Abstract
Purpose
A consistent post-operative limb positioning regime could be an attractive, simple and cost-effective alternative to improve patient’s outcomes after total knee arthroplasty (TKA). The aim of this study was to perform a systematic review of the available literature in order to understand whether a consistent post-operative limb positioning regime could affect blood loss and range of motion (ROM) after TKA.
Methods
A search was performed using the keywords “total knee replacement/knee prosthesis” in combination with “post-operative management”, “blood loss”, “range of motion”, “leg position”, “flexion”, “extension” and “splinting” regardless of the year of publication. The scientific databases have been accessed in order to identify papers dealing with post-operative limb positioning regimes after TKA.
Results
Seven articles matching the inclusion criteria were selected. Blood loss and ROM were both investigated in all but one paper, in which only blood loss was evaluated. There were six randomized controlled trials and one prospective comparative study. A 48–72 h post-operative knee flexion protocol seems to be effective in reducing blood loss and increasing ROM following TKA. We did also find no benefit in using extension splints in the immediate post-operative period.
Conclusions
Based on the studies undertaken to date, a 48–72 h post-operative knee flexion protocol should be implemented as an easy and inexpensive method of reducing blood loss and increasing ROM following TKA. Shorter flexion regimes failed to influence these parameters.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is a highly effective treatment for knee osteoarthritis and recent reports highlighted the growing use of TKA in the last decade [18, 30]. Furthermore, TKA has the highest aggregate cost among the 2004–2007 top ten most rapidly increasing procedures in the USA [18], and many efforts have been made to improve functional recovery and reduce the length of hospital stay following this procedure [7]. The early restoration of a satisfactory knee range of motion (ROM) can improve patient’s discharge and a decreased transfusion rate could make the procedure cheaper. Different strategies have been recently implemented to reduce blood loss and increase ROM that are thought to be two important factors in determining the outcomes of TKA [1, 11]. Many of these strategies such as the use of blood reinfusion systems [22, 28], different drainages management protocols [32], antifibrinolytic medications [5, 17, 25, 31], continuous passive motion machines [21] and minimally invasive and computer-aided surgical techniques [3, 4, 16, 29] imply strains on hospital resources, use of expensive equipments or dedicated surgical instrumentations. Limb position in the immediate post-operative period could theoretically affects blood loss and ROM following TKA, and the reduction in transfusion requirement associated with ROM improvement could conversely reduce the overall costs [24, 27]. Particularly, it can be hypothesized that knee flexion can reduce bleeding because of the angulation of popliteal vessels, and the subsequent reduced hidden blood loss can improve ROM recovery [15].
Although a consistent post-operative limb positioning regime could be an attractive, simple and cost-effective alternative to improve patient’s outcomes after TKA, the ideal limb management is still under debate [14]. A full extended position with compressive dressing applied to the knee has been traditionally proposed [19], notwithstanding various post-operative limb positioning regimes could be ideally implemented. If proven to be effective in reducing blood loss and increasing ROM, an adequate post-operative limb positioning regime could be an inexpensive and easily reproducible method to maximize functional recovery.
The aim of this study was to understand whether a consistent post-operative limb positioning regime could effectively improve ROM restoration and reduce blood loss following TKA. The currently available literature was analyzed in order to provide an answer to those questions.
Materials and methods
A search was performed using the keywords “total knee replacement/knee prosthesis” in combination with “post-operative management”, “blood loss”, “range of motion”, “leg position”, “flexion”, “extension” and “splinting” regardless of the year of publication. Scientific databases have been accessed in order to identify papers dealing with post-operative limb positioning regimes after TKA.
The following databases were accessed on 1 June 2013: PubMed (http://www.ncbi.nlm.nih.gov/sites/entrez/); Ovid (http://www.ovid.com); Cochrane Reviews (http://www.cochrane.org/reviews/); and Google Scholar. All journals were considered, but only English papers were taken into account. Literature reviews, instructional courses, biomechanical and in vitro reports, surgical techniques and letters to the editors were excluded. Two authors (MD, FT) read the abstracts and excluded the articles that were considered unrelated to the topic of the study. When the abstract was not available, the title of the paper was used to judge its relevance. In case of doubt about inclusion of an article, the senior author (CF) made the decision.
