Abstract
Purpose
To prospectively assess the anterior tibial translation and rotational kinematics of the knee joint as well as the clinical outcome after single-bundle (SB) and double-bundle (DB) anterior cruciate ligament (ACL) reconstruction.
Methods
Forty-two patients randomly underwent single-bundle (Group SB, n = 21) or double-bundle (Group DB, n = 21) ACL reconstruction using hamstring tendon autografts. Anterior tibial translation and rotatory laxity were measured prior to and after fixation of the graft during reconstruction under the guidance of a navigation system. Clinical outcome measurements included the evaluation of the joint stability and functional status.
Results
Anterior tibial translation and rotatory laxity were improved significantly at all degrees of knee flexion in both groups. The postoperative total rotation (sum of internal and external rotation) at 30° and 60° (26.6° vs. 24.0°; 28.7° vs. 25.1°) as well as postoperative change in external rotation at 60° (−1.4° vs. −4.6°), and a change in total rotation at 30° and 60° (−7.0° vs. −11.5°; −6.1° vs. −8.9°) differed between the two groups, with better stability in the DB group. At 2 years follow-up, IKDC subjective satisfaction score was significantly different between two groups (70.9 vs. 79.6), while manual and instrumented laxity, pivot shift tests, modified Lysholm score, Tegner activity score, thigh muscle strengths were not different. Correlation analysis showed little correlations between anterior laxity tests at follow-up, and the kinematic variables measured by navigation during surgery while pivot shift test, IKDC subjective satisfaction score, modified Lysholm score, and Tegner activity score were mainly correlated with navigation-measured rotations in both groups.
Conclusions
The kinematic tests in this study found evidence suggesting that the DB ACL reconstruction improved rotatory laxity better than the SB ACL reconstruction at 30° and 60° of flexion, but there was no difference in functional outcome at 2 years follow-up between SB and DB groups.
Level of evidence
Prospective comparative study, Level II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although the conventional anterior cruciate ligament (ACL) reconstruction technique has met with some success in restoring overall joint stability, reports in the literature still reveal instabilities and subsequent patient dissatisfaction [2, 9, 33]. In order to overcome these limitations of the single-bundle (SB) ACL reconstruction technique, the double-bundle (DB) reconstruction technique was proposed as a method to anatomically replicate both the anteromedial (AM) and the posterolateral (PL) bundle [29]. However, there is still not enough evidence as to whether the DB ACL reconstruction is worth the extra effort required to reconstruct the PL bundle in addition to the AM bundle in ACL reconstruction.
The reason for the continued controversy regarding the proper number of bundles and the orientation of tunnels and grafts is largely attributable to the general incomparability of studies owing to inter-operator variability of tunnel measurements and placements as well as to the lack of accuracy and objectivity of kinematic measurements [4, 5, 7, 8, 24, 28, 30]. Cadaver studies also have some inherent limitations in reproducing all relevant muscle forces and weight-bearing conditions.
A computer-assisted navigation system for use in ACL reconstruction is considered to provide the precision necessary for objective and quantitative measurements of knee kinematics in three-dimensional planes pre- and postoperatively [10, 31]. Using this navigation system, inter- and intra-operator differences in the orientation of tunnel placement is reduced and three-dimensional kinematic measurements, including rotational properties, have been conducted with improved accuracy and objectivity [24, 39].
The objective of this study was to assess anterior tibial translation and rotatory laxity in ACL-reconstructed knees with SB and DB techniques. The principal objective of the study was to evaluate kinematic variables accurately using a navigation system, and the secondary objective was to measure knee-specific outcomes and functions at follow-up. Our hypothesis was that the DB ACL reconstruction better limits rotational laxity than SB ACL reconstruction, thereby improving knee function.
Materials and methods
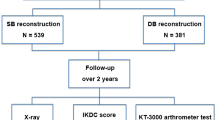
Subjects were recruited from patients with ACL-deficient knees operated on by a single surgeon from November 2007 through January 2009 (Fig. 1). After three more patients were excluded due to subtotal meniscectomy, forty-two patients who fulfilled the inclusion criteria and provided informed consent were randomized and underwent ACL reconstruction procedures via either SB (Group SB, n = 21) or DB (Group DB, n = 21) using autologous gracilis and semitendinosus tendon grafts. The patients with fractures and those with multiple ligamentous injuries including posterior cruciate ligament and posterolateral corner were excluded (Table 1). The college and hospital institutional review board approved the protocols of this study. A sample size analysis suggested the original size of the groups was approximated to 17 for each group to detect the kinematic difference by navigation with the power 0.8 and type I error probability of 0.05.
