Abstract
Purpose
The objective of this study was to compare the clinical and radiologic results of preserved ligament remnants in the selective bundle anterior cruciate ligament (ACL) reconstruction and totally sacrificed ligament remnant in the double-bundle ACL reconstruction in order to confirm the evidence of selective bundle reconstruction.
Methods
This retrospective comparative study was conducted for comparison between preserved ligament remnants in the selective bundle ACL reconstruction and totally sacrificed ligament remnant in the double-bundle ACL reconstruction. From 2008 to 2010, 16 patients (group I) underwent selective bundle ACL reconstruction and 30 patients (group II) underwent double-bundle ACL reconstruction. Clinical, stability and radiologic results (tunnel locations of femoral tunnels using 3-D computed tomography and graft signal intensity using magnetic resonance imaging) were compared.
Results
In comparison with functional results, no statistical differences in the Lysholm, Tegner and International Knee Documentation Committee scores were observed between the two groups (n.s.). In comparison with stability results between the two groups, no statistical differences were observed in the Lachman, pivot shift and anterior drawer stress tests using a Telos® device at 30° and 90° flexed positions (n.s.). In evaluation of the femoral tunnel location, no statistical significant differences in the tunnel position were observed between the groups (n.s.). No statistically significant differences in signal intensity were observed between the two groups (n.s.).
Conclusions
Compared to the double-bundle ACL reconstruction, selective bundle ACL reconstruction produced comparable clinical and radiologic results. Selective bundle ACL reconstruction could be performed instead of double-bundle ACL reconstruction if some intact bundle exists.
Level of evidence
Comparative study, Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction targets replication of the anatomy of the native ACL, and thus, double-bundle ACL reconstruction is gaining popularity because it is mainly composed of two bundles, anteromedial (AM) and posterolateral (PL) bundles [10, 15, 36]. These strategies are supported by evidence demonstrating superior clinical outcomes when graft placement is aligned with the native ACL, and lesser tunnel widening and cartilage degeneration have been reported after double-bundle reconstruction [14, 16, 18–20, 23, 30, 31, 39].
However, during the reconstruction, relatively well-preserved remnants are sometimes encountered, and it is questionable to sacrifice all of these remnants because the confirmation of anatomic footprints is essential in the double-bundle reconstruction. It has been suggested that these remnants could improve knee function, stability and graft healing [1, 6, 9, 11, 28]. Accordingly, selective bundle ACL reconstruction is being attempted in patients who have relatively intact bundles [3, 6, 27, 28, 33].
A partial tear of the ACL is a very common injury pattern, accounting for 10 to 35 % of ACL tears, although the incidence of a symptomatic AM or PL bundle tear is reported to be between 5 and 10 % [6, 24, 26, 28, 35]. However, the definition of a partial tear is vague and less is known about the fate of preserved remnants after selective AM or PL bundle ACL reconstruction [5, 24, 25, 28]. In addition, few studies comparing the results of selective bundle reconstruction with those of the anatomic double-bundle ACL reconstruction have been reported.
This study was designed for the confirmation whether the preserved remnant bundle that was relatively intact during a single-bundle reconstruction could be comparable to the double-bundle reconstruction and selective bundle reconstruction could be performed instead of double-bundle ACL reconstruction if some intact bundle exists. The objective of this study was to compare the clinical and radiologic results of preserved ligament remnants in the selective bundle ACL reconstruction and totally sacrificed ligament remnant in the double-bundle ACL reconstruction to confirm the evidence of selective bundle reconstruction. It was hypothesized that selective bundle ACL reconstruction would show comparable clinical and radiologic results that were comparable to those of the double-bundle ACL reconstruction.
Materials and methods
To verify our hypotheses, a retrospective comparative study was conducted for comparison between preserved ligament remnants in the selective bundle ACL reconstruction and totally sacrificed ligament remnant in the double-bundle ACL reconstruction. From 2008 to 2010, ACL surgery was performed in 92 patients, and of these, 16 patients (group I) underwent selective bundle (single bundle) ACL reconstruction and 30 patients (group II) underwent double-bundle ACL reconstruction. Other 46 patients underwent conventional single-bundle ACL reconstruction without intact bundle. Institutional review board approval was obtained prior to initiation of the study, and all patients provided informed consent for participation (GIBRA2823-2012).
