Abstract
Purpose
This study was conducted to examine the long-term survivorship and functional outcome of distal femoral varus osteotomy with fresh osteochondral allograft following failed lateral tibial plateau fracture surgery. We hypothesized that this procedure would be associated with a low rate of conversion to total knee arthroplasty (TKA) at medium to long-term follow-up.
Methods
A consecutive series of 27 of distal femoral varus osteotomy combined with fresh osteochondral allograft following (27 patients) conducted between January 1981 and January 2005 for failed lateral tibial plateau fracture was retrospectively reviewed. Outcome measures included the Knee Society Knee Score (KSKS) and Knee Society Function Score (KSFS) and conversion rates to TKA.
Results
The study group consisted of 15 females (55.6 %) and 12 males (44.4 %), with a median age of 41.2 years (range 17–62 years). The median follow-up was 13.3 years (range 2–31 years). The knee function scores improved significantly at 2 years post-surgery (p < 0.01) from a median of 54.6 points preoperatively to 83.8 points (KSKS) and median of 50.6 points to 71.1 points (KSFS) at 2 years post-distal femoral varus osteotomy with fresh osteochondral allograft following surgery. At most recent follow-up, 4/27 patients had required conversion to TKA, and one patient had fractured the FOCA, requiring revision of the allograft. The survivorship for distal femoral varus osteotomy with fresh osteochondral allograft following was 88.9 ± 4.6 % at 10 years, 71.4 ± 18.1 % at 15 years, and 23.8 ± 11.1 % at 20 years.
Conclusion
The use of distal femoral varus osteotomy combined with fresh osteochondral allograft following in patients with failed lateral tibial plateau fracture results in the majority of patients having good or excellent clinical outcomes and significantly delays the need for TKA in most patients.
Level of evidence
Case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Purpose
Realignment osteotomies around the knee are a well-established treatment for symptomatic primary knee osteoarthritis (OA) in younger patients and have been shown to relieve pain and redistribute the weight-bearing axis by off-loading the affected compartment [5, 7, 12, 13, 19, 22]. While the results of proximal tibial valgus osteotomy in appropriately selected patients with varus deformity and medial compartment arthritis are encouraging [9, 12], the results of a proximal tibial varus osteotomy for primary valgus deformity of the knee are less favourable, especially if the valgus deformity is greater than 12° or if the correction will result in a tibio-femoral tilt of more than 10° [16, 18]. In this setting, a distal femoral varus osteotomy is preferred, with the reported 10-year survivorship ranging from 83 to 87 % [2, 4, 21].
One of the more common causes of lateral compartment OA is a tibial plateau fracture, with the incidence of end-stage OA after lateral tibial plateau fractures reported to be between 23 and 44 % [6, 20]. These injuries are often seen in younger patients and are often associated with significant articular defects and residual valgus malalignment. In this setting, osteotomy alone cannot address the osteochondral defects and may be limited in its ability to correct the mechanical axis [14]. Furthermore, techniques such as periosteal grafting and autologous chondrocyte transplantation can provide surface coverage, but are unable to address associated bone defects [3].
In this setting, combining a varus osteotomy with a lateral tibial focal osteochondral allograft may be appealing, allowing the restoration of the osteochondral defect and the mechanical axis of the knee; the osteotomy also serves to protect the osteochondral allograft. This study was conducted to examine the long-term survivorship and functional outcome of distal femoral varus osteotomy with focal osteochondral allograft following failed lateral tibial plateau fracture surgery—currently there is no long-term data in the literature on this topic. The hypothesis was that this procedure would be associated with a low rate of conversion to total knee arthroplasty (TKA) at medium to long-term follow-up.
Materials and methods
A consecutive series of 27 distal femoral varus osteotomies combined with focal osteochondral allografts (27 patients) conducted between January 1981 and January 2005 at our institution was retrospectively reviewed. All 27 patients included in the study had previously undergone an open reduction with internal fixation surgery of a lateral tibial plateau fracture, yet continued to complain of lateral knee pain.