A cross-referencing process was used to find further relevant publications from the retained articles. The papers were analyzed searching information regarding post-operative limb position regimes, blood loss and ROM after TKA.
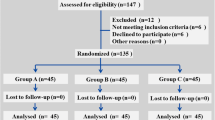
From a total number of 1,415 retrieved articles, after abstract or title page evaluation 1,374 articles not matching the inclusion criteria were excluded. The full text version of the remaining 41 articles was obtained, and the reference lists were screened, finding another article relevant to the topic at hand. The contents of these 42 articles were then discussed by all co-authors, and 35 papers not dealing with post-operative limb positioning regimes following TKA were excluded, thus leaving 7 articles available for the review (Fig. 1).
Two of us (MP, AS) independently assessed the methodological quality of the papers according to the Cochrane Bone, Joint and Muscle trauma Group quality assessment tool [26], and any final disagreement was resolved by the senior Author’s decision. This form allows to rate the methods of randomization, the presence of blinded assessors, the type of outcomes assessed, the effectiveness of clinical tests used, etc. (see http://bjmtg.cochrane.org/sites/bjmtg.cochrane.org/files/uploads/Coding%20Manual.pdf).
Data from the relevant articles were collected onto an anonymous data extraction form.
Results
As previously discussed, 7 articles matched the inclusion criteria [8, 9, 14, 19, 20, 23, 33]. There were one prospective comparative study [8] and six randomized controlled trials [9, 14, 19, 20, 23, 33]. Blood loss and ROM were both evaluated in all but one [20] study, in which only blood loss was investigated. Details about the type of study, level of evidence, demographics pre-operative statistical differences between the groups and total number of patients involved were summarized in Table 1.
The inclusion criteria were exhaustively described in five articles [9, 14, 19, 23, 33], and a power analysis was performed in four [9, 14, 19, 20]. As a result, the adequate definition of inclusion parameters in association with the statistical assessment of the correct samples size was present in three articles [9, 14, 19].
Randomization using the closed envelope technique was realized in four studies [9, 19, 23, 33], calendar randomization [20] and random number list [14] were used in the other two.
The same standardized surgical technique was applied in six studies [8, 9, 14, 20, 23, 33]. In the paper by Ma et al. [19], lateral release for patellar maltracking was performed in six patients in the flexion group and in one patient in the extension group; however, statistical subgroup analysis revealed no difference in the results excluding these patients.
The operations were performed by a single surgeon in one paper and [8] by different surgeons in four papers [9, 14, 19, 23]; no indications regarding the operating surgeons were supplied in the remaining two papers [20, 33]. Since implant design is thought to influence ROM [2] implants used were evaluated founding four studies [14, 19, 20, 33] in which the same prosthetic model was implanted. Although Horton et al. [9] reported the use of the same prosthetic design, patella was replaced in four out of 23 cases in the splint group and in three out of 25 cases in the no-splint group, with no statistical difference.
Post-operative limb position protocols involved the use of extension splints [9, 33], short [19, 20, 23] or long flexion regimes [8, 14] (Table 2). Active quadriceps exercises, straight leg raise initiatives and active or passive ROM exercises using continuous passive motion machines were commenced during the first [8, 14, 19] or the second [9] post-operative day, and rehabilitation protocols were not described in three studies [20, 23, 33].
A blinded outcome assessment was present in only two studies, whose quality level was higher [9, 14] (Table 3). Three studies revealed significant differences in terms of blood loss [14, 23, 33] (Table 4). Significant results pertaining to ROM were reported in three papers [8, 14, 33] (Table 5).
Length of hospitalization was assessed in five articles [8, 9, 19, 20, 23], and no difference were recorded in 4 [9, 19, 20, 23]. In the remaining article [8], hospitalization averaged 9.00 days in the flexion group and 10.04 days in the extension group (p = 0.048).
Complication rates were similar between groups in five papers [8, 14, 19, 23, 33], and complications were not mentioned in one [20]. Horton et al. [9] found 1 wound complication in the no-splint group, 1 deep vein thrombosis, 1 fatal pulmonary embolism and 1 case of stiffness requiring manipulation under anaesthesia in the splint group.