All patients who underwent ACL reconstruction were symptomatic, and indications for selective bundle ACL reconstruction were as follows: (1) positive physical examination (anterior or rotatory instability), (2) a visible tear by magnetic resonance imaging (MRI), (3) and the most important point was that there was a relatively intact bundle during surgery. For checking out the intact bundle, the AM bundle was checked at 90° of knee flexion and the PL bundle was checked in the figure of 4 positions [35, 37]. All patients who underwent selective bundle ACL reconstruction fulfilled the above-mentioned criteria. Double-bundle reconstruction was performed in patients with no intact bundle and remnant tissue was sacrificed.
Exclusion criteria were as follows: (1) single-bundle ACL reconstruction showing completely torn ACL (46 patients in this period), (2) multiple ligamentous injuries (posterior cruciate ligament, PL corner injury, medial collateral ligament injury which required surgical repair or reconstruction), revision surgery, or previous surgery around the affected knee, combined fracture of the affected lower extremity, and bilateral tears [37].
Evaluation methods
Lysholm and International Knee Documentation Committee (IKDC) scores were used for the assessment of clinical results. Stability was evaluated using Lachman, pivot shift and anterior drawer stress tests using a Telos® device (Telos, Weterstadt, Germany) at 30° and 90° flexed positions.
For the evaluation of anatomic tunnel location, tunnel locations of femoral tunnels were assessed by 3-D computed tomography (CT). Postoperative CT scans (SIEMENS SOMATOM Definition, SIEMENS, Forscheim, Germany) were performed during hospital stays. Subsequently, 3-D surface models were produced using somaris/7 syngo CT 2008G software (Syngo CT Workplace VA20A, SIEMENS, Forscheim, Germany) using the EBW workstation (v3.5.0, Philips Medical Systems, Best/NL). Measurements were performed using a PiViewSTAR (v 5.0.9.2, INFINITT, Seoul). Positions of femoral tunnels were measured using an anatomic coordinate axes method (ACAM). Centres of femoral tunnel apertures were determined from 3-D CT reconstruction images and compared with reference data [10, 21].
In some patients, postoperative MRI (3-T MRI (Siemens Magnetom Verio, SIEMENS, PA, USA)) was performed at 12 months (range 12–24 months) in group I (7, 43.8 % patients) and at 12 months (range 6–25 months) in group II (11, 36.7 % patients). Graft status was measured quantitatively using regionalized MR signal intensities and complications, such as cyclops lesion and graft failure. Measurements were carried out using sagittal, coronal and oblique coronal images. The larger parts of ACLs, from the origin to insertion, were reconstructed using AQUARIS (Aquarius, TERARECON, CA) along the course of graft. Graft status was graded using the Howell grading system [13]. Intra-articular portions of grafts were divided into three portions, and signal intensities were analysed using sagittal T2-weighted turbo spin echo images in each portion and graded as follows: (1) normal signal, (2) >50 % of total graft volume with a normal signal, (3) <50 % of total graft volume with a normal signal and (4) 100 % of graft with an increased signal. In order to check intra- and interobserver bias, all CT and MRI measurements were made twice (with an interval of 2 weeks) by two orthopaedic surgeons.
Surgical technique
Double-bundle ACL reconstruction
A 3-strand semitendinosus graft was used for the AM bundle and a 4-strand gracilis tendon graft was used for the PL bundle. For femoral tunnel formation, with the knee flexed at 90°, the arthroscope was inserted through the AM portal and a femoral guide set at a 90° angle was inserted through the central portal. The tip of the guide pin was pointed at the central portion of the footprint of each bundle using an outside-in technique. For AM and PL tunnel formation, a bony landmark, such as, the lateral bifurcated ridge or lateral intercondylar ridge was used5. For tibial tunnel formation, the tip of the guide pointed at the central portion of the footprint of each bundle. Femoral and tibial tunnel positions were confirmed using an image intensifier. If tunnel positions were acceptable, reaming according to the graft diameter was performed.
Selective bundle reconstruction
Using the anatomic reconstruction concept, the ruptured bundle was identified and carefully debrided, while preserving the intact bundle (Fig. 1). In addition, an effort was made to retain the ruptured bundle as much as possible. A standard AM portal was used for visualization with the knee flexed at 90°.
