Abstract
Purpose
Anterior cruciate ligament (ACL) ruptures are common, especially among young athletes, and such injuries may have considerable impact on both sport careers and everyday life. ACL reconstructions are successful for most patients, but some suffer from persistent giving-way symptoms and/or re-ruptures requiring revision surgery. The aim of this study was to evaluate the results after revision ACL reconstructions and compare them with the results in a control group consisting of primary ACL reconstructions.
Methods
This retrospective study included 56 patients undergoing revision ACL reconstruction and 52 patients receiving primary ACL reconstructions. The follow-up evaluation included clinical examination, instrumented laxity testing, testing of muscle strength, Tegner activity score, Lysholm score, Knee injury and osteoarthritis outcome score (KOOS) and radiological grading of osteoarthritis.
Results
The median time from the last ACL reconstruction to follow-up was 90 months in the revision ACL reconstruction group and 96 months in the primary ACL reconstruction group. The revision group had significantly inferior KOOS and Lysholm scores compared with the primary group. Patients in the revision group also showed greater laxity measured with the pivot shift test, a larger reduction in the Tegner activity score, reduced muscle strength in the injured knee, and more severe radiological osteoarthritis; however, no difference in anterior-posterior translation was found.
Conclusion
Inferior results were found on several of the testing parameters in the revision group compared with the primary group. Patients should receive this information prior to revision ACL reconstructions.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rupture of the anterior cruciate ligament (ACL) is a serious injury that may lead to abnormal laxity [22], increased risk of meniscal lesions [24] and degenerative changes [16, 22, 43]. Patients may experience pain and giving-way symptoms during activities of daily living and especially during sport activities [4, 15]. Patients experiencing such symptoms commonly receive ACL reconstructions. The results after ACL reconstructions are generally good [26, 27, 31], and patients can typically return to sport or recreational activities. However, some ACL reconstructions fail and revision ACL reconstruction is then an option. Since not all failures undergo revision surgery, the exact rate of failure is difficult to determine. Studies from the Danish Registry for Knee Ligament Reconstructions demonstrated a 3 % revision rate among primary reconstructions at a 2-year follow-up [29] and 4 % at a 5-year follow-up [30]. Most studies involving revision ACL reconstructions report relatively small numbers of patients [17, 21]. Some studies compare ACL revisions to primary reconstructions [19, 23, 45, 47, 48], but to our knowledge, no other study has directly compared the functional results of a revision group to a group of patients with primary ACL reconstructions concurrent in time. According to previous studies, the results after revisions seem to be inferior when compared with the results after primary reconstructions [6, 8, 21, 47]. The purpose of this study was to evaluate the results after revision ACL reconstruction surgery, compared with the results of a group of patients undergoing primary ACL reconstruction concurrent in time. The hypothesis was that there will be no differences in the results following revision ACL reconstructions compared with primary ACL reconstructions.
Materials and methods
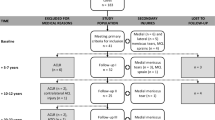
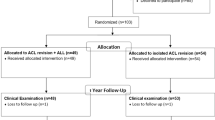
Patients who underwent revision ACL reconstructions (revision group = RG) at Trondheim University Hospital from 1993 to 2003 were considered eligible for the study. Patients undergoing primary ACL reconstruction (primary group = PG) immediately following the revisions in time were potential controls. The main indication for both the primary and the revision ACL reconstruction was giving-way symptoms. All patients were older than 18 years and skeletally mature with closed epiphyseal lines at the time of surgery. Patients in both groups were excluded if they had previously had direct suture of a ruptured ACL, major knee ligament surgery, extra-articular procedures or osteotomies, or if any of these procedures were conducted in the meantime between surgery and follow-up. In addition, patients in the primary group were excluded if a previous ACL reconstruction had occurred and the patients in the revision group if more than one previous ACL reconstruction was performed. The time from surgery to follow-up was set to be at least 2 years. A rehabilitation programme instructed by physiotherapists was implemented in both groups and consisted of immediate knee movement exercises, full passive extension several times a day and early weight bearing [18]. Knee braces were not prescribed for either group following surgery or during return to sports. Jogging was initiated at the ten- to 12-week time points. Return to sports was allowed after 6 months, provided that knee flexion and extension muscle strength had been restored and controlled functional training had been carried out without difficulty. The clinical examination at the follow-up evaluation included range of motion and laxity testing with the Lachman test, the pivot shift test and anterior-posterior translation in millimetres (mm) with the KT-1000 arthrometer® (MEDmetric, San Diego, CA, USA). The Lachman test grade zero and one indicated a negative test and <5 mm anterior displacement compared with the opposite side, respectively, while grade two and three were ≥5 mm and no clear endpoint. The pivot shift test grade zero and one indicated a negative shift and a glide, respectively, while grade two or three represented a pivot shift or a gross pivot shift. All examinations were carried out by one unblinded senior orthopaedic surgeon. Knee flexion and extension muscle strength was tested on a Biodex dynamometer® (Biodex Medical System, Inc., Shirley, NY, USA) by experienced physiotherapists. In addition, the Tegner activity score [44], the Lysholm functional score [44] and the Knee injury and osteoarthritis outcome score (KOOS) [40] were completed by the patients. Non-weight-bearing radiographs with frontal and lateral views in full extension were carried out for radiological osteoarthritis analysis using the Kellgren and Lawrence five grade system [25]. The grading was performed by a single senior radiologist. The study was approved by the regional ethical committee, and all patients signed informed consent forms.