All information was obtained from medical records as well as a prospective database; data included patients’ age at time of surgery, gender, length of follow-up, and time to conversion to TKA (Table 1). Clinical and radiographic examination was conducted postoperatively at 6 weeks, 6 months, 1 year, and then biannually. Patients were assessed for pain, range of motion, limb alignment, and knee stability, allowing calculation of a Knee Society Function Score (KSFS) and a Knee Society Knee Score (KSKS) according to the Knee Society clinical rating system proposed by Insall et al. [8]. For patients who subsequently underwent TKA, the KSFS and KSKS prior to conversion were used as most recent scores for the purpose of statistical analysis. In addition, the KSFS and KSKS were graded as excellent (80–100), good (70–79), fair (60–69), and poor (<60) [1].
Radiographic evaluation included pre- and postoperative anterior–posterior and lateral views of the knee, and full-length standing anterior–posterior radiograph of the lower extremity taken preoperatively and 2 years after surgery (Figs. 1, 2). Kellgren and Lawrence [10] grading of OA was graded on weight-bearing radiographs at latest follow-up.
a Postoperative AP radiograph. A distal femoral varising osteotomy has been performed, using a blade plate. A fresh osteochondral allograft has also been used to reconstruct the lateral tibial plateau and secured with 3.5-mm screws. b Postoperative long leg radiograph, demonstrating restoration of alignment
Failure was defined as a repeated focal osteochondral allograft implantation or conversion to TKA.
Surgical technique
All distal femoral varus osteotomies combined with focal osteochondral allografts were performed by a single surgeon (AEG), with the patient supine and with the use of a tourniquet. A 15–20 cm midline incision is made starting lateral to the tibial tuberosity and positioned so that it can be used for TKA in the future. The hardware used for the fracture fixation is removed from the lateral tibial plateau, and an arthrotomy is performed via a lateral parapatellar approach taking care not to injure the underlying femoral cartilage.
The lateral tibial plateau is resected to a depth of between 1 and 2 cm depending on the traumatic defect using an oscillating saw, leaving the anterior soft tissue attachment of the native lateral meniscus intact in order to allow re-attachment of the lateral meniscus of the focal osteochondral allograft. The osteochondral allograft is cut in similar shape and size (1–2 cm thick) in order to replace the native lateral tibial plateau. The allograft is temporarily fixed to the tibial plateau with 2–3 k-wires, and the range of motion and stability of the knee examined with the allograft in place. If necessary, fine tuning of the allograft size in the medial–lateral dimension was performed until satisfactory stability and 0–140° of knee range of motion are achieved. The allograft is then secured to the native proximal tibia via two or three 3.5-mm cancellous screws. The lateral meniscus of allograft is then sutured in place with an absorbable suture to the posterior root at the lateral edge of the PCL, to the popliteus tendon, and at the anterior soft tissue attachment of the native lateral meniscus. After completing the focal osteochondral allograft implantation, a distal femoral closing wedge varus osteotomy was performed via a subvastus approach, as previously described by the authors [11].
The study was approved by the institutional review board (IRB number 10-0020-C) at the Mount Sinai Hospital, Toronto, Ontario, Canada.
Statistical analysis
Statistical analysis was performed with the use of the Statistical Package for Social Science (SPSS) software (version 20; SPSS, Chicago, Illinois). One-way ANOVA test was performed to compare the preoperative and postoperative KSFS and KSKS at set time intervals (2, 5, 10 years, and most recent), in order examine the decline of knee function specifically in this subgroup. Kaplan–Meier survival analysis was performed with the end point defined as conversion or planned conversion to TKA. For all statistical tests, a p < 0.05 was chosen as the level of significance.
Results
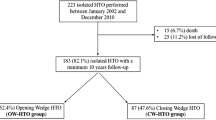
The study group consisted of 15 females (55.6 %) and 12 males (44.4 %), with a median age of 42 years (range 17–62 years) at the time of their varus osteotomy + focal osteochondral allograft. The median follow-up was 13 years (range 2–31 years) (Table 1). None of the patients in the study group were lost to follow-up.
