Abstract
In this study, the results of open-wedge osteotomy with Puddu plate for the treatment of varus gonarthrosis have been evaluated prospectively. This study assessed 65 knees of 60 patients with varus gonarthrosis who underwent high tibial osteotomies. Our study population consisted of 13 male and 47 female patients with a mean age of 54 (range 39–76) years. For the clinical evaluation of the patients Hospital of Special Surgery (HSS) score, American Knee Society and Oxford knee scores, and for the radiological assessment mechanical axis deviation (MAD), lateral distal femoral angle (LDFA), medial proximal tibial angle (MPTA), femorotibial angle and Insall-Salvati index were basically taken into consideration. Our patients were followed up for an average of 34 (range 18–60) months. In the last assessments of our cases, mean improvements detected in HSS scores, Oxford knee scores, knee and functional scores of Knee Society were 26.72, 19.18, 49.9, and 30 points, respectively. The radiological examinations revealed that their mechanical axes on the average passed 5.09 mm laterally achieving an average of 6.5° genu valgum, and a mean Insall-Salvati index of 1.09. As complications, superficial wound infection in two patients (3%), implant infections in one patient (1.5%), deep vein thrombosis in two patients (3%), peroperative lateral tibial plateau fracture in one patient (1.5%), and postoperative lateral tibial plateau fracture due to a falling down were encountered. According to the results obtained, postoperative pain resolves promptly and a significant degree of improvement of knee functions of the patients are achieved. Therefore, we believe that high tibial osteotomy with a Puddu plate is a valuable alternative to total knee arthroplasty in cases with varus gonarthrosis. Although early results are satisfactory, long-term follow-up studies are required especially in the middle aged and elderly patient populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unlike inflammatory diseases, abnormality leading to varus gonarthrosis is considered to be a mechanical problem [5, 7, 15, 19]. Among the etiological factors resulting in mechanical problems, tibial and femoral bone deformities, malalignments and malorientations due to the laxities of the lateral ligaments rank first [2, 18]. It is believed that arthrosis develops as a natural consequence of this relevant malalignment [24].
High tibial ostetomy procedure is thought to resolve pain owing to its decompressive effect in early period, while this effect leads to an improvement in knee functions due to the translation of the mechanical axis onto relatively intact lateral tibial plateau in long term, subsequently it prevents the development of arthrosis [3, 5, 13, 19]. Jackson and Waugh [9] first described high tibial osteotomy and Coventry [3] popularized this technique by publishing long-term results. Later various modifications of high tibial ostreotomies were described. Although in 1951 Debeyre [4] delineated medial open-wedge osteotomy technique, it has not been used widely. At the end of 1990s due to the introduction of fixation plate named Puddu into clinical practice, and relative simplicity of the technique [20] the procedure of medial open-wedge osteotomy gained popularity.
In this study we reported early results, together with advantages and disadvantages of early results of medial open-wedge osteotomies we performed for the patients with varus gonarthrosis in the light of current literature.
Materials and methods
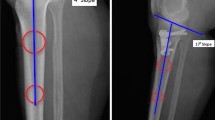
This is a retrospective study evaluating 65 knees of 60 patients who had undergone medial open-wedge osteotomies with Puddu plates performed by two surgeons (ÖT, MA) for the cases with varus gonarthrosis referred to our clinic between April 2000 and December 2003. Thirteen (21.6%) male and 47 (78.4%) female patients were operated for their right (n=23; 38.3%), left (n=32; 53.3%) and both (n=5; 8.3%) knees. The mean age of patients at the time of operation was 54 (range 39–76). In our study group, 59 patients had primary varus gonarthrosis, while one patient suffered from posttraumatic arthrosis. Preoperatively, 12 (20%) patients had been treated with arthroscopic debridement, while 48 cases (80%) received conservative treatment for 1 year. The indication criteria for high tibial osteotomy with Puddu plate were presence of isolated medial compartment arthrosis, good patient motivation to comply with postoperative rehabilitation program, patients aged <65 years, absence of knee contractures and excessive patellofemoral arthrosis, range of motion being at least 90°–100°, varus gonarthrosis requiring <20° correction, stable knees. Pre- and postoperative assessments of our patients were performed using clinical parameters, Hospital for Special Surgery score, American Knee Society’s knee and functional scoring system and Oxford knee scores. For radiological evaluations, AP, lateral and tangential knee radiograms and orthoradiograms were taken (Table 1) [17]. In addition, magnetic resonance imaging (MRI) was used for the assessment of 38 (63%) patients. All the patients received prophylactic treatment for deep vein thrombosis (DVT) for 10 days.