Statistical analyses
All statistical analyses were conducted with IBM SPSS Statistics 19. Groups based on graft were tested against each other within the revision group and the primary group with the one-way ANOVA test, the independent t test, the nonparametric K independent-samples test and the chi square test or the Fisher’s exact test. The tests showed no significant differences between any of the functional parameters or any of the knee scores. The further statistical analyses were therefore based on comparisons between the revision group and the primary group. The chi square test was used to compare the categorical variables and the Fisher’s exact test when groups with small numbers were involved. The Tegner activity scores were assessed with the nonparametric Mann–Whitney U test. All scale variables for both groups were, in addition to the Lysholm and KOOS scores, tested with Q–Q plots and found approximately normally distributed. The independent-samples t test was therefore used for comparing equality of means. The level of statistical significance was p < 0.05, and all variables were considered independent.
Results
A total of 83 revision ACL reconstructions were carried out at Trondheim University Hospital from 1993 to 2003. Fourteen of these patients did not meet the inclusionary criteria (two second revisions, one third revision, one posterior cruciate ligament reconstruction, two patients with high tibial osteotomies and eight patients were excluded as the primary ACL reconstruction was an extra-articular transposition of the lateral third of the patellar ligament). Fifty-six out of 69 revised patients (81 %) were available for a clinical evaluation at the follow-up. The patients undergoing primary ACL reconstruction immediately after each of these 56 revision patients were potential controls, and 52 of the patients (93 %) in the PG were available for the follow-up evaluation. Three patients in the RG had an injured ACL in the contralateral knee at the follow-up evaluation. Therefore, the laxity testing and the evaluation of the muscle strength of these patients were excluded from further analyses. Retrospective review of the patient journals revealed that all revision ACL reconstructions except for one were performed as a one-stage procedure and that all the femoral tunnels were drilled with a transtibial technique. Only single-bundle reconstructions were performed and surgery was carried out under general or spinal anaesthesia with a tourniquet. Removal of the old hardware was performed when this compromised the drilling of the new tunnels or the fixation of the graft in the RG. Ipsilateral or contralateral bone patellar tendon bone grafts (BPTB grafts) or ipsilateral double-looped semitendinosus-gracilis grafts (hamstring grafts) were used for the ACL reconstructions (Table 1). No allografts were used. Twenty-three of the patients in the RG were found to have a new trauma leading to the need for revision ACL reconstruction. One patient had an infection as the cause of failure and another had failure of the graft fixation method. There were 57 % women in the RG and 56 % in the PG (n.s.). Mean age at the follow-up was 34 years (range 20–56) in the RG and 36 years (range 20–57) in the PG (n.s.). Twenty-nine patients (52 %) in the RG were injured in the left knee compared with 24 (46 %) in the PG (n.s.). No differences were found between the RG and the PG concerning median time from injury to the primary ACL reconstruction or median time from last reconstruction to follow-up. These figures are shown in Table 2.
Clinical results
Five patients in the RG had an extension deficit ≥5° compared with no patients in the PG (n.s.). A flexion deficit ≥5° was observed in six patients in the RG compared with one patient in the PG (n.s.). A total of eight patients had a Lachman test grade two or three in the RG (seven and one, respectively), compared with six (six and zero, respectively) in the PG (n.s.). The pivot shift test was graded two or three in 11 patients in the RG compared with two patients in the PG (p = 0.009). The mean side-to-side difference measured with the KT-1000 arthrometer® was 3.3 mm (SD ± 2.7, range 0–14) in the RG and 2.9 mm (SD ± 2.1, range 0–8) in the PG (n.s.). The distribution of the side-to-side differences is shown in Table 3.