For AM bundle reconstruction, the tip of the guide pin of the femoral tunnel was pointed at the centre of the AM bundle footprint. The tip of the guide pin for tibial tunnel was also pointed at the centre of the stump, and the guide pin was identified by making a longitudinal incision on the remnant. Finally, we confirmed femoral and tibial tunnel positions using an intraoperative image intensifier. For PL bundle reconstruction, the method was similar with AM bundle and the femoral footprint of the PL bundle was accessed easily in figure of 4 positions. The tip of the guide pin for tibial ACL insertion was also pointed at the centre of the remnant which is usually the centre of interspinous area.
Postoperative rehabilitation
All patients began immediately active quadriceps isometric exercise and active range of motion (ROM) exercise. Three days after surgery, a pair of crutch was used to allow partial weight bearing. Four or five days after surgery, ACL brace was put on and joint motion exercise was conducted by 15° increment by week. At 4 weeks after surgery, 90° motion was allowed, and at 8 weeks after surgery, 130° motion was allowed. At 6 months after surgery, straight line running was allowed, and at 9 months after surgery, changing the direction while running was allowed.
Statistical analysis
The sample size was 16 and 30 for each group, and the alpha was 0.05 and the power was 64 %. Statistical analysis was performed using SPSS (Statistical Package for Social Science 19, IBM, USA). Wilcoxon’s signed-rank test, the paired T test, the independent T test and the Mann–Whitney U test were used to analyse clinical and radiologic results. p values of <0.05 were considered statistically significant.
Results
Group I consisted of 14 male and two female patients, with a mean age of 30.6 ± 9.7 years. Seven patients received AM bundle reconstruction and nine underwent PL bundle reconstruction. Group II consisted of 24 male and six female patients, with a mean age of 33.9 ± 11.4 years. Mean follow-up duration was 29.5 ± 7.4 months (ranging from 16 to 32 months) in group I and 35 months ± 8.6 in group II. Preoperative demographic data did not differ significantly between the two groups.
Range of motion and functional results were not statistically different between the two groups (n.s.) (Table 1). In comparison with stability results between the two groups, no statistical differences were observed (n.s.) (Table 2). In comparison with operation time, the mean operation time of group I and group II was 65 ± 9.2 and 95 ± 13.4 min, respectively. The double-bundle reconstruction showed longer operation time with statistical significance.
In evaluation of the femoral tunnel location, inter- and intraobserver reliabilities for tunnel measurement were satisfactory, with mean values of 0.82 (ranging from 0.77 to 0.88) and 0.84 (ranging from 0.78 to 0.91). The posterior–anterior direction of the PL tunnel showed an anterior position, and the proximal to distal direction of PL tunnel showed a proximal position versus reference data in both groups (p < 0.05 and p < 0.05, respectively) [10, 21]. No statistically significant differences were observed in the tunnel position of the AM bundle (Table 3).
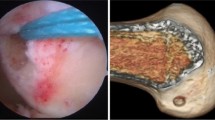
Postoperative MRI was available for seven patients in group I and 11 patients in group II at mean of 12 months after surgery (ranging from 12 to 24 months and 10 to 25 months, respectively). They want to know the status of the reconstructed ligament, and other patients did not want to check MRI because of high cost. Inter- and intraobserver reliabilities for the measurement of signal intensity were satisfactory, with mean values of 0.84 (ranging from 0.75 to 0.89) and 0.81 (ranging from 0.75 to 0.9). No cyclops-like mass lesion was observed, and all patients had an intact ACL graft. In group I, mean values of signal intensity were 2.4 (femoral), 2.1 (mid-substance) and 2.4 (tibial). In group II, mean values were 1.9 (femoral), 2.5 (mid-substance) and 2.0 (tibial). No statistically significant differences were observed between the two groups (Fig. 2).
Discussion
The principal findings of this study were as follows: (1) clinical and stability results of selective bundle ACL reconstruction were not statistically different from those of double-bundle ACL reconstruction, (2) tunnel locations of the two groups were not statistically different, although both groups showed a slight deviation compared to the anatomic locations, and (3) graft status was not statistically different in the comparison using a follow-up MRI.
The most important difference between single-bundle and selective bundle reconstruction, as defined in the current study, is that the remnant bundle is sacrificed and tunnelling is targeted at the whole foot print during single-bundle reconstruction, whereas selective tunnelling is determined by the torn bundle during selective bundle reconstruction. For the conventional ACL reconstruction techniques, sacrificing the remaining ligament and limited notchplasty is recommended for improving visualization and to avoid tissue impingement [12]. Remnant preservation could have potential problems, such as (1) increasing the risk of non-anatomic ACL positioning due to poor visualization, (2) technically demanding, (3) cyclops formation and (4) graft passage difficulties [3, 7].
