SL, Merican AM, Devadasan B, Strachan RK, Amis AA (2009) Radiographic features predictive of patellar maltracking during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 17:1217–1224
Colvin AC, West RV (2008) Patellar instability. J Bone Joint Surg Am 90:2751–2762
Conlan T, Garth WP Jr, Lemons JE (1993) Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 75:682–693
Crosby EB, Insall J (1976) Recurrent dislocation of the patella. Relation of treatment to osteoarthritis. J Bone Joint Surg Am 58:9–13
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26:59–65
Elias JJ, Cech JA, Weinstein DM, Cosgrea AJ (2004) Reducing the lateral force acting on the patella does not consistently decrease patellofemoral pressures. Am J Sports Med 32:1202–1208
Elias JJ, Cosgarea AJ (2006) Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med 34:1478–1485
Elias JJ, Wilson DR, Adamson R, Cosgarea AJ (2004) Evaluation of a computational model used to predict the patellofemoral contact pressure distribution. J Biomech 37:295–302
Fabricant PD, Ladenhauf HN, Salvati EA, Green DW (2014) Medial patellofemoral ligament (MPFL) reconstruction improves radiographic measures of patella alta in children. Knee 21:1180–1184
Farahmand F, Naghi Tahmasbi M, Amis A (2004) The contribution of the medial retinaculum and quadriceps muscles to patellar lateral stability—an in-vitro study. Knee 11:89–94
Feller JA, Amis AA, Andrish JT, Arendt EA, Erasmus PJ, Powers CM (2007) Surgical biomechanics of the patellofemoral joint. Arthroscopy 23:542–553
Garth WP Jr, Connor GS, Futch L, Belarmino H (2011) Patellar subluxation at terminal knee extension: isolated deficiency of the medial patellomeniscal ligament. J Bone Joint Surg Am 93:954–962
Grelsamer RP, Meadows S (1992) The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Relat Res 280:170–176
Hensler D, Sillanpaa PJ, Schoettle PB (2014) Medial patellofemoral ligament: anatomy, injury and treatment in the adolescent knee. Curr Opin Pediatr 26:70–78
Hinckel BB, Gobbi RG, Bonadio MB, Demange MK, Pecora JR, Camanho GL (2016) Reconstruction of medial patellofemoral ligament using quadriceps tendon combined with reconstruction of medial patellotibial ligament using patellar tendon: initial experience. Rev Bras Ortop 51:75–82
Hinckel BB, Gobbi RG, Demange MK, Bonadio MB, Pecora JR, Camanho GL (2016) Combined reconstruction of the medial patellofemoral ligament with quadricipital tendon and the medial patellotibial ligament with patellar tendon. Arthrosc Tech 5:e79–e84
Insall J, Salvati E (1971) Patella position in the normal knee joint. Radiology 101:101–104
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P et al (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29:600–613
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9:159–163
Lippacher S, Dejour D, Elsharkawi M, Dornacher D, Ring C, Dreyhaupt J et al (2012) Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med 40:837–843
Mani S, Kirkpatrick MS, Saranathan A, Smith LG, Cosgarea AJ, Elias JJ (2011) Tibial tuberosity osteotomy for patellofemoral realignment alters tibiofemoral kinematics. Am J Sports Med 39:1024–1031
Nomura E, Inoue M, Osada N (2005) Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthrosc 13:510–515
Papachristou G, Nikolaou V, Efstathopoulos N, Sourlas J, Lazarettos J, Frangia K et al (2007) ACL reconstruction with semitendinosus tendon autograft without detachment of its tibial insertion: a histologic study in a rabbit model. Knee Surg Sports Traumatol Arthrosc 15:1175–1180
Philippot R, Boyer B, Testa R, Farizon F, Moyen B (2012) The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc 20:331–336
Rillmann P, Dutly A, Kieser C, Berbig R (1998) Modified Elmslie-Trillat procedure for instability of the patella. Knee Surg Sports Traumatol Arthrosc 6:31–35
Rodeo SA, Arnoczky SP, Torzilli PA, Hidaka C, Warren RF (1993) Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg Am 75:1795–1803
Scuderi G, Cuomo F, Scott WN (1988) Lateral release and proximal realignment for patellar subluxation and dislocation. A long-term follow-up. J Bone Joint Surg Am 70:856–861
Servien E, Verdonk PC, Neyret P (2007) Tibial tuberosity transfer for episodic patellar dislocation. Sports Med Arthrosc 15:61–67
Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C (2012) A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 40:1916–1923
Stephen JM, Dodds AL, Lumpaopong P, Kader D, Williams A, Amis AA (2015) The ability of medial patellofemoral ligament reconstruction to correct patellar kinematics and contact mechanics in the presence of a lateralized tibial tubercle. Am J Sports Med 43:2198–2207
Thevenin-Lemoine C, Ferrand M, Courvoisier A, Damsin JP, Ducou le Pointe H, Vialle R (2011) Is the Caton-Deschamps index a valuable ratio to investigate patellar height in children? J Bone Joint Surg Am 93:e35
Ward SR, Terk MR, Powers CM (2007) Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am 89:1749–1755
Watanabe T, Muneta T, Ikeda H, Tateishi T, Sekiya I (2008) Visual analog scale assessment after medial patellofemoral ligament reconstruction: with or without tibial tubercle transfer. J Orthop Sci 13:32–38
Weber AE, Nathani A, Dines JS, Allen AA, Shubin-Stein BE, Arendt EA et al (2016) An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am 98:417–427
Zaffagnini S, Golano P, Farinas O, Depasquale V, Strocchi R, Cortecchia S et al (2003) Vascularity and neuroreceptors of the pes anserinus: anatomic study. Clin Anat 16:19–24
Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Luetzow WF, Vaccari V, Benzi A et al (2014) Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc 22:2491–2498
Funding
The study was supported by Beijing Nova Program (Z161100004916137).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Ethical approval
This study was ethically approved by the Chinese People's Liberation Army General Hospital institutional review board.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MP4 199913 KB)
Rights and permissions
About this article
Cite this article
Yang, Y., Zhang, Q. Reconstruction of the medial patellofemoral ligament and reinforcement of the medial patellotibial ligament is an effective treatment for patellofemoral instability with patella alta. Knee Surg Sports Traumatol Arthrosc 27, 2599–2607 (2019). https://doi.org/10.1007/s00167-018-5281-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5281-z