The Biodex measurements in the RG showed significantly reduced strength in the injured knee compared with the uninjured knee in both mean total flexion work (p = 0.001) and mean total extension work (p < 0.001), mean peak flexion torque (p = 0.004) and mean peak extension torque (p < 0.001). Correspondingly, significant differences were found in peak extension torque (p = 0.001) in the PG (Table 4). When comparing percentage loss in muscle strength in the RG and the PG, the RG had significantly larger reductions in total flexion work values (p = 0.035) and total extension work values (p = 0.040). There were no significant differences between the two groups concerning peak flexion torque (n.s.) and peak extension torque (n.s.).
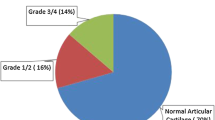
There was no difference between the two groups in the primary pre-injury median Tegner activity score or at the follow-up evaluation. However, there was a significantly larger median reduction in the Tegner activity score in the RG compared with the PG (p = 0.012). Significantly, more patients in the PG returned to their pre-injury level of sports or better compared with the RG (p = 0.006; Table 5). The mean Lysholm functional score at the follow-up was 80 (SD ±15, range 45–100) in the RG and 89 (SD ±9.4, range 54–100) in the PG (p = 0.001). The KOOS profiles for both groups are presented in Fig. 1. Mean total score in the RG was 70 (SD ±21, range 25–100) compared with 84 (SD ±13, range 50–100) in the PG (p < 0.001). The patients in the RG had significantly more severe radiological osteoarthritis compared with the PG (p = 0.045; Fig. 2).
Discussion
The main findings of this study were significantly inferior KOOS and Lysholm scores in the RG compared with the PG. A significantly larger number of revised patients also had a pivot shift test grade two or three, reduced muscle strength in the injured knee, a larger reduction in the Tegner activity score and significantly more severe radiological osteoarthritis. There were no significant differences between the RG and the PG concerning gender, age, injured knee, time from injury to primary reconstruction, time from last surgery to follow-up and the primary pre-injury Tegner activity score. Based on these findings and the fact that they underwent reconstructions concurrent in time performed by the same group of surgeons, the group consisting of patients with primary ACL reconstructions can be considered a matched control group to the RG. The strengths of this study are the relatively high number of patients in the RG, the comparison to the time-matched control group, the high follow-up rate (81 % in the RG and 93 % in PG) and the completeness of the follow-up evaluation including muscle strength testing in addition to regular clinical tests and questionnaires. The results from the current study are in accordance with other studies [2, 14, 21, 30, 48].
The RG in this study had a trend towards reduced extension range of motion compared with the PG. However, there were no differences in flexion range of motion in the two groups. Weiler et al. [47] found that revised patients had reduced knee extension motion compared with primary reconstructions, but no differences in knee flexion. The same authors [47] found no differences when testing for normal laxity with the Lachman test and the pivot shift test; however, we found significantly more revised patients with a pivot shift test grade two or three (p = 0.009). Musahl et al. [34] summarize that the posterolateral bundle of the ACL relaxes during knee flexion and is tight when the knee is fully extended. An explanation for the pivot shift test findings in the current study might be due to a tendency to place the revision femoral tunnel more dorsal (proximal) and thus perform an anteromedial bundle revision rather than a posterolateral bundle revision. Järvelä [20] found in a randomized controlled trial significantly better rotational laxity when performing a double-bundle ACL reconstruction compared with a single-bundle ACL reconstruction, measured with the pivot shift test. However, they found no differences between the two reconstruction methods when measuring anterior laxity [20]. Daniel et al. [9, 10] described that a side-to-side difference of 3 mm or more measured with the KT-1000 arthrometer in non-operated knees is associated with ACL failure. In the present study, 48 % of the patients in the RG and 50 % in the PG had a side-to-side difference of 3 mm or more at the follow-up. Denti et al. [11] found correspondingly 44 % in their revision group, and Eberhardt et al. [14], using patellar tendon autografts, found that 59 % of their patients had a side-to-side difference of 3.1 mm or more after revision. Noyes and Barber-Westin [36] found 47 % in the allograft group and 34 % in the autograft group. Several studies [1, 8, 11, 45] consider a side-to-side difference up to 5 mm as satisfactory laxity. In the current study, only 15 % of the patients in both the RG and the PG had a larger difference than 5 mm, and these findings correspond quite well with the number of patients found with a positive Lachman test and/or a positive pivot shift test.