The KSKS improved significantly (p < 0.01) from a median of 57 points preoperatively to 86 points at 2 years post-surgery (Fig. 3; Tables 2, 3). Similarly, the KSFS improved significantly (p < 0.01) from a median of 50 points to 70 points (Table 3). At 5-year follow-up, two patients (7.4 %) had required conversion to TKA at 2 years (for progressive arthritis changes) and 5 years (for allograft subsidence), respectively, leaving 25 patients available for evaluation. At 5-year follow-up, the median KSKS was 85 and the mean KSFS was 70 points, both significantly (p < 0.01) better than the preoperative scores.
Nineteen patients were available for a 10-year follow-up evaluation—in five patients <10 years passed since their surgery and one patient had required a revision focal osteochondral allograft procedure due to osteochondral graft fracture at 8 years post-surgery. Ten years postoperatively, the median KSKS declined to 75 points, which, while significantly better than the preoperative KSKS (p < 0.01), was significantly worse than both the 2- and 5-year KSKS (p = 0.04). At 10 years postoperatively, the median KSFS was 70 points which was not worse than the 2- and 5-year follow-up KSFS and remained significantly better than the preoperative KSFS (p < 0.01).
At most recent follow-up (median 13 years, range 2–31), two additional patients required conversion to TKA at 13 (for progressive arthritic changes) and 20 years (for subsidence) post-surgery, leaving 17 patients available for evaluation. The median KSKS of the remaining patients further declined to 70 points, which was not significantly worse than the 10-year follow-up KSKS, and remained significantly better than the preoperative KSKS (p < 0.01). The KSFS at latest follow-up further declined to a median of 65 points, which was not significantly worse than the previous postoperative KSFS, and remained significantly better than the preoperative SKFS (p < 0.01).
Union of the allograft was seen in all patients. Due to the long-term nature of this study, only 5/27 preoperative long leg radiographs were available secondary to the digitization of the X-ray system at our institution—the median preoperative tibio-femoral axis was 7° valgus (range 5–15° valgus) in these patients. Postoperative long leg views were available in 15/27 patients—the median postoperative tibio-femoral axis was 2° varus (range 5° varus to 5° valgus). Allograft subsidence of 5 and 10 mm, respectively, was seen in two patients, both of who required revision to TKA. At final follow-up in the 17 patients not converted to TKA, the Kellgren–Lawrence grading of OA on weight-bearing films was grade 0–2 in 12/17 patients, grade 3 in 4/17 patients, and grade 4 in one patient. Patients who developed advanced osteoarthritic changes in the knee had worse knee scores at final follow-up than those who did not.
The Kaplan–Meier survival analysis is seen in Fig. 4. The 10-year survivorship for distal femoral varus osteotomy + focal osteochondral allograft was 88.9 ± 4.6 %. At 15 years, the survivorship declined to 71.4 ± 18.1 %, respectively, and at 20 years, survivorship further declined to 23.8 ± 11.1 %.
Discussion
The major finding of this study is that the 10-year survival (using TKA as an end point) for distal femoral varus osteotomy combined with focal osteochondral allograft is excellent at 89 %; however, the survival declines significantly over time to 71.4 % at 15 years and 23.8 % at 20 years. This surgery is also associated with significantly improved Knee Society Scores; however, these also tend to deteriorate slowly over time.
The lateral tibial plateau is frequently involved in tibial plateau fractures. When combined with meniscal injury and valgus malalignment, 44 % of these fractures are expected to result in OA [6]. As many patients with lateral tibial plateau fractures are young and active at the time of their index trauma, efforts to delay TKA via restoration of their chondral stock should be encouraged. However, it is imperative that surgery is performed before the lateral femoral condyle is irreversibly affected.