Surgical technique
After preoperative evaluation and preparation of our patients, firstly arthroscopic examination was performed with the patient in the supine position under general anesthesia and additional intraarticular lesions were treated. We used transvers incision for the earliest cases, then we converted it to longitudinal. An approximately 8–10 cm incision was done parallel to the anterior border of the medial collateral ligament adjacent to the anteromedial aspect of the proximal tibia. Superficial medial ligament was dissected from the bone proximally up to the level of osteotomy. Then under the guidance of fluoroscopy, guide wire was advanced medially from 1–2 cm distal to the level of the joint up to the lateral cortex, and osteotomy apparatus was mounted on the guide wire. Afterwards a second Kirschner wire was introduced at an appropriate angle up to the lateral cortex. Osteotomy apparatus and proximal wire were removed. After that, medial, anterior, and posterior cortex was cut immediately under the guide wire up to 1 cm away from the lateral cortex (Fig. 1a). Then using 10, 25, and 35 mm width osteotomes, osteotomy was performed under fluoroscopic control. Osteotomy line was opened and widened with a special wedge shaped spreader (Fig. 1b). Meanwhile the mechanical axis of the lower extremity was measured with special probes. After adequate exposure of the osteotomy line, the osteotomy guide was removed and an appropriate plate was placed inside the osteotomy line. The plate was placed just on the anterior aspect of the medial ligament. Using two 6.5 mm size spongeous or cannulated screws for the proximal and two 4.5 mm size cortical screws for the distal end of the plate the fixation was completed (Fig. 1c). The proximally placed screws were not allowed to come in direct contact with the joints. Finally, using tricortical grafts taken from the iliac ala or spongeous allografts (freeze dried cancellous block MTF(Musculoskeletal Transplant Foundation, Edison, NJ), osteotomy gap was grafted (Fig. 1d). After the closure of the layers and placement of a drain, the patient’s knee was put into a hinged immobilizer.
Postoperative rehabilitation
At approximately 6 weeks postoperatively, the patients were ambulated with knee-hinged immobilizers. Soon after the operation, the patient started isometric quadriceps exercises and used CPM (continuous passive motion) apparatus to ease his/her movements. PCA (patient controlled anesthesia) was used to alleviate postoperative pain and facilitate his/her daily exercises. The patient was rehabilitated with quadriceps muscle and hamstring strengthening exercises. Partial weight bearing exercises were initiated promptly and with gradual increments full weight bearing exercises was assumed at approximately 3 months postoperatively.
Results
Mean follow-up period was 34 (range 18–60) months (Fig. 2a–c). Tricortical autografts removed from the iliac alae and cubic allografts were used equally. In both groups full consolidation was achieved at the osteotomy site at the end of the three postoperative months. We evaluated bone consolidation according to Paley et al. [6, 16, 23]. These include appearing of trabecular formation, bridging of bone ends, and corticalization of three of the four sides at least as seen on anteroposterior and lateral radiographs. On the other hand, we did not observe any plate failure at the end of third month even though we allow patients to bear full weight. According to these criteria, there was no difference between our patients in terms of healing. The sizes and number of the plates we used for our patients are presented in Table 2.
During arthroscopic examination, in all of our patients, arthrosis was observed within the medial compartment and managed arthroscopically. Cartilagenous tissue in the lateral compartment was intact and of good quality. Besides, partial meniscectomies were performed for instable ruptures of 18 (15%) medial and 6 (5%) lateral menisci.
The clinical evaluation of our patients and X-ray results are shown in Table 3 and 4 respectively.
Complications
Two patients (3%) developed superficial wound infection, which healed with antibiotherapy. A deeper wound infection was seen in one patient (1.5%), which healed with open wound management, wound irrigation, debridement, and antibiotherapy. Deep vein thrombosis was detected in two (3%) patients treated satisfactorily with medical therapy and leg elevation. The correction angle of the osteotomy plate was disturbed in one patient due to a fall from a distance in the third postoperative week, and reosteosynthesis was achieved with an Ilizarov type external fixator. The postoperative pain of this patient was resolved, but his functional result improved only moderately. In one patient, during opening of the osteotomy line, lateral tibial plateau was fractured and osteosynthesis achieved safely with fixation of the Puddu plate using proximal screws during the same operative session. On the other hand, undercorrections were observed between 3° varus and 3° valgus in 13 patients. However, functional results were not different in those patients than the entire group. We found that Hospital for Special Surgery (HSS) score, Knee score of Knee Society, Functional score of Knee Society, and Oxford knee score in all group were 88.07, 85.6, 83.5, 39.78, respectively, while these scores in undercorrected group were 86.8, 84.2, 83.1, 39.2, respectively.