Discussion
The most important finding of the present study is that 2–3 day post-operative knee flexion protocols could effectively improve the outcomes of TKA.
Total knee arthroplasty (TKA) gained increasing popularity over recent years, and both the annual rate of procedures and the overall costs are expected to grow over the next decades [13, 18, 30]. In order to reduce the burden on health-care resources, many attempts have been made to improve functional results, whose are strongly influenced by blood loss reduction and ROM restoration [1, 11]. In this contest, the development of a consistent strategy of post-operative limb management could be a simple and inexpensive way to maximize the cost-effectiveness of this surgery.
This systematic review brought together and summarized the results of different studies pertaining to the effect of post-operative limb positioning on blood loss and ROM following TKA. Our goal was to ascertain whether a consistent post-operative limb positioning regime could effectively improve ROM restoration and reduce blood loss following TKA.
Based on the studies undertaken to date, a 48–72 h post-operative knee flexion protocol should be implemented as an easy and inexpensive method of reducing blood loss and increasing ROM following TKA. Shorter flexion regimes failed to influence these parameters. We also did not find any benefit in using extension splints in the immediate post-operative period (Fig. 2). Although the quality of evidence available seems to be satisfactory, since only prospective studies or randomized trials have been included in this review, no definitive conclusions can be drawn about the amount of flexion required.
Vessels angulation due to different degrees of knee flexion and the increased local tension due to the decreased venus return could explain the reduced bleeding, and the results of this study suggested this mechanism to be effective only for 48 h or longer flexion protocols. The decreased swelling and hidden blood loss in turns facilitate ROM restoration by reducing intraarticular pressure and capsular tension.
We acknowledge some limitations in this study. First, the noticeable heterogeneity in outcome measures and the presence of different subgroup analysis ranging from 2 to 4 throughout the seven retained manuscripts precluded the possibility of a more structured and accurate aggregation and comparison of the results. Second, this study failed to demonstrate a correlation between post-operative limb management and length of hospitalization, which should be considered the most relevant factor in improving TKA cost-effectiveness. However, since manifold factors can influence length of hospitalization following TKA [10], it seems too hard to isolate the effect of blood loss reduction and ROM restoration on this parameter.
The seven retained articles were analyzed in terms of methodological quality, randomization methods, sample size and outcome measures.
Methodological quality appears to be sufficient (Table 3) and this is in line with the level of evidence of the retrieved studies (Table 1). However, it must be emphasized that blinded outcome assessors were present in only two studies (Table 3); therefore, biases in the reporting of subjective outcome measures (i.e. ROM) could be expected. On the other hand, the objective general difficulties in conducting randomized controlled trials in an orthopaedic setting should mitigate this assignment.
Post-operative limb position regimes were very different among the studies since the effectiveness of short (24 h or less) high-degree flexion protocols [19, 20, 23] or longer protocols (48 h or more) involving mild [14] or high [8] degree of knee flexion and the use of post-operative extension splints [9, 33] were investigated (Table 3). Regimes duration rather than knee position seems to be the most relevant difference.
Noticeable variability among the selected articles was also recorded regarding the parameters used to measure blood loss and ROM. The thorough assessment of blood loss, by measuring total blood loss [6], hidden blood loss and knee circumference, which indirectly refers to hidden blood loss [15], was present just in one study [14], different parameters were variously estimated in other five papers [9, 19, 20, 23, 33], whereas Hewitt et al. [8] did not mention the method of blood loss estimation (Table 3).
Range of motion (ROM) restoration was consistently evaluated in three studies [9, 14, 33] in which fixed flexion deformity, early and late ROM following TKA were assessed, whereas just early [23] or late [8, 17] ROM was investigated in the other three articles (Table 3).
