Abstract
Purpose
The purpose of this study was to evaluate trends in surgical treatment of articular cartilage defects of the knee in the United States.
Methods
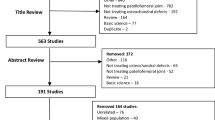
The current procedural terminology (CPT) billing codes of patients undergoing articular cartilage procedures of the knee were searched using the PearlDiver Patient Record Database, a national database of insurance billing records. The CPT codes for chondroplasty, microfracture, osteochondral autograft, osteochondral allograft, and autologous chondrocyte implantation (ACI) were searched.
Results
A total of 163,448 articular cartilage procedures of the knee were identified over a 6-year period. Microfracture and chondroplasty accounted for over 98 % of cases. There was no significant change in the incidence of cartilage procedures noted from 2004 (1.27 cases per 10,000 patients) to 2009 (1.53 cases per 10,000 patients) (p = 0.06). All procedures were performed more commonly in males (p < 0.001). This gender difference was smallest in patients undergoing chondroplasty (51 % males and 49 % females) and greatest for open osteochondral allograft (61 % males and 39 % females). Chondroplasty and microfracture were most commonly performed in patients aged 40–59, while all other procedures were performed most frequently in patients <40 years old (p < 0.001).
Conclusions
Articular cartilage lesions of the knee are most commonly treated with microfracture or chondroplasty in the United States. Chondroplasty and microfracture were most often performed in middle-aged patients, whereas osteochondral autograft, allograft, and ACI were performed in younger patients, and more frequently in males.
Level of evidence
Cross-sectional study, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Articular cartilage defects of the knee present a challenging problem for orthopaedic surgeons, and the treatment of these defects represents an active area of orthopaedic research. Full-thickness chondral defects are commonly found during arthroscopy in the general population and seen at a higher frequency in athletes. Curl et al. [7] reported chondral lesions in 63 % of patients in a retrospective review of over 30,000 arthroscopies in patients of all ages.
During the past two decades, several cartilage reparative and restorative procedures have been developed. Current options in the United States include debridement, subchondral marrow stimulation, reconstruction using allograft or autograft, and regeneration via grafting autologous chondrocyte cells [23]. Second-generation systems are now available outside of the United States that employ absorbable scaffolds to support autologous chondrocytes prior to implantation, and systems employing growth factors and stem cell therapy are on the horizon [17, 21].
The indications for procedures addressing articular cartilage defects are evolving as more data become available on clinical outcomes. Current treatment algorithms for cartilage restoration procedures are based primarily on the size of the defect, functional demands of the patient, and age [1, 9]. At present, there are limited clinical studies demonstrating superiority of any one procedure addressing these lesions [5, 13]. Although there are a number of different cartilage restoration procedures being performed in the United States, there are no data describing the frequency with which they are being used nor the demographics of the patients undergoing these procedures. The purpose of this study was to use a cross-sectional analysis to evaluate trends in surgical treatment of articular cartilage defects of the knee in the United States and to test the hypothesis that the performance of these procedures is increasing and utilized primarily in a younger patient population.
Materials and methods
The current procedural terminology (CPT) billing codes of patients undergoing articular cartilage procedures of the knee were searched using the PearlDiver Patient Record Database (PearlDiver Technologies, Inc., Fort Wayne, IN). This database is a national insurance database with the largest contribution being from UnitedHealth Group. From the years 2004 to 2009, over 216 million orthopaedic patient records exist in the database from over 11 million patients with an orthopaedic International Classification of Disease, Ninth Revision (ICD-9) diagnosis code or CPT code [8].
Procedures and the corresponding CPT codes searched included chondroplasty, microfracture, osteochondral autograft, osteochondral allograft, and autologous chondrocyte implantation (ACI). The complete definitions of these codes are listed in Table 1. Each of these CPT codes was then searched in combination with high tibial osteotomy. The type of procedure, date, gender, and region of the country (West, Midwest, Northeast, and South) was identified for each patient.
Statistical analysis
Chi-square analysis was used to determine the statistical significance with regard to gender, age, and region. Linear regression was performed to test the significance of trends over time. Variations in the total number of orthopaedic patients in the database for a given time, gender, age, or region were accounted for when performing statistical analysis [24].