The mean age was 29.4 (range 17–56) in the SB group and 31.2 (range 19–52) in the DB group. No differences were noted in age, gender, weight, height, and body mass indices between the two groups (Table 2). The ACL ruptures and other combined injuries were initially confirmed by arthroscopic examination, and arthroscopic meniscectomy and meniscal repair were carried out concurrently at the time of ACL reconstruction. Two knees were combined with medial collateral injuries that healed prior to subsequent surgeries, and meniscal resection was less than 50% in all knees. The remnants of the torn ACL were partially removed in order to identify the anatomic footprints of the ACL attachments on the femur and the tibia through the anterolateral and anteromedial portals.
Single-bundle ACL reconstruction with hamstring autograft
The semitendinosus and gracilis tendons were harvested from the ipsilateral knee joint and folded into a 4-stranded graft. The tibial tunnel was drilled to the center of the ACL footprint through the anteromedial surface of the tibia, and the femoral tunnel was drilled into the lateral femoral condyle at the anatomic footprint of ACL with the knee flexed to 120° using a 4.5-mm cannulated reamer (Smith & Nephew Endoscopy). After femoral and tibial tunnels were created with a cannulated reamer matching the graft diameter, the prepared quadrupled hamstring tendon graft was passed and secured with a 15 mm EndoButton CL (Smith & Nephew Endoscopy). The tibial side of the quadrupled graft was fixed with a 25-mm bioabsorbable interference screw (Matryx™ screw; ConMed Linvatec, Largo, FL) with the same diameter matching the tibial tunnel, and it was augmented by tying the sutures over the biocortical screw.
Double-bundle ACL reconstruction
The semitendinosus and gracilis tendons were harvested via the technique described above. However, the harvested tendons were fashioned into two multi-stranded grafts, rather than into a single quadrupled graft. The gracilis tendon and the proximal half of the semitendinosus tendon were each looped and quadrupled to replicate the AM bundle, and the thicker distal half of the semitendinosus tendon was looped (doubled) to replicate the PL bundle. The diameter of the grafts was 5 to 6 mm (M: 5.3 ± 0.6 mm; F: 5.0 ± 0.4 mm) for the PL bundle and 6 to 8 mm (M: 7.3 ± 0.8 mm; F: 6.6 ± 1.1 mm) for the AM bundle. Each tendon graft bundle was pretensioned prior to implantation in the same manner. The tibial and femoral tunnels were prepared generally in accordance with the previously described techniques with modification [14, 25, 42]. Briefly, the tip of the tibial guide for the PL bundle was located on the posterior half of ACL footprint, and the probe for the AM bundle was placed anterior to the posterior tunnel, leaving a 2-mm bone bridge. The femoral tunnels were made at femoral footprints under lateral intercondylar ridge with an inside-out technique transtibially if possible or from an AM portal with a graft-matched diameter. The grafts replicating each bundle were passed and fixed to the femur using the EndoButton-CL-technique and secured to the tibia using bioabsorbable interference screws augmented by tying onto a post screw. The AM bundle was fixed at 10 degrees of flexion first and then the PL bundle at full extension.