Most studies examining revision ACL reconstruction have not performed muscle strength testing with a Biodex or similar instruments. We found an overall reduction in strength in the RG for the injured knee compared with the uninjured knee. These findings correspond well with the diminished results found in both clinical examination and various knee scores. Other studies [5, 13, 31, 33] have shown persisting loss of knee flexion strength when hamstring grafts are used for ACL reconstruction. The current study found significant differences in both total flexion work and total extension work when comparing the RG with the PG. In our study, most patients in the PG received BPTB grafts, this being the standard procedure at our department during the surgeries. Several long-term follow-up studies comparing BPTB grafts and hamstring grafts present no major differences between the two grafts [27, 38, 39, 41]. No allografts were used in the current study. Pallis et al. [37] found that young active individuals were significantly more likely to need revision ACL reconstruction when allografts were used in ACL reconstruction compared with autografts. A study based on the Danish Registry for Knee Ligament Reconstructions [30] found that allografts had two times the risk of re-revision surgery. Mayr et al. [32] reported comparable functional results between autografts and allografts when used in revision ACL reconstruction; however, a relatively low number of patients were included in that study. Causes of ACL failure were not completely analysed in the current study since pre-operative radiographs were unavailable for several of the patients in the revision group. Twenty-three cases of new trauma were, however, identified, in addition to one infection and one failure of the graft fixation method. New traumas were reported as cause of failure in 30 % of the cases in the revision group in a study presented by Trojani et al. [46].
The reduction in the activity score at the follow-up evaluation compared with pre-injury values was significantly larger in the RG compared with the PG; however, no significant difference in actual score was found between the two groups. Seven patients (13 %) in the RG and 18 patients (35 %) in the PG returned to their pre-injury activity level or better (p = 0.006). Diamantopoulos et al. [12] and Denti et al. [11] found that 36 and 78 % of their revision patients, respectively, returned to their pre-injury activity level. Similar to others [19, 47], we found that the mean Lysholm score in the RG was significantly inferior to the score in the PG (p = 0.001). Corresponding findings were also present for the KOOS scores (Fig. 1). A reduction in the Tegner activity score at the follow-up might be due to ageing of patients and thereby a natural change in social activities or a change in activity due to fear of re-injury. However, with significantly inferior results in other scores for the RG compared with the PG, it seems likely that the decrease in activity level can at least partially be explained by inferior function of the knee. The findings of significantly more severe radiological osteoarthritis in the RG could possibly be explained by a longer duration of abnormal knee joint laxity. The median time from primary ACL reconstruction to revision was 38 months. A second reconstruction may also be a contributing factor to the development of degenerative changes. Thomas et al. [45] found a higher rate of meniscal and chondral lesions in a revision group when compared with a group of primary ACL reconstructions. Kamath et al. [21] support this when summarizing in their review that continued abnormal laxity predisposes to further meniscal and chondral damage. In our study, 27 % of the patients in the RG had radiological osteoarthritis grade two or higher. Similar findings were reported by Niki et al. [35]. Other sources report presence of all radiographic degenerative changes after revision ACL reconstruction in 36–83 % of the cases [8, 12, 32, 42].
The main limitations of the current study are the retrospective design and the insufficient perioperative data on concomitant meniscal injuries and chondral lesions in both groups. The orthopaedic specialist carrying out the follow-up examinations was, due to practical reasons, not blinded. This study cannot shed light on the actual clinical improvement of the revised patients after the revision. Although the RG showed inferior results in several tests, most patients in both the RG and in PG had normal laxity and satisfactory knee function at the follow-up evaluation. Since the indication for both revision and primary ACL reconstructions in this study was subjective ACL instability, it should be fair to assume that most patients in both groups have experienced an ease of symptoms postoperatively. Other studies [3, 12, 47] that have scored patients both before and after revision ACL reconstruction describe significant improvement. Based on the results presented above, we recommend revision ACL reconstructions to patients experiencing major giving-way symptoms and a desire to participate in competitive sports, and to those patients not willing to modify physical activity level. When indicated, the revision ACL reconstruction should be conducted as early as possible to prevent subsequent knee injuries and the possible development of osteoarthritis [7]. As with other studies [2, 21, 28], we find it crucial to inform the patients about the potential risks and the inferior results following revision ACL reconstruction.