Discussion
Varus gonarthrosis is one of the most frequently encountered abnormalities currently seen by orthopedic surgeons. Although morbidities (inflammatory diseases, traumas, disorders of the articular cartrilage) are responsible for this deformity, the mostly seen etiologic factors are genu varum or varus malalignment. Varus malalignment could develop as a result of a dynamic factor due to lateral laxity, however it could occur more often because of a bony deformity [3, 5, 18, 19]. In our study group, primary varus gonarthrosis was detected in 59 patients and the presence of 31.25 mm deviation of the mechanical axis, 83.5° MPTA and 5.7° genu varum indicate the development of varus gonarthrosis due to bony deformities.
The association between varus malalignment and gonarthrosis is not fully understood. An abnormal response of the cartilage to normal stresses or normal reaction of the cartilage against excessive stresses is suggested for this association [24]. Akamatsu et al. [1] in their series consisting 144 knees, detected that mineral densities and sclerosis of medial femoral condyles and tibial bone plateau are denser than those of the lateral compartment assessed using preoperative dual X-ray absorptiometric measurements. They performed high tibial osteotomies for 23 patients and stated that the degree of bone mineral density and sclerosis decreased by distributing mechanical stress evenly and diminishing weight-bearing forces impinging on medial compartment. In a study by Odenbring et al. 189 knees with isolated medial compartment arthrosis were followed up for 16 years. HTO’s and total knee prostheses were carried out for 85 and 33 of these knees, respectively. After 16 years of follow-up of untreated cases, it was revealed that 23 knees were painful with restricted mobility, while in 20 knees arthrosis advanced as demonstrated with radiographic controls [15]. In a study conducted by Hernborg and Nilsson [7], 94 untreated knees with medial arthrosis were followed up radiologically for 10–18 years, and arthrosis was detected deteriorated at the end of the follow-up period. Based on these studies, we believe that the patients with isolated medial compartment arthrosis must be managed surgically and high tibial osteotomy is one of the surgical alternatives for these patients.
To obtain successful results in HTO not only requires the application of a good surgical technique but also depends on appropriate patient selection. The factors which will increase the rate of success obtained from high tibial osteotomy procedures include presence of isolated medial compartment arthrosis, good patient motivation to comply with postoperative rehabilitation program, patients aged <65 years, absence of knee contractures and excessive patellofemoral arthrosis, range of motion being at least 90°–100°, varus gonarthrosis requiring <20° correction, stable knees, and the usage of rigid fixation material for osteosynthesis [3, 5, 10, 13, 19, 21]. In this study period, the patients who did not comply with our criteria (isolated medial compartment arthrosis, range of motion being at least 90°–100°, absence of knee contracture and excessive patellofemoral arthrosis) underwent total knee prosthesis. We selected patients complying with the above inclusion criteria. Successful outcomes found at the last follow-up visits suggest our meticulous concern for the selection of HTO candidates.
Although the patient’s age is an important criterion for classical high tibial osteotomy indication, nowadays chronological age per se is not accepted as a criterion for eligibility. Bone texture, daily activity level, and biological age have a greater impact on selection criteria.
With high tibial osteotomy, lesser weight bearing impact on subchondral bone, decrease of intraosseous venous hypertension and microfractures involving subchondral bone and alleviation of clinical symptoms such as pain and consequently improvement in functional status of the patients are targeted [3, 5, 10, 13, 18, 19]. For high tibial osteotomy, many surgical techniques have been used. So far, Coventry type close wedge osteotomy is the most frequently used technique. However for this osteotomy technique loss of correction, fibular nerve injury, compartment syndrome, delay in bone union or non-union, and intraarticular fractures are among the most frequently reported complications [5, 12, 18, 19, 21, 22]. After innovative definition of the lower extremity deformity and new insight into their management proposed by Paley et al. [18] these authors also recommended reverse focal dome osteotomy and their method of osteosynthesis using circular external fixator. Fairly successful results have been reported with this technique [2, 18, 22]. However, the burden of carrying an uncomfortable apparatus like circular external fixator, frequency of pin track infections, requirement of more frequent control visits, and intensive expertise essential for Ilizarov technique are among important disadvantages of the technique [2, 11, 22].
