Abstract
Purpose
This study prospectively assessed the effects of knee position on blood loss and range of motion after primary total knee arthroplasty (TKA).
Methods
One hundred and ten consecutive TKA patients were randomized into flexion group and extension group. Both groups had the leg elevated 30° at the hip over an inactive CPM for 72 h postoperatively. The flexion group had the knee flexed to 30° during this period. The extension group had the knee extended fully. Perioperative blood loss, hidden blood loss, knee swelling, ecchymosis, analgesia requirements, range of motion (ROM), fixed flexion deformity (FFD), straight-leg raising action, and postoperative complications within 6 weeks of surgery were measured for evaluation and comparison.
Results
The postoperative hidden blood loss, knee swelling, and scope of ecchymosis were significantly lower in the flexion group than in the extension group, and ROM and straight-leg raising action were significantly higher during the early period after operation. No significant difference was observed in perioperative blood loss, the amount of morphine used, or FFD in the early postoperative period or in ROM and FFD at 6 weeks postoperatively.
Conclusions
The findings of this study indicate that flexion of the knee to 30° with the leg elevated 30° at the hip after total knee arthroplasty may mitigate knee swelling and provide other beneficial results during the early rehabilitation following TKA.
Level of evidence
Prospective comparative study, Level I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blood loss and range of motion (ROM) following total knee arthroplasty (TKA) are thought to be contributing factors to functional outcomes. Blood loss due to extensive soft tissue release and bone cuts in TKA may result in a significant anemia and prolonged postoperative recovery [1], while recovery of a good range of motion is vital for an optimal functional result, and small changes in maximum flexion can have profound effects on functional capability [9]. To improve the TKA result, many factors directly and indirectly related to these two outcomes have been studied. These have included tourniquet use during operation [13], various drain placement protocols [21], postoperative cryotherapy [11], minimally invasive surgery, such as TKA with navigation system [2, 12], bipolar sealer versus standard electrocautery [15], autologous platelet gel [7], and postoperative limb positioning [6, 8, 14, 18, 22]. Postoperative limb positioning has been proposed as a simple and cost-effective way to maximize patient outcomes. Recently published studies investigating the effect of different limb positioning regimens on functional outcome after TKA have reported promising but inconsistent results. A recent review of the literature found no papers that have investigated the effect of the mild knee flexion (less than 45°) following TKA [6, 8, 14, 18, 22]. Therefore, to evaluate the potential benefits of mild knee flexion, the authors have performed a prospective randomized study comparing outcomes in patients with their knees placed in 30° flexion or in full extension postoperatively. The hypothesis of this study is that mild knee flexion (to 30°), in comparison to full extension, decreases blood loss and improves ROM post-TKA.
Materials and methods
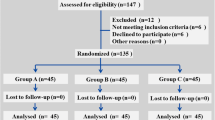
All patients who underwent primary TKA in our institution during an 11-month period starting in September 2008 were enrolled in this prospective study. The approval of the institutional review board and informed consent from all participants were obtained. One hundred and ten consecutive patients suffering from primary osteoarthritis and rheumatoid arthritis were included in the study. Exclusion criteria were as follows: bilateral TKA planned either simultaneously or within a 3-month interval, diabetes, hemostasis defect, history of peripheral vascular disease, malignant tumor, preoperative hemoglobin level less than 10 g/dL, previous thromboembolism.
For randomization, a random number list was generated, and upon entering the study, each patient was assigned a number. An equal number of patients (55) was assigned to each group. Patients in both groups had the affected leg elevated 30° at the hip over an inactive CPM postoperatively; patients in the flexion group had the knee flexed to 30°; patients in the extension group had the knee extended fully. The CPM machine was removed at 72 h postoperation. Patients in the two groups were well matched for age, gender, body mass index (BMI), preoperative diagnosis, preoperative hemoglobin (Hb) and hematocrit (Hct), preoperative circumference at the superior patellar pole, and preoperative range of motion of the knee (Table 1).
Surgical technique
The type of anesthesia varied according to patient. Each procedure was performed by one of a group of four staff surgeons. The implant used was the posterior cruciate ligament substituting total knee prosthetic component (GENESIS II, Smith & Nephew Inc., Memphis, TN, USA). No tourniquets were used. An anterior mid-line skin incision facilitated a mid-vastus approach. Bone cuts and soft tissue balancing were done in the same sequence. The patella was reshaped to better match the shape of the femoral component trochlea. To reduce the blood loss from the femoral hole, an intramedullary plug with bone grafts was used before closure of the wound. A wool and crepe bandage was applied followed by a compressive dressing. No drains were used in the wounds. None of the patients required transfusion during the operation. The transfusion trigger was a hemoglobin level of less than 9 g/dL measured at 24 h postoperatively.
