Abstract
Distal femoral varus osteotomy (DFVO) may be indicated for symptomatic lateral compartment gonarthrosis associated with valgus deformity in younger, active patients. Thirty-three consecutive DFVOs (31 patients) with a minimum follow-up of ten years (mean 15.1, range 10–25) were reviewed. Fifteen DFVOs were converted to total knee arthroplasty (TKA) and one DFVO was awaiting TKA, reaching an overall failure rate of 48.5% at a mean of 15.6 years (range 6–21.5). Of the remaining 17 DFVOs, ten (58.8%) had good or excellent results, two (11.8%) had fair results and five (29.4%) had poor results. Mean modified Knee Society scores improved significantly (p < 0.01) from 36.8 preoperatively to 77.5 at one year post DFVO. DFVO is a viable treatment alternative for lateral compartment gonarthrosis. Conversion to TKA is expected to be required in approximately half of the patients at a mean of 15.6 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteotomies around the knee for the purpose of unloading the affected compartment and correction of the underlying deformity are a well recognised treatment alternative for symptomatic gonarthrosis in active patients [1–4]. Varus deformity with medial compartment arthritis is more common than valgus deformity with lateral compartment involvement [5]. Several studies reported good outcomes lasting more than a decade for patients with varus deformity treated by high valgus tibial osteotomy in appropriately selected patients [1–5].
However, in the situation of correction of valgus deformity, a proximal tibial varus osteotomy has resulted in less reliable improvement in symptoms and knee function [6, 7]. These suboptimal outcomes are possibly related to excessive translational forces on intraarticular structures (hyaline cartilage, menisci, capsule) due to the resulting excessive coronal tibial slope. Thus, correction may be conducted through the proximal tibia only if the deformity is minimal and the resulting superolateral slope of the joint line is expected to be smaller than 10° [8]. Instead, for a valgus deformity of more than 12° or in situations where the plane of the joint is deviated from the horizontal by more than 10°, a distal femoral varus osteotomy (DFVO) is preferred by the authors.
A recent study indicated good mid-term success rates of DFVO even in the presence of moderate patello femoral arthritis at a mean follow-up of 99 months [9]. It has been the practice in our institution for more than three decades to correct lateral compartment gonarthritis with valgus deformity using a DFVO [10, 11].
The purpose of the this study was to present our long-term outcomes of DFVO with a minimum follow-up of ten years in the management of lateral unicompartmental gonarthrosis.
Materials and methods
A consecutive series of 36 DFVO (34 patients) conducted between January 1984 and January 1999 at our institution was retrospectively reviewed. Institutional research ethics board approval was obtained prior to commencing this study. Data were obtained from hospital and office charts as well as from our prospective database that included patients’ age at surgery, gender, length of follow-up and time to conversion to total knee arthroplasty (TKA) (Table 1).
Follow-up consisted of clinical and radiographic examination at standard intervals (preoperative, postoperatively at six weeks, six months, at one year and then annually). Patients were assessed for pain, range of motion, limb alignment and knee stability. Subsequently, modified knee society scores (MKSS) were calculated for each patient according to the Insall modification from 1993 [12]. For patients who underwent subsequent TKA, the MKSS prior to conversion was used as most recent MKSS for the purpose of statistical analysis.
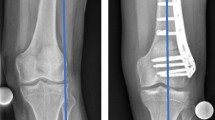
Radiographic evaluation included anterior–posterior and lateral views of the knee (Fig. 1). In addition, a full-length standing anterior–posterior radiograph of the lower extremity was taken preoperatively and one year after surgery to depict the postoperative limb alignment.
Three DFVOs (8.3%) were lost to follow-up after less than two years following the osteotomy, leaving 33 DFVOs (31 patients) available for assessment. The study group consisted of 25 females (75.6%) and eight males (24.4%), at a mean age of 45.5 years (range 24–63) at the time of their DFVO. The mean follow-up was 15.1 years (range 10–25, Table 1). Failure was defined as conversion to total knee arthroplasty (TKA) or if the patient was put on a list for TKA.
Statistical analysis
Statistical analysis was performed with the use of the Statistical Package for Social Science (SPSS) software (version 14; SPSS Inc., Chicago, Illinois). One way ANOVA tests were performed to compare the preoperative, one-year post surgery, ten-year post surgery and at most recent postoperative MKSS scores. ANOVA tests of the non-failed DFVOs were also performed to compare the preoperative and postoperative MKSS at the same time intervals in order to examine the decline of knee function specifically in this subgroup.