Results
A total of 163,448 articular cartilage procedures of the knee were identified from the years 2004 to 2009. The most commonly identified codes were observed when chondroplasty (125,245) and microfracture (36,095) were searched, together accounting for over 98 % of all cases. The fewest number of codes were identified when open osteochondral autograft was searched, yielding 107 patients. Arthroscopic osteochondral autograft (696), arthroscopic osteochondral allograft (633), open osteochondral allograft (310), and ACI (362) accounted for the remaining identified procedures.
Temporal trends
There was an increase in the total number of procedures from 19,772 in 2004 to 29,432 in 2009. However, linear regression analysis revealed that this difference did not reach statistical significance in the incidence of procedures identified over the 6-year study period from 2004 to 2009 when normalized to the number of patients in the database during those years (p = 0.06) (Table 2). Articular cartilage procedures were performed in 33–40 % of all patients undergoing knee arthroscopy depending on the year (Table 2), with the majority of these procedures being chondroplasties.
Age
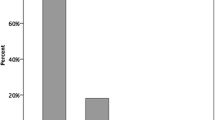
Patients were stratified into three groups representing a young (<40 years old), middle-aged (40–59 years), and older population (>60 years) (Fig. 1). Using this stratification, chondroplasty and microfracture were both observed at a significantly higher rate in patients aged 40–59 years (p < 0.001), accounting for 64 and 61 % of patients undergoing these procedures, respectively. Osteochondral allograft (open and arthroscopic), osteochondral autograft (open and arthroscopic), and ACI were all preformed at a significantly higher rate in patients aged <40 years (p < 0.001).
Gender
All procedures combined, and each individual procedure, was performed more commonly in males compared to females. This difference was smallest with chondroplasty (52 % males and 48 % females) and microfracture (54 % males and 46 % females). The magnitude of this difference was much higher for all other procedures and greatest in patients undergoing arthroscopic osteochondral allograft (61 % males and 39 % females). All differences were statistically significant when compared to the gender breakdown of those patients searched in the database (p < 0.05).
Regional distribution
The database is most well represented by the South (45 % of all patients), whereas the Northeast has the smallest representation (13 % of patients). With all procedures combined, the Northeast accounted for a significantly smaller proportion of patients (9.8 %) than its representation in the database, while all other regions accounted for a slightly larger proportion of patients (p < 0.001). In all procedures except ACI and open osteochondral autograft (n.s.), statistically significant regional differences were observed (p < 0.05) (Fig. 2). Arthroscopic osteochondral allograft was the only procedure in which more patients in the Northeast were observed than expected (p < 0.001).
Articular cartilage procedures combined with high tibial osteotomy
High tibial osteotomy (HTO) was searched in combination with each articular cartilage procedure to evaluate the incidence of HTO with each type of intervention. High tibial osteotomy was performed at a significantly higher rate in conjunction with ACI (6.3 % of cases) and with open osteochondral allograft (4.5 % of cases) compared to all other procedures (p < 0.001) (Fig. 3).
Discussion
The most important finding of the present study was that chondroplasty and microfracture were performed commonly in middle-aged patients. Articular cartilage defects of the knee are common, and the development of surgical interventions to decrease pain and improve function secondary to these lesions represents an evolving area in orthopaedic surgery. Currently, minimal data exist on the utilization of these procedures in the United States or on the demographics of patients undergoing these procedures. We are unaware of similar studies evaluating changes in the incidence of these procedures with time.
Chondroplasty and microfracture were observed most often in this database search, yielding 125,245 and 36,095 patients, respectively. Debridement or microfracture are often first-line treatments, particularly for small chondral defects, given the relative ease of these procedures, low cost, and practicality of performing each with other arthroscopic procedures such as meniscus repair and ligament reconstruction. Chondroplasty, despite its inability to restore the articular surface, has been demonstrated to have benefit in addressing chondral defects in the knee [12]. Additionally, patients have improved their clinical score following treatment with microfracture in several studies [6, 10, 16, 19, 22].
In this study, chondroplasty and microfracture were more commonly performed in patients aged 40–59 years, while all other procedures were performed more commonly in those <40 years of age. Age is an important and controversial consideration in cartilage repairing and restoring procedures in the knee and has been implicated in the degree of success achieved with these procedures [15]. In a survey of 242 orthopaedic surgeons in Europe, 33.1 % have an age limit for invasive cartilage repair, with 22.7 % treating patients only under the age of 60 and 32.2 % treating patients exclusively <50 years old [20]. Accordingly, the utility of these procedures in older patients, who are more likely to have diffuse cartilage degeneration, continues to be a matter of debate. High-level-of-evidence studies on cartilage surgery are from randomized controlled trials in patients under 50 years with focal defects without generalized osteoarthritis. Although debriding fragments of articular cartilage or chondral flaps may not be harmful, they may offer no benefit compared to nonoperative management [14]. Moreover, more aggressive methods such as microfracture can lead to an increase in the thickness of the subchondral bone plate and thus may predispose the joint to further cartilage degeneration [2]. The cost of rehabilitation, sick leave, crutches, and continuous passive motion (CPM) must also be considered.