There is limited information regarding the long-term outcome of distal femoral varus osteotomy in the literature. Edgerton et al. [4] reported on 23 patients (24 knees) with lateral compartment OA managed with varus osteotomy, finding that 71 % of patients had a good or excellent result at a mean follow-up of 8.3 years—at final follow-up, 13 % had been converted to TKA. Wang and Hsu reported a 10-year survivorship of 87 % in 30 patients, with satisfactory results seen in 83 % at a mean follow-up of 99 months [21]. Backstein et al. [2] reported on 40 patients who had undergone unilateral and bilateral distal femoral varus osteotomy, describing a survivorship of 82 and 45 % at 10 and 15 years, respectively. Each of these studies included patients with a variety of etiologies resulting in lateral compartment OA and valgus malalignment.
To the best knowledge of the authors, there has been no previous report of the outcomes of distal femoral varus osteotomy and tibial focal osteochondral allograft after failed tibial plateau fracture surgery. A previous report from our institution published in 2003 looked at the use of focal osteochondral allograft for the treatment for proximal tibial defects secondary to trauma, both medial and lateral [15]. At a mean of 12 years, 44/65 (68 %) patients had an intact graft—the remaining 1/3 of patients had been converted to a TKA. Review of the available radiographs of patients with intact grafts demonstrated union in all cases and graft collapse of >3 mm in 3/35 (8.6 %).
The results of this study indicate that the KSKS (reflecting pain, range of motion, and stability) of patients is expected to significantly improve after osteochondral allograft combined with osteotomy, from a median of 57 points to 86 points at 2 years after surgery, with 92.6 % of the patients having good or excellent scores. The improvement in the median KSFS (which reflects the patients’ ability to walk, climb stairs and need for walking aids) is more modest, increasing from 50 points to 70 points, with two-thirds of the patients having good or excellent outcomes. The results show that this improvement can be expected to last well over a decade, although patient outcomes will most likely partly diminish over time.
A percentage of patients undergoing varus osteotomy in combination with focal osteochondral allograft will eventually require conversion to a TKA—two patients required a TKA prior to 10 years, with an additional two patients converted at 13 and 20 years after the index procedure. For the majority of these patients, conversion from distal femoral varus osteotomy to TKA can be performed successfully with the use of standard knee implants, without the need for stemmed or highly constrained components. Our institution has previously reported on 22 consecutive distal femoral varus osteotomies that were converted to TKA with a mean follow-up of 5 years [11]. Of the 22 patients converted, only 5 patients (all of which had poor bone quality) required stemmed components. At follow-up of between 8 and 11 years, only 2 of the 22 patients required revision due to aseptic loosening.
An alternative treatment for this difficult cohort of patients might be to perform a varus osteotomy in isolation or to perform a focal osteochondral allograft in isolation. Without a control group, it is impossible to say for certain that combining a distal femoral varus osteotomy and a focal osteochondral allograft is the ideal procedure for these patients. However, the senior surgeon (AEG) believes that the osteochondral allograft is a crucial component of the surgery, which is used to address both the severe chondral defects and bony deficiency. Furthermore, previous research from this institution suggests that patients in whom a previous or concomitant realignment is performed in association with focal osteochondral allograft have improved outcomes [15]. This is in line with other research demonstrating the importance of a distal femoral varus osteotomy in unloading the lateral compartment of the knee [11, 17].
Other limitations of this study are related to the long-term follow-up involved—information regarding the original classification of the tibial plateau fractures was lacking, and pre- and postoperative long leg radiographs were also not available for all patients. It would also have been interesting to include BMI; however, information regarding patient height and weight was not routinely collected. Clinical outcomes were assessed using Knee Society Scores; however, this score was originally developed for TKA, rather than for patients undergoing corrective osteotomy. A patient-derived score such as the WOMAC may have been more appropriate [18].
Conclusion
The use of distal femoral varus osteotomy combined with focal osteochondral allograft in patients with failed lateral tibial plateau fracture results in the majority of patients having good or excellent clinical outcomes and significantly delays the need for TKA in most patients.