A t-test was performed to compare the preoperative MKSS as well as the patients' age at the time of surgery of the failed DFVOs to those of the non-failed DFVO.
For all statistical tests a p < 0.05 was chosen as the level of significance.
Surgical technique
The patient is placed in a supine position and a tourniquet is inflated prior to skin incision. A straight 15 cm midline incision is made starting just distal to the joint line and continuing proximally. This incision is positioned so that it can easily be used for TKA in the future [13].
The vastus medialis muscle is bluntly dissected from the medial intermuscular septum and reflected anteriorly and laterally to expose the medial aspect of the femoral cortex and the medial femoral condyle. A small arthrotomy is performed to enable visual control of the guidewires throughout the procedure. The knee is flexed to 90°, and a guide wire is passed from medial to lateral parallel to the articular surfaces through the medial arthrotomy and across the joint space. A second wire is then drilled into the medial femoral condyle parallel to the first wire and approximately 1 cm proximal to the femoral articular surface. An anteroposterior (AP) radiograph or image intensifier is used to confirm that the second wire is indeed parallel to the articular surface (Fig. 2). Placement of this wire parallel to the articular surface is important for a more predictable correction of the deformity by aligning the anatomical axis of the femur perpendicular to the femoral articular surface and the blade plate.
Once the parallel placement of the second guidewire has been confirmed, three 4.5-mm drill holes are made in the medial femoral cortex at a location 2–2.5 cm from the articular surface in the anterior half of the medial cortex (Fig. 2). These drill holes are for the entrance of the blade plate chisel and prevent uncontrolled fracture of the femur. The chisel is then inserted to a depth of 50–70 mm, depending on the size of the distal femur. The plate holder is used to guide the chisel and to obtain optimal apposition of the plate to long axis of the femur. After insertion of the chisel, AP and lateral images are obtained to confirm its alignment (Fig. 3). An arthrotomy is performed from the medial side, just proximal to the adductor tubercle and the anterior part of the femoral articular surface. Visualisation through this medial arthrotomy can confirm that the chisel has not penetrated the intercondylar notch by either direct vision or palpation of the anterior part of the femoral articular surface.
A longitudinal line is marked on the medial part of the femoral cortex parallel to the long axis of the femur proximal and distal to the osteotomy site to ensure that correct rotational alignment is restored after resection of the bone. A closing wedge osteotomy is made 1 cm proximal to the chisel. The base of the osteotomy is made by an oscillating saw while the lateral cortex is perforated in several places with a drill bit and small osteotome. This allows a correction of the deformity while preventing lateral translocation of the proximal fragment. The base of the wedge should be wide enough (5–10 mm) to allow a 90° angle between the chisel and the medial part of the femoral cortex after the wedge is removed. Since the proximal cortical fragment has a smaller diameter it can be easily impacted into the cancellous bone of the distal fragment. This allows an increase in the magnitude of the angular correction if desired. It also provides additional stability and promotes more rapid healing of the osteotomy site.
While the axial alignment of both parts is maintained by adhering to the previously marked longitudinal axis, the 90° offset dynamic compression plate is inserted. If the plate cannot be brought into contact with the medial femoral diaphyseal cortex after inserting the blade, a slot can be created to better accommodate the shoulder of the blade plate until satisfactory contact is achieved. The osteotomised bony wedge is morcellized and used as an autograft along the medial aspect of the osteotomy. With the 90° blade plate positioned properly along the medial part of the femoral cortex, screws are inserted into the plate using compression techniques.
The medial part of the femoral cortex and the transepycondylar femoral line are now at 90° to each other. This results in a desired anatomical tibio-femoral angle of approximately 0°. The vastus medialis is then tacked back to the medial septum using interrupted sutures, and the skin and subcutaneous tissues are closed in a routine fashion.
The postoperative protocol for the series under study requires that active flexion of the knee is started ten to 14 days postoperatively. Weight bearing began at six to eight weeks postoperatively, or when radiographs indicated that the osteotomy was uniting. Full activities were resumed three to six months after surgery (Fig. 4).