However, many studies have demonstrated that a preserved remnant could have advantages and have been trying remnant-preserving reconstruction [4, 6, 29, 40]. In terms of mechanical stability, it was reported that the ACL remnant helps to prevent anterior knee laxity in approximately 20 % of cases, and other studies have also supported the role of the remnant bundle in stability [1, 22]. In our study, the results of Lachman, pivot shift and postoperative side-to-side differences of anterior displacement showed significant improvement, compared with the values of preoperation, and no statistical differences in the postoperative values were observed between the two groups. These findings could imply that selective bundle ACL reconstruction could provide stability comparable to that of the double-bundle ACL reconstruction.
Zantop et al. [42] reported that partial rupture of the ACL can be diagnosed by stress radiography, because greater translation is observed at 90° of knee flexion for an AM bundle tear and at 30° of knee flexion for a PL bundle tear. In the present study, anterior translation as determined using stress radiographs at 30° and 90° of flexion in the group I were not significantly different for AM and PL bundle tears (Table 2). In our opinion, it is suspected that delicate partial tear does not occur in a real injury situation and some overlapping between AM and PL bundle could occur in the partial injury [2]. However, the presence of a partial ACL tear could be suspected by stress radiography because mean anterior translation was less for partial ACL tears, compared with that of total ACL rupture, although no statistical significance was observed.
Tunnel position is an important factor in terms of normal knee kinematics and graft incorporation [15, 34, 36]. In terms of PL bundle placement, a slight deviation compared to the anatomic location was observed in both groups, and this could be interpreted that the PL bundle was located more inferiorly and posteriorly and restoration of normal insertion without damage to cartilage would be difficult [21, 39, 41]. However, the locations of both bundles did not differ significantly in the two groups, indicating that selective bundle ACL reconstruction using the outside-in technique could not cause greater mal-positioning of the tunnel location.
On graft status, preservation of remnant ACL could have potential advantages, such as remnants contribute to revascularization of grafted tendons and preserved synovium plays an important role in extracellular formation [1, 9, 11]. In the current study, we evaluated signal intensities of grafts at around 1-year postoperatively using the Howell grading system. No significant intergroup difference was observed, and relatively high intrasubstance ACL graft signals were observed around graft cores in both groups. The reasons for these findings could be interpreted according to the following explanations. First, the time required for complete resolution of such graft signal changes differs between individuals [8]. Second, as described by Saupe et al. [32], increased signal intensity may be observed at more than 4 years after surgery despite complete ligamentization. Third, as reported by Yasuda et al. [38], double-bundle reconstruction has a relatively wider area of contact with the bone tunnel, which might have a positive effect on graft healing. In four cases of second-look operation in group I, good synovialization and taut grafts were observed (<3 mm of translation on probing) (Fig. 3) [17]. These findings suggest that simultaneous consideration of the graft integrity, morphological changes and signal intensity should be considered when MRI is used for postoperative evaluation.
The clinical relevance of this study is that intact bundle could have some values in partial tears. Therefore, selective bundle reconstruction for the injured bundle could be performed instead of double-bundle ACL reconstruction if intact bundle exists. This study has several limitations that must be considered. First, the definition of a partial tear could be subjective. Therefore, there would be the possibility of selection bias. In addition, optimal indications and procedures used for selective ACL reconstruction have not been determined. Second, the study group is little small (power: 64 %) and the follow-up period is relatively short. However, the inclusion criteria were delicate, and then, it was inevitable. Third, the number of MRI acquisition is small and further study is needed to clarify our results. Finally, although it was guessed, it was impossible to prove the biological merits of selective bundle ACL reconstruction.
Conclusion
Compared to the double-bundle ACL reconstruction, selective bundle ACL reconstruction produced comparable clinical and radiologic results. Selective bundle ACL reconstruction could be performed instead of double-bundle ACL reconstruction if some intact bundle exists.