Intraoperative measurement with navigation system
The navigation system (OrthoPilot, B.Braun-Aesculap, Tuttlingen, Germany) was used to evaluate the kinematics of the knee in the three-dimensional plane including the anteroposterior translation of the tibia and the internal rotation (IR) and external rotation (ER) of the tibia [16]. To begin the navigation process, after fixing the transmitters firmly to the femur and tibia with 2 Steinman pins of 2.0-mm diameter, we registered extra-articular and intra-articular landmarks with straight and hooked pointers: the tibial tuberosity, the medial and lateral points of the tibial plateau, femoral epicondyles, the anterior edge of the PCL on the tibial plateau, the anterior horn of the lateral meniscus, the spine of the medial intercondylar tubercle, the medial notch wall, the anterior notch outlet, the lateral notch wall, the ACL insertion area on the femur, the 12-o’clock over-the-top position, and the lateral over-the-top position (Fig. 2). The navigation was used to estimate the manual maximum anterior tibial translation, as well as IR and ER of the tibia at 0°, 30°, 60°, and 90° of knee flexion (Fig. 3). All measurements were initially conducted immediately after registration and finally after ACL reconstruction. The anterior displacement values were recorded by the system and expressed in millimeters; the IR and ER values of the tibia were recorded by the system and expressed in degrees. Total rotation was calculated as the sum of internal and external rotation. The accuracy of the navigation was estimated at 0 to 1 mm and 0°–1° [19, 20, 23]. The navigation system was used to collect the motion measurements with 6 degrees of freedom per bone and to provide real-time calculation of translation and rotation at all degrees of knee flexion while the surgeon manipulated the joint. All manual stress tests were conducted by two surgeons who made every effort to apply similar loading to the knee each time, and the averaged value was used for further analysis to minimize inter-operator variability.
Postoperative rehabilitation
For all patients, continuous passive motion was started from 0° to 45° of motion the next postoperative day and continued for 1–2 days while patients were hospitalized. Full extension was achieved during the first postoperative week, and full flexion was achieved by 6 weeks. Kinetic exercise and weight bearing were progressed as tolerated, and full activity such as strenuous sport was permitted 9 months postoperatively after confirming recovery of quadriceps strength.
Evaluation of clinical results
Clinical results were evaluated with regard to the joint laxity and functional status in the outpatient clinic preoperatively and at 24 months postoperatively. Assessments were performed by two independent examiners. To evaluate the laxity of the reconstructed knees, the side-to-side differences in translation were measured via manual maximum testing with a KT-1000 arthrometer (MEDmetric Corp, San Diego, California), and the knees were graded as 0, 1, 2, and 3 by the anterior drawer test, Lachman test and also by the pivot shift test manually. Modified Lysholm, IKDC, and Tegner activity scores were documented, and quadriceps muscle strength was measured by Cybex II dynamometer.
Statistical analysis
Statistical analyses were conducted via Fisher’s exact test and Mann–Whitney test with SPSS 17.0 K software (SPSS Inc, Chicago, Illinois) to compare the demographic variables, kinematic variables of translation and rotation measured by the navigation system, manual laxity test, and functional scores between SB and DB groups. The correlations were investigated between the clinical outcome variables at 2-year follow-up and kinematic variables measured by navigation during surgery. The minimum level of significance was set at P < 0.05.
Results
Anterior tibial translation and rotatory laxity were reduced in all patients after ACL reconstruction, and the changes were significant in all evaluations.
The postoperative reduction in anterior tibial translation and rotatory laxity did not differ for the most part between the SB and DB groups. However, DB group showed significantly smaller total rotation (sum of internal and external rotation) at 30° and 60° (P < 0.05) postoperatively. In addition, DB group showed greater postoperative change in external rotation at 60° (P < 0.05), and postoperative change in total rotation at 30° and 60° (P < 0.05; Table 3).
Eighteen patients in the SB group (85.7%) and 19 patients (90.5%) in the DB group were followed-up at 2 years after surgery, and clinical outcomes in anterior laxity, pivot shift, functional scores, quadriceps muscle strength did not differ between the SB and DB groups except IKDC subjective satisfaction score (P < 0.05; Table 4).
Correlation analysis showed little correlations between anterior laxity tests at follow-up and the kinematic variables measured by navigation during surgery. However, the pivot shift test, IKDC subjective satisfaction score, modified Lysholm score, and Tegner activity score were mainly correlated with navigation-measured rotations in SB group as well as DB group (P < 0.05; Table 5).
Discussion
This study demonstrated superiority in rotatory laxity, particularly at 30 and 60 degrees of knee flexion, in the DB ACL reconstruction group relative to the SB group based on the kinematic data acquired from a navigation system. These findings are consistent with data of other cadaveric biomechanical studies as well as those of other in vivo kinematic study using the navigation system, which revealed improved rotatory laxity with the additional PL bundle to the AM bundle [8, 26, 27, 32, 35, 41, 43].