Postoperative management
All patients received standard thromboprophylaxis in the form of low molecular weight heparin and early mobilization. Every patient was provided with patient-controlled analgesia system machines (PCAS) for 48 h postoperatively and thereafter maintained on NSAID-based analgesia. The wound dressing was changed when soaked or if wrapped so tightly as to hinder the blood circulation of the extremity. Active isometric quadriceps, initiative straight-leg raising, and extension-flexion motion were encouraged immediately after operation, and ambulation with partial weight bearing was permitted at 24 h postoperatively under the supervision of a physical therapist. During the first 72 h postoperatively, the affected leg would always be placed back over the inactive CPM after physical therapy. The study data were documented by a single surgeon to avoid inter-observer error. To ensure that the examining surgeon was blinded to the postoperative limb position, the CPM was removed before any examination during the first 72 h postoperatively.
Outcome assessment
The following parameters were measured for each patient.
Calculated total blood loss (CBL)
CBL was calculated using the formula reported by Nadler et al. [17] and Gross [5]. The hematocrit (Hct) value used in the formula was measured preoperatively and at 24 h postoperatively.
Hidden blood loss (HBL)
HBL was calculated by subtracting the intraoperative blood loss (IBL) and the postoperative wound blood loss (PWBL) from the CBL at the 24th postoperative hour. IBL was estimated by adding the volume in suction bottles after subtraction of wound irrigation fluid to the net blood weight of the sponges used during the procedure. PWBL was approximated by weighing the soaked dressings and converting this measurement to volume.
Knee swelling
Knee circumference (KC) at the level of the superior patellar pole was measured preoperatively and at 3 and 7 days postoperatively, and the increase compared with the preoperative measurement was calculated.
Ecchymosis
The scope of ecchymosis around the affected knee was calculated by the palm method at 3 days postoperatively.
Analgesia
The total amount of morphine delivered postoperatively via a PCAS over a 48-h period was recorded.
ROM
The arc of knee flexion was measured preoperatively and at 3 days, 7 days, and 6 weeks postoperatively.
FFD
FFD was measured preoperatively and at 3 days, 7 days, and 6 weeks postoperatively. The number of patients in each group who were able to conduct initiative straight-leg raising to more than 60° at 1, 3, and 7 days postoperatively was recorded.
Complications
All complications were recorded. Any clinical suspicion of DVT was promptly investigated by Doppler ultrasound or venogram.
Statistical analysis
A power analysis was performed to determine the number of patients necessary to distinguish significant differences in blood loss, ROM, and the fixed flexion deformity (FFD) at the follow-up intervals. A difference of 100 mL in blood loss, 10° of motion, and 1° in FFD were considered clinically significant. The sample size required to detect these differences with a confidence level of 95% and a power of 80% is 52 knees per group.
Statistical analysis was performed with SPSS 16.0 software for Windows. Continuous data with normal distribution were expressed as means (± standard deviation). Normality of the data was checked by use of the Kolmogorov–Smirnov tests. The unpaired t test was used for comparisons of normally distributed continuous data. Chi-square test was used for the comparison of nominal data. Differences at a level of P < 0.05 were considered statistically significant.
Results
The results below are shown in Table 2. The CBL following TKA was 1,168 (±211) mL in the flexion group and 1,231 (±206) mL in the extension group. The difference in CBL between the two groups was not statistically significant (n.s.). However, the hidden blood loss was significantly greater in the extension group (P < 0.05). The increase in circumference of the affected knee and the area of surrounding ecchymosis were also significantly greater in the extension group than in the flexion group (P < 0.001), which corresponded with the hidden blood loss results.
There were similar results in both groups in the amount of morphine used during the first 48 h postoperatively (n.s.) and in FFD at 3 days, 7 days, and 6 weeks postoperatively (n.s.). The range of active knee flexion at 3 and 7 days postoperatively and the number of people conducting straight-leg raising initiatively at 1 and 3 days postoperatively were significantly greater in the flexion group (P < 0.001, 0.05, 0.05 and 0.05, respectively), which indicated that the flexion placement was beneficial to the early postoperative rehabilitation. No difference was found in the range of active knee flexion at 6 weeks postoperatively or in the number of people conducting straight-leg raising initiatively at 7 days postoperatively (n.s.). Each group had one patient who developed wound infection in the early postoperative period. These patients were treated with intravenous antibiotics and surgical debridement. No patients in either group developed DVT.
Discussion
The most important finding of the study was the statistically significant correlation between postoperative knee placement in mild flexion and decreased hidden blood loss, reduced edema, and early benefit to postoperative rehabilitation excises when compared with knee extension. This finding supports to the hypothesis the authors have stated in the introduction, i.e., mild knee flexion (to 30°), in comparison with full extension, decreases blood loss and improves ROM after TKA. A consistent postoperative extremity positioning regimen is an easy and cost-efficient technique that can potentially improve functional outcomes. There are currently a limited number of studies examining the effects of postoperative limb positioning on blood loss and ROM following TKA. The content of the available studies varies widely, and the results are inconsistent.