References
Adachi N, Ochi M, Uchio Y, Sumen Y (2000) Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg 120:128–133
Ahn JH, Lee YS, Ha HC (2009) Anterior cruciate ligament reconstruction with preservation of remnant bundle using hamstring autograft: technical note. Arch Orthop Trauma Surg 129:1011–1015
Ahn JH, Wang JH, Lee YS, Kim JG, Kang JH, Koh KH (2011) Anterior cruciate ligament reconstruction using remnant preservation and a femoral tensioning technique: clinical and magnetic resonance imaging results. Arthroscopy 27:1079–1089
Araujo PH, van Eck CF, Macalena JA, Fu FH (2011) Advances in the three-portal technique for anatomical single- or double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 19:1239–1242
Bak K, Scavenius M, Hansen S, Norring K, Jensen KH, Jorgensen U (1997) Isolated partial rupture of the anterior cruciate ligament. Long-term follow-up of 56 cases. Knee Surg Sports Traumatol Arthrosc 5:66–71
Borbon CA, Mouzopoulos G, Siebold R (2012) Why perform an ACL augmentation? Knee Surg Sports Traumatol Arthrosc 20:245–251
Buda R, Ferruzzi A, Vannini F, Zambelli L, Di Caprio F (2006) Augmentation technique with semitendinosus and gracilis tendons in chronic partial lesions of the ACL: clinical and arthrometric analysis. Knee Surg Sports Traumatol Arthrosc 14:1101–1107
Claes S, Verdonk P, Forsyth R, Bellemans J (2011) The “ligamentization” process in anterior cruciate ligament reconstruction: what happens to the human graft? A systematic review of the literature. Am J Sports Med 39:2476–2483
Deie M, Ochi M, Ikuta Y (1995) High intrinsic healing potential of human anterior cruciate ligament. Organ culture experiments. Acta Orthop Scand 66:28–32
Forsythe B, Kopf S, Wong AK, Martins CA, Anderst W, Tashman S, Fu FH (2010) The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Joint Surg Am 92:1418–1426
Gohil S, Annear PO, Breidahl W (2007) Anterior cruciate ligament reconstruction using autologous double hamstrings: a comparison of standard versus minimal debridement techniques using MRI to assess revascularisation. A randomised prospective study with a one-year follow-up. J Bone Joint Surg Br 89:1165–1171
Harner CD, Giffin JR, Dunteman RC, Annunziata CC, Friedman MJ (2001) Evaluation and treatment of recurrent instability after anterior cruciate ligament reconstruction. Instr Course Lect 50:463–474
Howell SM, Clark JA, Blasier RD (1991) Serial magnetic resonance imaging of hamstring anterior cruciate ligament autografts during the first year of implantation. A preliminary study. Am J Sports Med 19:42–47
Jepsen CF, Lundberg-Jensen AK, Faunoe P (2007) Does the position of the femoral tunnel affect the laxity or clinical outcome of the anterior cruciate ligament-reconstructed knee? A clinical, prospective, randomized, double-blind study. Arthroscopy 23:1326–1333
Kaseta MK, DeFrate LE, Charnock BL, Sullivan RT, Garrett WE Jr (2008) Reconstruction technique affects femoral tunnel placement in ACL reconstruction. Clin Orthop Relat Res 466:1467–1474
Kawaguchi Y, Kondo E, Kitamura N, Kai S, Inoue M, Yasuda K (2011) Comparisons of femoral tunnel enlargement in 169 patients between single-bundle and anatomic double-bundle anterior cruciate ligament reconstructions with hamstring tendon grafts. Knee Surg Sports Traumatol Arthrosc 19:1249–1257
Kondo E, Yasuda K (2007) Second-look arthroscopic evaluations of anatomic double-bundle anterior cruciate ligament reconstruction: relation with postoperative knee stability. Arthroscopy 23:1198–1209
Lee S, Kim H, Jang J, Seong SC, Lee MC (2012) Comparison of anterior and rotatory laxity using navigation between single- and double-bundle ACL reconstruction: prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 20:752–761
Lee YS, Jeong YM, Sim JA, Kwak JH, Kim KH, Nam SW, Lee BK (2013) Specific compartmental analysis of cartilage status in double-bundle ACL reconstruction patients: a comparative study using pre- and postoperative MR images. Knee Surg Sports Traumatol Arthrosc 21:702–707
Lee YS, Lee SW, Nam SW, Oh WS, Sim JA, Kwak JH, Lee BK (2012) Analysis of tunnel widening after double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 20:2243–2250
Lee YS, Sim JA, Kwak JH, Nam SW, Kim KH, Lee BK (2012) Comparative analysis of femoral tunnels between outside-in and transtibial double-bundle anterior cruciate ligament reconstruction: a 3-dimensional computed tomography study. Arthroscopy 28:1417–1423