Since the reports of Debeyre [4] on open-wedge medial osteotomy published in 1951, both the technique and the implants used have undergone considerable modifications. In medial open-wedge osteotomy, fibular osteotomy is not performed, technique does not require a wide exposure and a stable fixation can be accomplished with a Puddu plate without loss of correction. Besides, anterior cruciate ligament (ACL) reconstruction can be achieved using the same incision. Furthermore, this technique also reserves bone stock to be used for possible future total knee prosthesis and provides the desired degree of correction. In addition, it is perfectly comfortable for the patient. Hernigou et al. [8] followed 93 cases with arthrosis of the medial compartment that had undergone open-wedge osteotomies for a median of 11.5 years, and reported that the results obtained were satisfactory up to 7 years postoperatively. Magyar et al. [12] practiced medial open-wedge osteotomy with hemicallotasis (25 knees) or close wedge osteotomy (25 knees) for 50 knees of 46 patients, and reported that after 2 years of follow-up, clinical scores had improved in both groups without a significant difference between groups. Success in medial open-wedge osteotomy depends largely on sound application of the technique. The determination of the exact localization of the osteotomy site accurately under a good fluoroscopic control, meticulous care not to fracture lateral cortex during opening of the osteotomy site, frequent assessment of the correction angle at every step of the operation, avoidance of overcorrection, the selection of an appropriate Puddu plate size fit for the osteotomy gap are important details increasing the success rate of this procedure [20]. Based on median 34 month follow-up of our patients, mean improvements obtained in HSS scores, American Knee Society’s knee and functional scores, and Oxford knee scores were 26.72, 49.9, 30, and 19.18 points, respectively. According to these four assessment scales, preoperative scores were deemed “worse”, and postoperative scores were “good”. In addition, the radiological examinations revealed that the mechanical axes on the average passed 5.09 mm laterally achieving an average of 6.5°genu valgum, and a mean Insall-Salvati index of 1.09. We are in the opinion that early outcomes of our medial open-wedge osteotomies with Puddu plates are fairly successful and safe. Besides when compared with the results reported in the literature for high tibial osteotomies our success rates are found to be similar or slightly better [2, 3, 8, 10, 12, 14, 21, 22].
One of the most important complications reported for either close or open wedge osteotomies is patella infera or alta [3, 8, 12, 14, 21, 22]. Based on postoperative Insall-Salvati index, we didn’t encounter neither patella infera nor patella alta in our patient group. We attributed this outcome to meticulous selection of inclusion criteria, avoidance of postoperative casting and initiation of early rehabilitation program.
Different complication rates ranging between 2 and 51% were reported for medial open-wedge osteotomy procedures. These include over or undercorrection, non-union or delayed union on the osteotomy site, problems related to fibular nerve and vessels, traumatic injuries of anterior and posterior arteries, compartment syndrome, deep vein thrombosis, pulmonary embolism, infection, dysthesias around the incision line, fractures of the lateral cortex and tibial plateau and inadequate stabilization [10, 11, 14]. However, complication rates due to pin track infections are reportedly higher especially in series related to the application of external fixators. The complication rates in our series are also in accordance with those reported in the literature.
Many authors have reported that a slight overcorrection with 3°–6° valgus position influenced long-term outcomes favorably [2, 3, 8, 10, 18, 20, 21, 22]. Coventry et al. [3] stated that they had obtained successful results in varus or neutral (64%) and in 4°–6° valgus (94%) positions. In a study by Hernigou et al. [8] arthrosis did not deteriorate in patients maintained in 3°–6° valgus position. In our study group, mechanical axes passed through 5.09 laterally, and we obtained a median 6.5° valgus position. We believe that this approach had a favorable impact on the early improvement of functional status, and also thought that it might prevent the deterioration of arthrosis owing to the even distribution of mechanical weight bearing forces in the long run. However, we did not observe poor functional results in patients who had undercorrection. We think that this result comes from our short follow-up period. In early postoperative period, most of patients are satisfied because osteotomy results in decompressive effect on bone. Then this effect alleviates pain and consequently provides a good functional status in short term, while a good outcome after high tibial osteotomy depends on the distribution of overload to healthy compartment in long term. Therefore, this study should be supported by another studies with longer follow-up.