Although this study reports evidence suggesting that the DB ACL reconstruction is superior to the SB ACL reconstruction in terms of kinematic properties, some other previous studies have reported data contradicting our findings, wherein the addition of a PL bundle did not appear to improve rotatory laxity [11]. In the study of Ferretti et al. in which ten knee joints were evaluated, no difference was detected between the AM bundle only and the AM + PL bundle in ACL reconstruction using the same navigation system. The bundle reconstruction was done serially, and the resultant data were compared in the same knee joint, whereas two independent groups were compared in our study. In another study with the same navigation system, the range of difference was only between 15° and 30°, although rotational superiority was reported [16].
A limitation of this study was that time-zero measurements only were carried out. As we still do not have sufficient quantitative data regarding normal knees to establish a reference regarding the degrees of motion required for specific sports activities, we do not yet know precisely how much the knee must be stabilized to achieve optimal function. Even though laxity has proven to be the principal issue more frequently than overtightening after ACL reconstruction, precise tuning of in situ forces in the reconstructed ACL and the resultant laxity are mandatory for normal physiological reconstruction.
The results of a host of comparative studies with clinical outcomes are quite contradictory, although these studies are limited principally to short-term follow-up [1, 3, 13, 17, 21, 35, 36, 40]. In this study, we also detected no significant differences between the groups in regard to clinical outcomes except IKDC subjective satisfaction, despite the superior biomechanical properties observed in the navigation process. This may be because the sensitivities of the outcome measurement tools are different from those of the biomechanical study. Although it is less likely, relatively low activity level of the subjects involved in this study, most of whom were recreational players, could be another reason why there was no difference between groups. Unfortunately, there is no sufficient evidence for the correlations between the activity level and the functional difference between groups because most previous comparison studies did not specify the level of activities of subjects. Another reason for no distinction may be the low power to observe the effect of clinical outcome variables because of the small number of subjects, which was partly limited by potential invasiveness of the navigation system and sufficient to detect the difference in kinematic variables only. Further study with greater number of the patients is warranted.
It is interesting to note that the rotations were largely correlated with pivot shift test results as well as functional outcome variables such as IKDC subjective satisfaction, modified Lysholm and Tegner activity scores, while anterior tibial translations were not. This finding is in agreement with the results of other studies in that rotational measurements such as pivot shift test were more predictive of functional recovery and subjective satisfaction [18, 37]. The results in this study can be one of the evidences supporting that rotation influences on the functional outcome more than the anterior laxity does both in SB and in DB groups. However, it is still questionable whether the correlation with the rotation is more remarkable or the functions are superior in DB group than in SB group. Recently several authors reported conflicting results about the functional outcomes comparison after SB and DB ACL reconstructions, but the final conclusion remains unclear [12, 22].
The navigation system used in ACL reconstruction surgery has not only been shown to improve the accuracy of the procedure, but also enables researchers to collect objective and quantitative data in a more valid and reliable fashion [15, 23, 31, 39]. Previous studies regarding the relationship of navigation system to conventional clinical examinations, including the Lachman test and the pivot shift test, have already corroborated its validity as a kinematic evaluation tool [6, 24, 34, 38]. However, the current navigation system is based on unmeasured manual stress, which is one of the principal limitations of this study. The manually exerted stress could not be precisely calibrated. Two individuals attempted to control the magnitude of manual stress in the measurement procedures, and the mean values were used for comparison in order to minimize the bias in the kinematic evaluations.
In summary, this study uncovered evidence suggesting that DB ACL reconstructions result in better in vivo stability than SB ACL reconstruction; the hypothesis that the PL bundle would improve rotatory laxity was confirmed. However, we failed to observe significant differences in clinical outcomes between groups except IKDC subjective satisfaction score, although we noticed the rotation was more important than anterior tibial translation equally in SB and DB groups. The hypothesis that improved rotatory laxity by the addition of the PL bundle would improve functional outcomes was not confirmed.
The results of this study do not currently prove the hypothesis that more bundles result in better outcomes in ACL reconstruction. However, the findings of this study warrant further studies into more optimized ACL reconstruction techniques using multiple graft bundles. After establishing the reference kinematic data of the normal physiologic range of motion in various activities, we should be able to come to some more definitive conclusions regarding the laxity of the patient’s knee joint on navigation-based kinematic analyses; this will allow us to more effectively customize ACL reconstructions for individual patients. Additionally, further observation of clinical outcomes and graft evaluation are mandatory to assess whether the navigational measurements are pertinent to the clinical consequences or, in other words, whether the intraoperative kinematic data would predict clinical outcome.