Results
Modified Knee Society scores (MKSS) improved significantly (p < 0.01) from a mean of 36.8 points preoperatively to 77.5 points at one-year post DFVO. Prior to DFVO, 32 (97%) patients had poor knee function and one patient had a fair function. At one-year post DFVO, 28 (84.8%) patients had excellent or good knee function scores, while three (9.1%) had fair results and two (6.1%) had poor results.
At ten-year follow-up, knee function was significantly (p < 0.01) worse than one-year post DFVO, with mean MKSS of 66 points (range 25–91). However, these MKSS were still significantly (p < 0.01) better than the preoperative scores. Eighteen (54.5%) knees had good or excellent function, while two knees (6.1%) had fair function and 12 knees (36.4%) had poor function. DFVO was converted to TKA in two patients. These failures (6.1%) that occurred in less than ten years post DFVO (at six years and eight years, respectively), occurred in the only two patients with bilateral DFVOs (1 failure in each patient). Both women were morbidly obese (BMI 41.5 and 43, respectively) with preoperative MKSS of 25 and 31 points.
At most recent follow-up (mean 15.1 years, range 10–25), MKSS declined significantly (p = 0.008) to a mean of 59 (range 15–91). Ten (30.3%) of the 33 knees had a good or excellent result, two (6.1%) had a fair result, and seven (21.2%) had poor results. Of the nine knees with fair or poor results, one patient was on the waiting list for TKA, 20 years after his DFVO, but succumbed to lung carcinoma and was considered a failure. Fifteen (45.4%) DFVOs had been converted to TKA. Thus, a total of 16 (48.5%) of the 33 knees were considered to have failed at a mean time of 15.6 years (range 6–21.5, Table 1).
Similar to the findings in the study group, the one year post DFVO MKSS in the non failed DFVOs were significantly (p < 0.01) better than the preoperative scores (mean 80.2, range 53–91 versus mean 40.9, range 23–65). Although the ten year post DFVO MKSS were lower (mean 70.7, range 25–91) than the one year scores, this difference was not found to be statistically significant (p = 0.23) in this subgroup of patients. The difference compared to the MKSS at one year post DFVO became statistically significant (p = 0.04) only at the 15-year follow-up when mean MKSS further declined to 67.4 points (range 25–91).
The non failed DFVO patients were not significantly (p = 0.25) older than the failed DFVO patients (mean 47.6, range 24–63 versus mean 45.6 points, range 27–67, respectively). However, the preoperative MKSS of the non failed DFVOs were significantly (p = 0.034) higher than the failed DFVOs (mean 40.9 points, range 23–65 versus mean 32.6 points, range 11–65, respectively).
Discussion
Long-term results of DFVO for the treatment of isolated lateral compartment knee arthritis with a valgus deformity is not well documented in the literature. There have been relatively few studies depicting the clinical outcome of these patients. Edgerton et al. [14] reported on 23 patients (24 knees managed with DFVO) and found 71% with good or excellent results at a mean follow-up of 8.3 years. Our institution previously reported that 12 (31.6%) of 38 knees were either converted to TKA or were on a waiting list for conversion to TKA at an average of 123 months (range 39 –245) after DFVO. Wang and Hsu [9] reported satisfactory results in 83% of 30 knees after DFVO at a mean follow-up of 99 months with a ten-year survivorship of 87%.
Since DFVO is intended for the younger and more active population, it is particularly important to examine the long-term success of this procedure, including rates of failure as well as knee function beyond the horizon of a single decade. Such data is both important for patients and for surgeons to possess in order to have a more informed decision regarding the patient's treatment strategy. In this study we present our results for DFVO with minimum follow-up of ten years (mean 15.1, range 10–25) in 33 patients. This series constitutes the longest term follow-up analysis of DFVO in the literature conducted by a single surgeon (AEG), using a single technique over more than two decades.
Patients knee function is expected to consistently and significantly (p < 0.01) improve following DFVO. At one-year follow-up, 28 (84.8%) patients had excellent or good knee function scores, while three (9.1%) had fair results and two (6.1%) had poor results compared to the poor function encountered in 97% of these patients preoperatively. The knee function scores significantly (p < 0.01) deteriorate at ten-year follow up but remain much better (p < 0.01) than before surgery. Only two DFVOs (6.1%) were converted to TKA prior to ten-year follow-up, and both cases were in morbidly obese patients who had bilateral DFVO with extremely poor preoperative knee function. At 15-year follow-up, the knee function further declined resulting in an overall failure rate of 48.5% at a mean follow-up of 15.8 years.