Shorter follow-up periods and lack of comparative results are shortcomings of this study. However, early results obtained indicate that medial open-wedge osteotomies using Puddu plates could be realized safely with considerable success with encouraging outcomes, and this technique could be a good alternative for unicompartmental total knee arthroplasty. Comparative studies with longer follow-up periods will be required to demonstrate its favorable effects on arthrosis in the long term.
References
Akamatsu Y, Koshino T, Saito T , Wada J (1997) Changes in osteosclerosis of the osteoarthritic knee after high tibial osteotomy. Clin Orthop 334:207–214
Catagni MA, Guerreshi F, Ahmad TS, Cattaneo R (1994) Treatment of genu varum in medial compartment osteoarthritis of the knee using the ilizarov method. Orthop Clin North Am 23(5):509–514
Coventry MB, Ilstrup DM, Walrichs SL (1993) Proximal tibial osteotomy. A critical long-term follow-up study of eigthy-seven cases. J Bone Joint Surg (Am) 75(2):196–201
Debeyre J, Artigou JM (1972) Long-term results of 260 tibial osteotomies for frontal deviations of the knee. Rev Chir Orthop Reparatrice Appar Mot 58:335–339
Dutkowsky JP (1992) Miscellaneous nontraumatic disorders. In: Crenshaw AH (ed) Campbell’s operative orthopaedics, 8th edn. vol 3. Mosby, St. Louis, pp 2005–2057
Fischgrund J, Paley D, Suter C (1994) Variables affecting time to bone consolidation during limb lengthening. Clin Orthop 301:31–37
Hernborg JS, Nilsson BE (1977) The natural course of untreated osteoarthritis of the knee. Clin Orthop 123:130–137
Hernigou PH, Medeivelle D, Debjre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen years follow-up study. J Bone Joint Surg (Am) 69(3):332–354
Jackson JP, Waugh W (1961) Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg (Br) 43(7):746–751
Lobenhoffer P, Agneskirchner JD (2003) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11(3):132–138
Magyar G, Toksvig-Larsen S, Lindstrand A (1999) Hemicallotasis open-wedge osteotomy for osteoarthritis of the knee. J Bone Joint Surg (Br) 81(3):449–451
Magyar G, Ahl TL, Vibe P, Toksvig-Larsen S, Lindstrand A (1999) Open-wedge osteotomy by hemicallotasis or the closed-wedge technique for osteoarthritis of the knee. J Bone Joint Surg (Br) 81(3):444–448
Murphy SB (1994) Tibial osteotomy for genu varum: indications, preoperative planning, and technique. Orthop Clin North Am 3:477–482
Nakamura E, Mizuta H, Kudo S, Takagi K, Sakamato K (2001) Open-wedge osteotomy of the proximal tibia with hemicallotasis. J Bone Joint Surg (Br) 83(8):1111–1115
Odenbring S, Lindstrand A, Egund N, Larsson J, Heddson B (1991) Prognosis for patients with medial gonarthrosis. A 16 year follow-up study of 189 knees. Clin Orthop 266:152–155
Paley D (1990) Problems, obsctacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop 250:81–104
Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A (1994) Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am, 35(3):425–465
Paley D, Maar DC, Herzenberg JE (1994) New concepts in high tibial osteotomy for medial compartment osteoarthritis. Orthop Clin North Am 25(3):483–498
Phillips MJ, Krachow KA (1998) High tibial osteotomy and distal femoral osteotomy for valgus or varus deformity around the knee. AAOS instructional course lectures 47:429–436
Puddu G (2003) Personal communication. International symposium on operative and biologic treatments in sport medicine, Colonia, 2003
Rinonapoli E, Mancini GB, Coruaglia A, Nusiello S (1998) Tibial osteotomy for varus gonarthrosis. Clin Orthop 353:185–193
Sen C, Kocaoglu M, Eralp L (2003) The advantages of circular external fixation used in high tibial ostetomy. Knee Surg Sports Traumatol Arthrosc 11(3):139–144
Shefelbine SJ, Simon U, Claes C et al (2005) Prediction of fracture callus mechanical properties using micro-CT images and voxel-based finite element analysis. Bone 36:480–488
Tetsworth K, Paley D (1994) Malalignment and degenerative arthropathy. Orthop Clin North Am 25(3):367–377
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Asik, M., Sen, C., Kilic, B. et al. High tibial osteotomy with Puddu plate for the treatment of varus gonarthrosis. Knee Surg Sports Traumatol Arthrosc 14, 948–954 (2006). https://doi.org/10.1007/s00167-006-0074-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-006-0074-1