Conclusions
The kinematic tests in this study found evidence suggesting that the DB ACL reconstruction improved rotatory laxity better than the SB ACL reconstruction at 30° and 60° of flexion, but there was no difference in functional outcome at 2 years follow-up between SB and DB groups.
References
Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y (2004) Reconstruction of the anterior cruciate ligament. Single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br 86:515–520
Aglietti P, Buzzi R, D’Andria S, Zaccherotti G (1992) Arthroscopic anterior cruciate ligament reconstruction with patellar tendon. Arthroscopy 8:510–516
Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N (2010) Comparison between single- and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med 38:25–34
Bach JM, Hull ML, Patterson HA (1997) Direct measurement of strain in the posterolateral bundle of the anterior cruciate ligament. J Biomech 30:281–283
Bedi A, Musahl V, Lane C, Citak M, Warren RF, Pearle AD (2010) Lateral compartment translation predicts the grade of pivot shift: a cadaveric and clinical analysis. Knee Surg Sports Traumatol Arthrosc 18:1269–1276
Bignozzi S, Zaffagnini S, Lopomo N, Fu FH, Irrgang JJ, Marcacci M (2010) Clinical relevance of static and dynamic tests after anatomical double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 18:37–42
Bull AM, Andersen HN, Basso O, Targett J, Amis AA (1999) Incidence and mechanism of the pivot shift. An in vitro study. Clin Orthop Relat Res 363:219–231
Bull AM, Earnshaw PH, Katchburian MV, Hassan AN, Amis AA (2002) Intraoperative measurement of knee kinematics in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 84:1075–1081
Chouliaras V, Ristanis S, Moraiti C, Stergiou N, Georgoulis AD (2007) Effectiveness of reconstruction of the anterior cruciate ligament with quadrupled hamstrings and bone-patellar tendon-bone autografts: an in vivo study comparing tibial internal-external rotation. Am J Sports Med 35:189–196
Colombet P, Robinson J, Christel P, Franceschi J-P, Djian P (2007) Using navigation to measure rotation kinematics during ACL reconstruction. Clin Orthop Relat Res 454:59–65
Ferretti A, Monaco E, Labianca L, de Carli A, Maestri B, Conteduca F (2009) Double-bundle anterior cruciate ligament reconstruction: a comprehensive kinematic study using navigation. Am J Sports Med 37:1548–1553
Gobbi A, Mahajan V, Karnatzikos G, Nakamura N (2011) Single- versus double-bundle ACL reconstruction: is there any difference in stability and function at 3-year followup? Clin Orthop Relat Res. Epub doi:10.1007/s11999-011-1940-9
Hamada M, Shino K, Horibe S, Mitsuoka T, Miyama T, Shiozaki Y, Mae T (2001) Single- versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with endobutton femoral fixation: a prospective study. Arthroscopy 17:801–807
Harner CD, Honkamp NJ, Ranawat AS (2008) Anteromedial portal technique for creating the anterior cruciate ligament femoral tunnel. Arthroscopy 24:113–115
Hart R, Krejzla J, Sváb P, Kocis J, Stipcák V (2008) Outcomes after conventional versus computer-navigated anterior cruciate ligament reconstruction. Arthroscopy 24:569–578
Ishibashi Y, Tsuda E, Tazawa K, Sato H, Toh S (2005) Intraoperative evaluation of the anatomical double-bundle anterior cruciate ligament reconstruction with the orthopilot navigation system. Orthopedics 28:s1277–s1282
Jarvela T (2007) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 15:500–507
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32:629–634
Koh J (2005) Computer-assisted navigation and anterior cruciate ligament reconstruction: accuracy and outcomes. Orthopedics 28:s1283–s1287
Koh J, Koo SS, Leonard J, Kodali P (2006) Anterior cruciate ligament (ACL) tunnel placement: a radiographic comparison between navigated versus manual ACL reconstruction. Orthopedics 29:S122–S124
Lewis PB, Parameswaran AD, Rue JP, Bach BRJ (2008) Systematic review of single-bundle anterior cruciate ligament reconstruction outcomes: a baseline assessment for consideration of double-bundle techniques. Am J Sports Med 36:2028–2036
Longo UG, King JB, Denaro V, Maffulli N (2008) Double-bundle arthroscopic reconstruction of the anterior cruciate ligament: does the evidence add up? J Bone Joint Surg Br 90:995–999