In this study, all of the patients in both groups had their leg to elevated 30° at the hip. The main difference between the two groups was the knee position that was either flexed to 30° or extended fully. The intent was to avoid potential confounding factors related to hip position. One et al. [18] compared the effects of three different postoperative positioning regimens on blood loss: knee extension with the leg horizontal, knee extension with the leg elevated 35° at the hip, and knee flexion to 70° with the leg elevated 35° at the hip. They found that in both the knee flexion and knee elevated in extension groups, the calculated hemoglobin loss was 25% less than in the horizontal group. Thus, it was postulated that elevation of the leg rather than the flexion of knee caused the benefit. Ma et al. [14] randomized 49 patients into two groups: knee flexed to 70° with the leg elevated 70° at the hip and knee extended fully with the leg horizontal. They found that there was no significant difference between the two groups in postoperative blood loss. Although each of the two studies above included a group in which patients had the knee flexed to 70°, the findings of effect on blood loss are contrary. In addition to differences in patient demographics, surgical technique, the types of implant, and the postoperative regimens in each study, it is noted that the position of the hip in the patients of the two groups was different. It is possible that if the angle of hip flexion is too great, the femoral vein will be so curved as to hinder venous blood return. Similarly, with an excessive angle of knee flexion, the popliteal vein might be so curved as to hinder venous return. On the other hand, if the knee is extended fully, the popliteal vein may strain, which could also hinder venous blood backflow. This might be the reason that no difference was found in patients in the limb-elevated groups in One’s study. In the present study, the hidden blood loss decreased significantly in patients with the leg elevated 30° at the hip and the knee flexed to 30° versus patients with the hip flexed to 30° and the knee extended fully, which seems to substantiate this point. The hidden blood loss after TKA has been estimated to be about 55% of the calculated blood loss [13]. While differences in hidden blood loss between the two groups were statistically significant in the present study, the trend toward lower calculated blood loss in the knee flexion group did not reach statistical significance.
Important clinical indicators of hidden blood loss, which is generally defined as residual blood loss into the joint space and extravasation into the tissues, are limb swelling and ecchymosis [3, 16]. In this study, the rate of knee swelling and the scope of ecchymosis around the affected knee were significantly lower in the knee flexion group than in the knee extension group, which is consistent with the hidden blood loss data. Minimizing hidden blood loss is beneficial to the rehabilitation after TKA for the following reasons: (1) Joint effusion causes quadriceps inhibition by reduced afferent activity of intracapsular receptors, resulting in quadriceps weakness [20]; (2) Swelling may produce an increased weight in the affected limb sufficient to require more muscle force for conducting straight-leg raising activities; and (3) Knee swelling increases the tension of soft tissues around the affected knee, impeding the knee flexion motion and possibly inhibiting maximal wound healing because of decreased oxygen tension at the skin edges. In this study, the patients in the knee flexion group had statistically better outcomes in ROM and straight-leg raising activities than those in the extension group. The reasons for this might include the three points above. Although the active knee flexion at the sixth week postoperatively and the straight-leg raising by the seventh day postoperatively no longer showed a significant difference between the two groups, the more effective rehabilitation exercises in the relative early period can strengthen patient confidence and resolve, decrease the incidence of complications (particularly DVT) [20], and increase patient comfort.
FFD plays a major role in the functional outcome of primary TKA. If flexion contractures are present after TKA, pain scores, function scores, and KSS are much more likely to be adversely affected than if knee extension is normal [19]. Traditionally, the placement of the affected knee in full extension post-TKA has been thought to be an effective way to prevent FFD. However, in this study, the rate of FFD in knee flexion patients was not significantly higher than in the knee extension patients. In addition to the observations recorded above, the common anecdotal observation that patients tend to respond to knee swelling automatically by slightly flexing their knee into a more comfortable position [4] may further support the conclusion that postoperative placement in mild flexion can improve outcomes. Johnson has reported that knee flexion following TKA might increase wound complications by lowering oxygen tension in the wound edges [10]. However, in theory, the reduced oxygen tension in the wound edges secondary to mild knee flexion should be offset by the increased oxygen tension favored by the decrease in postoperative swelling. Accordingly, in the present study, the knee flexion patients did not have increased wound problems compared with the extension group patients.
Limitations of the current study include the relatively small sample size. A power analysis has been performed to determine the necessary sample size based on blood loss, ROM, and FFD. The lack of comparison with a third cohort group, which would include patients who had their knees flexed beyond 45° post TKA, is another potential limitation.