Liu W, Maitland ME, Bell GD (2002) A modeling study of partial ACL injury: simulated KT-2000 arthrometer tests. J Biomech Eng 124:294–301
Musahl V, Bedi A, Citak M, O’Loughlin P, Choi D, Pearle AD (2011) Effect of single-bundle and double-bundle anterior cruciate ligament reconstructions on pivot-shift kinematics in anterior cruciate ligament- and meniscus-deficient knees. Am J Sports Med 39:289–295
Noyes FR, Bassett RW, Grood ES, Butler DL (1980) Arthroscopy in acute traumatic hemarthrosis of the knee. Incidence of anterior cruciate tears and other injuries. J Bone Joint Surg Am 62(687–695):757
Noyes FR, Mooar LA, Moorman CT 3rd, McGinniss GH (1989) Partial tears of the anterior cruciate ligament. Progression to complete ligament deficiency. J Bone Joint Surg Br 71:825–833
Ochi M, Adachi N, Deie M, Kanaya A (2006) Anterior cruciate ligament augmentation procedure with a 1-incision technique: anteromedial bundle or posterolateral bundle reconstruction. Arthroscopy 22(463):e461–e465
Ochi M, Adachi N, Uchio Y, Deie M, Kumahashi N, Ishikawa M, Sera S (2009) A minimum 2-year follow-up after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy 25:117–122
Ohsawa T, Kimura M, Kobayashi Y, Hagiwara K, Yorifuji H, Takagishi K (2012) Arthroscopic evaluation of preserved ligament remnant after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy 28:807–817
Park SY, Oh H, Park SW, Lee JH, Lee SH, Yoon KH (2012) Clinical outcomes of remnant-preserving augmentation versus double-bundle reconstruction in the anterior cruciate ligament reconstruction. Arthroscopy 28:1833–1841
Pinczewski LA, Salmon LJ, Jackson WF, von Bormann RB, Haslam PG, Tashiro S (2008) Radiological landmarks for placement of the tunnels in single-bundle reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 90:172–179
Plaweski S, Grimaldi M, Courvoisier A, Wimsey S (2011) Intraoperative comparisons of knee kinematics of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19:1277–1286
Saupe N, White LM, Chiavaras MM, Essue J, Weller I, Kunz M, Hurtig M, Marks P (2008) Anterior cruciate ligament reconstruction grafts: MR imaging features at long-term follow-up—correlation with functional and clinical evaluation. Radiology 249:581–590
Serrano-Fernandez JM, Espejo-Baena A, Martin-Castilla B, De La Torre-Solis F, Mariscal-Lara J, Merino-Ruiz ML (2010) Augmentation technique for partial ACL ruptures using semitendinosus tendon in the over-the-top position. Knee Surg Sports Traumatol Arthrosc 18:1214–1218
Shen W, Forsythe B, Ingham SM, Honkamp NJ, Fu FH (2008) Application of the anatomic double-bundle reconstruction concept to revision and augmentation anterior cruciate ligament surgeries. J Bone Joint Surg Am 90(Suppl 4):20–34
Siebold R, Fu FH (2008) Assessment and augmentation of symptomatic anteromedial or posterolateral bundle tears of the anterior cruciate ligament. Arthroscopy 24:1289–1298
Tashman S, Collon D, Anderson K, Kolowich P, Anderst W (2004) Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med 32:975–983
van Eck CF, Lesniak BP, Schreiber VM, Fu FH (2010) Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy 26:258–268
Yasuda K, Kondo E, Ichiyama H, Kitamura N, Tanabe Y, Tohyama H, Minami A (2004) Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 20:1015–1025
Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H (2006) Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy 22:240–251
Yasuda K, Kondo E, Kitamura N, Kawaguchi Y, Kai S, Tanabe Y (2012) A pilot study of anatomic double-bundle anterior cruciate ligament reconstruction with ligament remnant tissue preservation. Arthroscopy 28:343–353
Zantop T, Haase AK, Fu FH, Petersen W (2008) Potential risk of cartilage damage in double bundle ACL reconstruction: impact of knee flexion angle and portal location on the femoral PL bundle tunnel. Arch Orthop Trauma Surg 128:509–513
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, Y.S., Nam, S.W., Sim, J.A. et al. Comparison of anatomic ACL reconstruction between selective bundle reconstruction and double-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc 22, 2803–2810 (2014). https://doi.org/10.1007/s00167-013-2684-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2684-8