The non failed DFVO subgroup of patients was found to have significantly (p = 0.034) higher preoperative MKSS scores than the non failed group (mean 40.9, range 25–63 versus mean 32.6, range 11–65, respectively). Moreover, the rate of decline in knee function was more gradual. Although the ten-year post DFVO MKSS were lower than the one year scores (mean 70.7, range 25–91 versus mean 80.2, range 53–91, respectively), this difference was not found to be statistically significant (p = 0.23). The decline in knee function became significant (p = 0.04) only at 15 year follow-up when mean MKSS further fell to 67.4 points (range 25–91). Thus, DFVO may provide longer lasting benefit in patients with better preoperative knee function.
This study has certain limitations, which are inherent to the retrospective work of this nature. The number of patients included is limited because of the relatively small prevalence of young and active patients with lateral unicompartmental arthritis and valgus deformity in the population. This is true despite the high volume referral base and catchment area of our institution. Although only three patients were lost to follow-up over the study's prolonged follow-up period, this constitutes 8.3% of the knees. In addition, follow-up review of the patients was not blinded. Since this was not a randomised study, bias and confounders are difficult to control.
In summary, the data presented in this study provides evidence that DFVO is a viable alternative for lateral compartmental knee arthritis for appropriately selected patients. DFVO may reliably assist in delaying the need for TKA by more than a decade as conversion to TKA in less then ten years occurred in 6.1%.
References
Insall JN, Joseph DM, Msika C (1984) High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Joint Surg Am 66:1040–1048
Sprenger TR, Doerzbacher JF (2003) Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty-two years. J Bone Joint Surg Am 85:469–474
Tjörnstrand BA, Egund N, Hagstedt BV (1981) High tibial osteotomy: a seven-year clinical and radiographic follow-up. Clin Orthop Relat Res 160:124–136
Vainionpää S, Läike E, Kirves P, Tiusanen P (1981) Tibial osteotomy for osteoarthritis of the knee. A five to ten-year follow-up study. J Bone Joint Surg Am 63:938–946
Hutchison CR, Cho B, Wong N, Agnidis Z, Gross AE (1999) Proximal valgus tibial osteotomy for osteoarthritis of the knee. Instr Course Lect 48:131–134
Coventry MB (1987) Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee. J Bone Joint Surg Am 69:32–38
Shoji H, Insall J (1973) High tibial osteotomy for osteoarthritis of the knee with valgus deformity. J Bone Joint Surg Am 55:963–973
Coventry MB (1973) Osteotomy about the knee for degenerative and rheumatoid arthritis. J Bone Joint Surg Am 55:23–48
Wang JW, Hsu CC (2006) Distal femoral varus osteotomy for osteoarthritis of the knee. Surgical technique. J Bone Joint Surg Am 88:100–108
McDermott AG, Finklestein JA, Farine I, Boynton EL, MacIntosh DL, Gross A (1988) Distal femoral varus osteotomy for valgus deformity of the knee. J Bone Joint Surg Am 70:110–116
Finkelstein JA, Gross AE, Davis A (1996) Varus osteotomy of the distal part of the femur. A survivorship analysis. J Bone Joint Surg Am 78:1348–1352
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Marti RK, Verhagen RA, Kerkhoffs GM, Moojen TM (2001) Proximal tibial varus osteotomy. Indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am 83:164–170
Edgerton BC, Mariani EM, Morrey BF (1993) Distal femoral varus osteotomy for painful genu valgum. A five to 11 year follow up study. Clin Orthop Relat Res 288:263–269
Backstein D, Morag G, Hanna S, Safir O, Gross A (2007) Long-term follow-up of distal femoral varus osteotomy of the knee. J Arthroplasty 22:2–6
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kosashvili, Y., Safir, O., Gross, A. et al. Distal femoral varus osteotomy for lateral osteoarthritis of the knee: a minimum ten-year follow-up. International Orthopaedics (SICOT) 34, 249–254 (2010). https://doi.org/10.1007/s00264-009-0807-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-009-0807-0