In this study, a greater incidence of procedures was found in male compared to female patients. These results are consistent with prior studies reporting on articular cartilage procedures of the knee. However, in the Norwegian ACL registry, no gender differences in the prevalence of articular cartilage lesions were observed [11]. Interestingly, we found that gender differences were much smaller in patients undergoing microfracture and chondroplasty compared to chondrocyte implantation, autologous transfer, or osteochondral allograft. The results of the current study suggest that males are more frequently undergoing these procedures.
Although considerable regional variation existed among the various procedures analysed in this study, the Northeast consistently had a lower incidence of cartilage repairing and restoring procedures when compared to the West, Midwest, and Southern regions of the United States. The reason for this difference is unclear. In an analysis of drivers of surgery rates for the degenerative hip, knee, and spine, Bederman et al. [4] identified age, nonminority, insurance coverage, and surgeon enthusiasm as factors that increased surgical rates. Specialty training in sports medicine has been shown to affect the rates of meniscal repair in combination with anterior cruciate ligament (ACL) reconstruction [18].
It is generally agreed that mechanical alignment must be restored prior to performing a cartilage repairing or restoring procedure in the knee. In particular, high tibial osteotomy is necessary to correct varus deformity when addressing chondral defects of the medial compartment [1]. High tibial osteotomy was most commonly performed with ACI and osteochondral allograft. Few reports exist in the literature describing the use of high tibial osteotomy in conjunction with these procedures. In a study of femoral osteochondral allograft for the treatment of post-traumatic knee defects, 68 % of patients underwent a concomitant realignment procedure and were found to have similar outcomes to those who underwent osteochondral allograft alone [3].
This study has a number of limitations. Although the study included a search of over 11 million patients with an orthopaedic ICD-9 or CPT code across all four regions of the United States, this does not necessarily provide a representative sample of the US population as a whole. Also, there is no patient-specific information (i.e. size of articular cartilage defect), operative report details, post-operative rehabilitation information, or outcome data available. Specifically, missing procedure details adds complexity in interpreting the chondroplasty data, as the term chondroplasty can be used to describe procedures ranging from debridement of loose cartilage flaps to those involving subchondral stimulation. However, based on the definitions of CPT codes for chondroplasty and microfracture, the code for microfracture indicates a more aggressive procedure more likely to involve stimulation of subchondral bone. Also, information about regional differences in confounding factors such as BMI and smoking habits is not available, and as with any database search using CPT codes, the results are subject to error introduced by improper coding.
Lastly, this study addresses a relatively broad topic including a number of different procedures. Future studies may be aimed at further subgroup analysis within each procedure and cross-referencing with other CPT codes and ICD-9 codes, such as those for meniscal and ligament injury, to further delineate the characteristics of surgeries addressing articular cartilage defects of the knee.
Conclusions
Articular cartilage lesions of the knee are most commonly treated with microfracture or chondroplasty in the United States, and no significant increase in utilization of these procedures was observed during the years evaluated. Chondroplasty and microfracture were most often performed in middle-aged patients, whereas osteochondral autograft, allograft, and autologous chondrocyte implantation (ACI) were performed in younger patients, and more frequently in males. This study provides information on current practice patterns in the treatment of articular cartilage defects of the knee as the orthopaedic community attempts to elucidate the most effective procedures to treat this pathology and the demographics of patients most likely to respond to these treatments.