References
Asif S, Choon DS (2005) Midterm results of cemented Press Fit Condylar Sigma total knee arthroplasty system. J Orthop Surg (Hong Kong) 13:280–284
Backstein D, Morag G, Hanna S, Safir O, Gross A (2007) Long-term follow-up of distal femoral varus osteotomy of the knee. J Arthroplasty 22:2–6
Bartlett W, Skinner JA, Gooding CR, Carrington RW, Flanagan AM, Briggs TW, Bentley G (2005) Autologous chondrocyte implantation versus matrix-induced autologous chondrocyte implantation for osteochondral defects of the knee: a prospective, randomised study. J Bone Joint Surg Br 87:640–645
Edgerton BC, Mariani EM, Morrey BF (1993) Distal femoral varus osteotomy for painful genu valgum. A five-to-11-year follow-up study. Clin Orthop Relat Res 288:263–269
Gardiner A, Richmond JC (2013) Periarticular osteotomies for degenerative joint disease of the knee. Sports Med Arthrosc 21:38–46
Honkonen SE (1995) Degenerative arthritis after tibial plateau fractures. J Orthop Trauma 9:273–277
Hutchison CR, Cho B, Wong N, Agnidis Z, Gross AE (1999) Proximal valgus tibial osteotomy for osteoarthritis of the knee. Instr Course Lect 48:131–134
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Insall JN, Joseph DM, Msika C (1984) High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Joint Surg Am 66:1040–1048
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kosashvili Y, Safir O, Gross A, Morag G, Lakstein D, Backstein D (2010) Distal femoral varus osteotomy for lateral osteoarthritis of the knee: a minimum ten-year follow-up. Int Orthop 34:249–254
Laprade RF, Spiridonov SI, Nystrom LM, Jansson KS (2012) Prospective outcomes of young and middle-aged adults with medial compartment osteoarthritis treated with a proximal tibial opening wedge osteotomy. Arthroscopy 28:354–364
Marti RK, Verhagen RA, Kerkhoffs GM, Moojen TM (2001) Proximal tibial varus osteotomy. Indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am 83-A:164–170
Matthews LS, Goldstein SA, Malvitz TA, Katz BP, Kaufer H (1988) Proximal tibial osteotomy. Factors that influence the duration of satisfactory function. Clin Orthop Relat Res 229:193–200
Shasha N, Krywulak S, Backstein D, Pressman A, Gross AE (2003) Long-term follow-up of fresh tibial osteochondral allografts for failed tibial plateau fractures. J Bone Joint Surg Am 85-A(Suppl 2):33–39
Sprenger TR, Doerzbacher JF (2003) Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty-two years. J Bone Joint Surg Am 85-A:469–474
Sternheim A, Garbedian S, Backstein D (2011) Distal femoral varus osteotomy: unloading the lateral compartment: long-term follow-up of 45 medial closing wedge osteotomies. Orthopedics 34:e488–e490
Tjornstrand BA, Egund N, Hagstedt BV (1981) High tibial osteotomy: a seven-year clinical and radiographic follow-up. Clin Orthop Relat Res 160:124–136
Vainionpaa S, Laike E, Kirves P, Tiusanen P (1981) Tibial osteotomy for osteoarthritis of the knee. A five to ten-year follow-up study. J Bone Joint Surg Am 63:938–946
Volpin G, Dowd GS, Stein H, Bentley G (1990) Degenerative arthritis after intra-articular fractures of the knee. Long-term results. J Bone Joint Surg Br 72:634–638
Wang JW, Hsu CC (2006) Distal femoral varus osteotomy for osteoarthritis of the knee. Surgical technique. J Bone Joint Surg Am 88(Suppl 1 Pt 1):100–108
Zaffagnini S, Bonanzinga T, Grassi A, Marcheggiani Muccioli GM, Musiani C, Raggi F, Iacono F, Vaccari V, Marcacci M (2013) Combined ACL reconstruction and closing-wedge HTO for varus angulated ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc 21:934–941
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Drexler, M., Gross, A., Dwyer, T. et al. Distal femoral varus osteotomy combined with tibial plateau fresh osteochondral allograft for post-traumatic osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 23, 1317–1323 (2015). https://doi.org/10.1007/s00167-013-2828-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2828-x