In the light of the results of this systematic review, the duration of post-operative knee flexion seems to be crucial, since longer post-operative flexion regimes proved to be beneficial. Li et al. [14] showed better results in terms of hidden blood loss, knee circumference and early ROM using a 72-h mild knee and hip flexion regime. The authors claim that hidden blood loss reduction positively affects rehabilitation after TKA because it reduces knee swelling and joint effusion, which in turn arouse quadriceps inhibition and quadriceps weakness [14, 26]. Hewitt et al. [8] reported significantly better late ROM using a 90° knee flexion regime 48 h post-operatively, without blood loss difference. However, blood loss was inconsistently evaluated in this paper. Shorter regimes ranging from 6 to 24 h of post-operative knee flexion failed to influence blood loss and ROM [19, 20, 23]. Although knee flexion for 48–72 h post-operatively determines outcomes improvement, it was suggested that prolonged knee flexion following surgery might increase the risk of wound complications [12] making it necessary closer patient’s monitoring. However, no difference in complication rates were found in 4 out of 5 studies comparing flexion to extension regimes [8, 14, 19, 23], and no mention to complications was reported in the other one [20]. Finally, another possible concern with flexion protocols is the likely increase in discomfort.
The use of extension splint revealed to be ineffective [9] or even harmful in terms of ROM restoration [33]. Drain volume reduction was reported by Zenios et al. [33] in the splint group; however, no differences in transfusion rates were found, and hidden blood loss was not estimated.
Only one paper [8] reported a significant reduction in the length of hospital stay following a 48-h knee flexion protocol; nevertheless, this statement is questionable since a lot of different variables can theoretically influence hospitalization after TKA [10], and no difference in hospitalization was reported in other four papers [9, 19, 20, 23].
Conclusion
Longer post-operative knee flexion protocols seem to be effective in reducing blood loss and increasing ROM following TKA, and the use of extension splint revealed no benefit (Fig. 2). These findings suggest that long post-operative knee flexion protocols should be implemented as an easy and cost-effective way to improve the outcomes of TKA.
References
Carson JL, Duff A, Poses RM, Berlin JA, Spence RK, Trout R, Noveck H, Strom BL (1996) Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet 348(9034):1055–1060
Dennis DA, Heekin RD, Clark CR, Murphy JA, O’Dell TL, Dwyer KA (2013) Effect of implant design on knee flexion. J Arthroplast 28(3):429–438
Fickert S, Jawhar A, Sunil P, Scharf H-P (2012) Precision of Ci-navigated extension and flexion gap balancing in total knee arthroplasty and analysis of potential predictive variables. Arch Orthop Trauma Surg 132:565–574
Fu Y, Wang M, Liu Y, Fu Q (2012) Alignment outcomes in navigated total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 20:1075–1082
Gillette BP, DeSimone LJ, Trousdale RT, Pagnano MW, Sierra RJ (2013) Low risk of thromboembolic complications with tranexamic acid after primary total hip and knee arthroplasty. Clin Orthop Relat Res 471:150–154
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anesthesiology 58(3):277–280
Den Hertog A, Gliesche K, Timm J, Mühlbauer B, Zebrowski S (2012) Pathway-controlled fast-track rehabilitation after total knee arthroplasty: a randomized prospective clinical study evaluating the recovery pattern, drug consumption, and length of stay. Arch Orthop Trauma Surg 132(8):1153–1163
Hewitt B, Shakespeare D (2001) Flexion vs. extension: a comparison of post-operative total knee arthroplasty mobilisation regimes. Knee 8(4):305–309
Horton TC, Jackson R, Mohan N, Hambidge JE (2002) Is routine splintage following primary total knee replacement necessary? A prospective randomised trial. Knee 9(3):229–231
Husted H, Holm G, Jacobsen S (2008) Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 79(2):168–173
Jergesen HE, Poss R, Sledge CB (1978) Bilateral total hip and knee replacement in adults with rheumatoid arthritis: an evaluation of function. Clin Orthop Relat Res 137:120–128