Despite these limitations, this study seems to demonstrate an important and clinically relevant finding, adding further support to the theory that optimal postoperative limb positioning is a simple and cost effective method of maximizing TKA patient outcomes.
Conclusion
The results in the present study support the hypothesis that mild flexion of the knee to 30° with the leg elevated 30° at the hip post TKA is an easy and effective way to decrease hidden blood loss, mitigate knee swelling, and provide benefit to the early postoperative rehabilitation exercises.
References
Carson JL, Duff A, Poses RM, Berlin JA, Spence RK, Trout R, Noveck H, Strom BL (1996) Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet 348:1055–1060
Chotanaphuti T, Ongnamthip P, Teeraleekul K, Kraturerk C (2008) Comparative study between computer assisted-navigation and conventional technique in minimally invasive surgery total knee arthroplasty, prospective control study. J Med Assoc Thai 91:1382–1388
Erskine JG, Fraser C, Simpson R, Protheroe K, Walker ID (1981) Blood loss with knee joint replacement. J R Coll Surg Edinb 26:295–297
Fehring TK, Odum SM, Griffin WL, McCoy TH, Masonis JL (2007) Surgical treatment of flexion contractures after total knee arthroplasty. J Arthroplasty 22(62):6 Suppl 2–6 Suppl66
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anesthesiology 58:277–280
Hewitt B, Shakespeare D (2001) Flexion vs. extension—a comparison of postoperative total arthroplasty mobilisation regimes. Knee 8:305–309
Horstmann WG, Slappendel R, van Hellemondt GG, Wymenga AW, Jack N, Everts PA (2011) Autologous platelet gel in total knee arthroplasty: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 19:115–121
Horton TC, Jackson R, Mohan N, Hambidge JE (2002) Is routine splintage following primary total knee replacement necessary? A prospective randomised trial. Knee 9:229–231
Jergeson HE, Poss R, Sledge CB (1978) Bilateral total hip and knee replacements in adults with rheumatoid arthritis: an evaluation of function. Clin Orthop Relat Res 137:120–128
Johnson DP (1993) Infection after knee arthroplasty. Clinical studies of skin and wound healing. Acta Orthop Scand Suppl 252:1–48
Kullenberg B, Ylipää S, Söderlund K, Resch S (2006) Postoperative cryotherapy after total knee arthroplasty: a prospective study of 86 patients. J Arthroplasty 21:1175–1179
Lee DH, Choi J, Nha KW, Kim HJ, Han SB (2011) No difference in early functional outcomes for mini-midvastus and limited medial parapatellar approaches in navigation-assisted total knee arthroplasty: a prospective randomized clinical trial. Knee Surg Sports Traumatol Arthrosc 19:66–73
Li B, Wen Y, Wu H, Qian Q, Lin X, Zhao H (2009) The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop 33:1263–1268
Ma T, Khan RJ, Carey Smith R, Nivbrant B, Wood DJ (2008) Effect of flexion/extension splintage post total knee arthroplasty on blood loss and range of motion—a randomised controlled trial. Knee 15:15–19
Marulanda GA, Krebs VE, Bierbaum BE, Goldberg VM, Ries M, Ulrich SD, Seyler TM, Mont MA (2009) Hemostasis using a bipolar sealer in primary unilateral total knee arthroplasty. Am J Orthop (Belle Mead NJ) 38:E179–E183
Mylod AG, France MP, Muser DE, Parsons JR (1990) Perioperative blood loss associated with total knee arthroplasty. A comparison of procedures performed with and without cementing. J Bone Joint Surg Am 72:1010–1012
Nadler SB, Hidalgo JU, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51:224–232
Ong SM, Taylor GJ (2003) Can knee position save blood following total knee replacement? Knee 10:81–85
Ritter MA, Lutgring JD, Davis KE, Berend ME, Pierson JL, Meneghini RM (2007) The role of flexion contracture on outcomes in primary total knee arthroplasty. J Arthroplasty 22:1092–1096
Schröder D, Pässler HH (1994) Combination of cold and compression after knee surgery. Knee Surg Sports Traumatol Arthrosc 2:158–165
Stucinskas J, Tarasevicius S, Cebatorius A, Robertsson O, Smailys A, Wingstrand H (2009) Conventional drainage versus four hour clamping drainage after total knee arthroplasty in severe osteoarthritis: a prospective, randomised trial. Int Orthop 33:1275–1278
Zenios M, Wykes P, Johnson DS, Clayson AD, Kay P (2002) The use of knee splints after total knee replacements. Knee 9:225–228
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, B., Wen, Y., Liu, D. et al. The effect of knee position on blood loss and range of motion following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20, 594–599 (2012). https://doi.org/10.1007/s00167-011-1628-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1628-4