Lopomo N, Bignozzi S, Martelli S, Zaffagnini S, Iacono F, Visani A, Marcacci M (2009) Reliability of a navigation system for intra-operative evaluation of antero-posterior knee joint laxity. Comput Biol Med 39:280–285
Lopomo N, Zaffagnini S, Bignozzi S, Visani A, Marcacci M (2010) Pivot-shift test: analysis and quantification of knee laxity parameters using a navigation system. J Orthop Res 28:164–169
Lubowitz JH (2009) Anteromedial portal technique for the anterior cruciate ligament femoral socket: pitfalls and solutions. Arthroscopy 25:95–101
Mae T, Shino K, Miyama T, Shinjo H, Yoshikawa H, Fujie H (2001) Single- versus two-femoral socket anterior cruciate ligament reconstruction technique: biomechanical analysis using a robotic simulator. Arthroscopy 17:708–716
Markolf KL, Park S, Jackson SR, McAllister DR (2009) Anterior-posterior and rotatory stability of single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg Am 91:107–118
Matsumoto H (1990) Mechanism of the pivot shift. J Bone Joint Surg Br 72:816–821
Muneta T, Sekiya I, Yagishita K, Ogiuchi T, Yamamoto H, Shinomiya K (1999) Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy 15:618–624
Noyes FR, Grood ES, Cummings JF, Wroble RR (1991) An analysis of the pivot shift phenomenon. The knee motions and subluxations induced by different examiners. Am J Sports Med 19:148–155
Plaweski S, Cazal J, Rosell P, Merloz P (2006) Anterior cruciate ligament reconstruction using navigation: a comparative study on 60 patients. Am J Sports Med 34:542–552
Radford WJ, Amis AA (1990) Biomechanics of a double prosthetic ligament in the anterior cruciate deficient knee. J Bone Joint Surg Br 72:1038–1043
Ristanis S, Stergiou N, Patras K, Tsepis E, Moraiti C, Georgoulis AD (2006) Follow-up evaluation 2 years after ACL reconstruction with bone-patellar tendon-bone graft shows that excessive tibial rotation persists. Clin J Sport Med 16:111–116
Robinson J, Carrat L, Granchi C, Colombet P (2007) Influence of anterior cruciate ligament bundles on knee kinematics: clinical assessment using computer-assisted navigation. Am J Sports Med 35:2006–2013
Seon JK, Park SJ, Lee KB, Yoon TR, Kozanek M, Song EK (2009) Range of motion in total knee arthroplasty: a prospective comparison of high-flexion and standard cruciate-retaining designs. J Bone Joint Surg Am 91:672–679
Siebold R, Dehler C, Ellert T (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:137–145
Snyder-Mackler L, Fitzgerald GK, Bartolozzi AR, Ciccotti MG (1997) The relationship between passive joint laxity and functional outcome after anterior cruciate ligament injury. Am J Sports Med 25:191–195
Song EK, Oh LS, Gill TJ, Gadikota HR, Seon JK (2009) Prospective comparative study of anterior cruciate ligament reconstruction using the double-bundle and single-bundle techniques. Am J Sports Med 37:1705–1711
Tsuda E, Ishibashi Y, Fukuda A, Tsukada H, Toh S (2007) Validation of computer-assisted double-bundle anterior cruciate ligament reconstruction. Orthopedics 30:S136–S140
Yagi M, Kuroda R, Nagamune K, Kurosaka M (2007) Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res 454:100–107
Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL-Y (2002) Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 30:660–666
Yasuda K, Kondo E, Ichiyama H, Kitamura N, Tanabe Y, Tohyama H, Minami A (2004) Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 20:1015–1025
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227
Acknowledgments
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea. (A100451).
Author information
Authors and Affiliations
Corresponding author
Additional information
Sahnghoon Lee and Hyoungmin Kim have contributed equally to the preparation of this article.
Rights and permissions
About this article
Cite this article
Lee, S., Kim, H., Jang, J. et al. Comparison of anterior and rotatory laxity using navigation between single- and double-bundle ACL reconstruction: prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 20, 752–761 (2012). https://doi.org/10.1007/s00167-012-1880-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-1880-2