Johnson DP (1993) Infection after knee arthroplasty. Clinical studies of skin hypoxia and wound healing. Acta Orthop Scand Suppl 252:1–48
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89(4):780–785
Li B, Wen Y, Liu D, Tian L (2012) The effect of knee position on blood loss and range of motion following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(3):594–599
Li B, Wen Y, Wu H, Qian Q, Lin X, Zhao H (2009) The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop 33(5):1263–1268
Liebensteiner MC, Krismer M, Koller A, Semenitz B, Mayr E (2012) Does minimally invasive total knee arthroplasty improve isokinetic torque? Clin Orthop Relat Res 470(11):3233–3239
Lin P-C, Hsu C-H, Huang C-C, Chen W-S, Wang J-W (2012) The blood-saving effect of tranexamic acid in minimally invasive total knee replacement: is an additional pre-operative injection effective? J Bone Joint Surg Br 94(7):932–936
Losina E, Thornhill TS, Rome BN, Wright J, Katz JN (2012) The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am 94(3):201–207
Ma T, Khan RJK, Carey Smith R, Nivbrant B, Wood DJ (2008) Effect of flexion/extension splintage post total knee arthroplasty on blood loss and range of motion—a randomised controlled trial. Knee 15(1):15–19
Madarevic T, Tudor A, Sestan B, Santic V, Gulan G, Prpic T, Ruzic L (2011) Postoperative blood loss management in total knee arthroplasty: a comparison of four different methods. Knee Surg Sports Traumatol Arthrosc 19(6):955–959
Maniar RN, Baviskar JV, Singhi T, Rathi SS (2012) To use or not to use continuous passive motion post-total knee arthroplasty presenting functional assessment results in early recovery. J Arthroplast 27(2):193–200
Muñoz M, Ariza D, Garcerán MJ, Gómez A, Campos A (2005) Benefits of postoperative shed blood reinfusion in patients undergoing unilateral total knee replacement. Arch Orthop Trauma Surg 125(6):385–389
Ong SM, Taylor GJSC (2003) Can knee position save blood following total knee replacement? Knee 10(1):81–85
Raut S, Mertes SC, Muniz-Terrera G, Khanduja V (2012) Factors associated with prolonged length of stay following a total knee replacement in patients aged over 75. Int Orthop 36(8):1601–1608
Roy SP, Tanki UF, Dutta A, Jain SK, Nagi ON (2012) Efficacy of intra-articular tranexamic acid in blood loss reduction following primary unilateral total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(12):2494–2501
Schröder D, Pässler HH (1994) Combination of cold and compression after knee surgery. A prospective randomized study. Knee Surg Sports Traumatol Arthrosc 2(3):158–165
Voorn VMA, Marang-van de Mheen PJ, So-Osman C, Vlieland TPMV, Koopman-van Gemert AWMM, Nelissen RGHH, van Bodegom-Vos L, LISBOA Study Group, Brand A, Engberts DP, van der Hout WB, Kaptein AA, van Mourik JBA (2012) Designing a strategy to implement cost-effective blood transfusion management in elective hip and knee arthroplasties: a study protocol. Implement Sci 7:58
Watts CD, Pagnano MW (2012) Minimising blood loss and transfusion in contemporary hip and knee arthroplasty. J Bone Joint Surg Br 94(11 suppl A):8–10
Wegrzyn J, Parratte S, Coleman-Wood K, Kaufman KR, Pagnano MW (2013) The John Insall award: no benefit of minimally invasive TKA on gait and strength outcomes: a randomized controlled trial. Clin Orthop Relat Res 471:46–55
Weinstein AM, Rome BN, Reichmann WM, Collins JE, Burbine SA, Thornhill TS, Wright J, Katz JN, Losina E (2013) Estimating the burden of total knee replacement in the United States. J Bone Joint Surg Am 95(5):385–392
Yang Z-G, Chen W-P, Wu L-D (2012) Effectiveness and safety of tranexamic acid in reducing blood loss in total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am 94(13):1153–1159
Al-Zahid S, Davies AP (2012) Closed suction drains, reinfusion drains or no drains in primary total knee replacement? Ann R Coll Surg Engl 94(5):347–350
Zenios M, Wykes P, Johnson DS, Clayson AD, Kay P (2002) The use of knee splints after total knee replacements. Knee 9(3):225–228
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faldini, C., Traina, F., De Fine, M. et al. Post-operative limb position can influence blood loss and range of motion after total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 23, 852–859 (2015). https://doi.org/10.1007/s00167-013-2732-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2732-4