References
Alford JW, Cole BJ (2005) Cartilage restoration, part 2: techniques, outcomes, and future directions. Am J Sports Med 33:443–460
Årøen A, Heir S, Løken S, Engebretsen L, Reinholt FP (2006) Healing of articular cartilage defects. An experimental study of vascular and minimal vascular microenvironment. J Orthop Res 24:1069–1077
Aubin PP, Cheah HK, Davis AM, Gross AE (2001) Long-term followup of fresh femoral osteochondral allografts for posttraumatic knee defects. Clin Orthop Relat Res 391:S318–S327
Bederman SS, Rosen CD, Bhatia NN, Kiester PD, Gupta R (2012) Drivers of surgery for the degenerative hip, knee, and spine: a systematic review. Clin Orthop Relat Res 470:1090–1105
Bentley G, Biant LC, Carrington RW, Akmal M, Goldberg A, Williams AM, Skinner JA, Pringle J (2003) A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br 85:223–230
Cerynik DL, Lewullis GE, Joves BC, Palmer MP, Tom JA (2009) Outcomes of microfracture in professional basketball players. Knee Surg Sports Traumatol Arthrosc 17:1135–1139
Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG (1997) Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy 13:456–460
Daffner SD, Beimesch CF, Wang JC (2010) Geographic and demographic variability of cost and surgical treatment of idiopathic scoliosis. Spine 35:1165–1169
Farr J, Cole B, Dhawan A, Kercher J, Sherman S (2011) Clinical cartilage restoration: evolution and overview. Clin Orthop Relat Res 469:2696–2705
Gobbi A, Nunag P, Malinowski K (2005) Treatment of full thickness chondral lesions of the knee with microfracture in a group of athletes. Knee Surg Sports Traumatol Arthrosc 13:213–221
Granan LP, Bahr R, Lie SA, Engebretsen L (2009) Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian National Knee Ligament Registry. Am J Sports Med 37:955–961
Hubbard MJ (1996) Articular debridement versus washout for degeneration of the medial femoral condyle. A five-year study. J Bone Joint Surg Br 78:217–219
Jakobsen RB, Engebretsen L, Slauterbeck JR (2005) An analysis of the quality of cartilage repair studies. J Bone Joint Surg Am 87:2232–2239
Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, Feagan BG, Donner A, Griffin SH, D’Ascanio LM, Pope JE, Fowler PJ (2008) A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med 359:1097–1107
Kreuz PC, Erggelet C, Steinwachs MR, Krause SJ, Lahm A, Niemeyer P, Ghanem N, Uhl M, Südkamp N (2006) Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy 22:1180–1186
Mithoefer K, Williams RJ 3rd, Warren RF, Potter HG, Spock CR, Jones EC, Wickiewicz TL, Marx RG (2005) The microfracture technique for the treatment of articular cartilage lesions in the knee. A prospective cohort study. J Bone Joint Surg Am 87:1911–1920
Moran CJ, Barry FP, Maher SA, Shannon FJ, Rodeo SA (2012) Advancing regenerative surgery in orthopaedic sports medicine: the critical role of the surgeon. Am J Sports Med 40:934–944
Musahl V, Jordan SS, Colvin AC, Tranovich MJ, Irrgang JJ, Harner CD (2010) Practice patterns for combined anterior cruciate ligament and meniscal surgery in the United States. Am J Sports Med 38:918–923
Namdari S, Baldwin K, Anakwenze O, Park MJ, Huffman GR, Sennett BJ (2009) Results and performance after microfracture in National Basketball Association athletes. Am J Sports Med 37:943–948
Salzmann GM, Niemeyer P, Steinwachs M, Kreuz PC, Südkamp NP, Mayr HO (2011) Cartilage repair approach and treatment characteristics across the knee joint: a European survey. Arch Orthop Trauma Surg 131:283–291
Schneider U, Rackwitz L, Andereya S, Siebenlist S, Fensky F, Reichert J, Löer I, Barthel T, Rudert M, Nöth U (2011) A prospective multicenter study on the outcome of Type I collagen hydrogel-based autologous chondrocyte implantation (CaReS) for the repair of articular cartilage defects in the knee. Am J Sports Med 39:2558–2565
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (2003) Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy 19:477–484
Versier G, Dubrana F, The French Arthroscopy Society (2011) Treatment of knee cartilage defect in 2010. Orthop Traumatol Surg Res 97:S140–S153
Zhang AL, Kreulen C, Ngo SS, Hame SL, Wang JC, Gamradt SC (2012) Demographic trends in arthroscopic SLAP repair in the United States. Am J Sports Med 40:1144–1147
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Montgomery, S.R., Foster, B.D., Ngo, S.S. et al. Trends in the surgical treatment of articular cartilage defects of the knee in the United States. Knee Surg Sports Traumatol Arthrosc 22, 2070–2075 (2014). https://doi.org/10.1007/s00167-013-2614-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2614-9