Conclusion
The revision ACL reconstruction group had significantly inferior Lysholm and KOOS scores compared with the primary ACL reconstruction group. There were also significantly more patients with a positive pivot shift test, reduced muscle strength in the injured knee and severe radiological osteoarthritis in the revision group. No difference in anterior-posterior translation was found between the two groups.
References
Aglietti P, Buzzi R, Giron F, Simeone AJ, Zaccherotti G (1997) Arthroscopic-assisted anterior cruciate ligament reconstruction with the central third patellar tendon. A 5–8-year follow-up. Knee Surg Sports Traumatol Arthrosc 5(3):138–144
Ahlden M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J (2012) The Swedish national anterior cruciate ligament register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med 40(10):2230–2235
Ahn JH, Lee YS, Chang MJ, Yim HS (2011) Analysis of revision anterior cruciate ligament reconstruction according to the combined injury, degenerative change, and MRI findings. Knee 18(6):382–386
Arnold JA, Coker TP, Heaton LM, Park JP, Harris WD (1979) Natural history of anterior cruciate tears. Am J Sports Med 7(6):305–313
Aune AK, Holm I, Risberg MA, Jensen HK, Steen H (2001) Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction. Am J Sports Med 29(6):722–728
Bach BR Jr (2003) Revision anterior cruciate ligament surgery. Arthroscopy 19(Suppl 1):14–29
Barenius B, Forssblad M, Engstrom B, Eriksson K (2012) Functional recovery after anterior cruciate ligament reconstruction, a study of health-related quality of life based on the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-2162-8
Battaglia MJ, Cordasco FA, Hannafin JA, Rodeo SA, O’Brien SJ, Altchek DW, Cavanaugh J, Wickiewicz TL, Warren RF (2007) Results of revision anterior cruciate ligament surgery. Am J Sports Med 35(12):2057–2066
Daniel DM, Malcom LL, Losse G, Stone ML, Sachs R, Burks R (1985) Instrumented measurement of anterior laxity of the knee. J Bone Joint Surg Am 67(5):720–726
Daniel DM, Stone ML, Sachs R, Malcom L (1985) Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med 13(6):401–407
Denti M, Lo Vetere D, Bait C, Schonhuber H, Melegati G, Volpi P (2008) Revision anterior cruciate ligament reconstruction: causes of failure, surgical technique, and clinical results. Am J Sports Med 36(10):1896–1902
Diamantopoulos AP, Lorbach O, Paessler HH (2008) Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med 36(5):851–860
Drogset JO, Strand T, Uppheim G, Odegard B, Boe A, Grontvedt T (2010) Autologous patellar tendon and quadrupled hamstring grafts in anterior cruciate ligament reconstruction: a prospective randomized multicenter review of different fixation methods. Knee Surg Sports Traumatol Arthrosc 18(8):1085–1093
Eberhardt C, Kurth AH, Hailer N, Jager A (2000) Revision ACL reconstruction using autogenous patellar tendon graft. Knee Surg Sports Traumatol Arthrosc 8(5):290–295
Feagin JA Jr, Curl WW (1976) Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med 4(3):95–100
Fetto JF, Marshall JL (1980) The natural history and diagnosis of anterior cruciate ligament insufficiency. Clin Orthop Relat Res 147:29–38
George MS, Dunn WR, Spindler KP (2006) Current concepts review: revision anterior cruciate ligament reconstruction. Am J Sports Med 34(12):2026–2037
Grontvedt T, Engebretsen L, Bredland T (1996) Arthroscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone grafts with and without augmentation. A prospective randomised study. J Bone Joint Surg Br 78(5):817–822
Harilainen A, Sandelin J (2001) Revision anterior cruciate ligament surgery. A review of the literature and results of our own revisions. Scand J Med Sci Sports 11(3):163–169
Jarvela T (2007) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 15(5):500–507
Kamath GV, Redfern JC, Greis PE, Burks RT (2011) Revision anterior cruciate ligament reconstruction. Am J Sports Med 39(1):199–217
Kannus P, Jarvinen M (1987) Conservatively treated tears of the anterior cruciate ligament. Long-term results. J Bone Joint Surg Am 69(7):1007–1012
Kartus J, Stener S, Lindahl S, Eriksson BI, Karlsson J (1998) Ipsi- or contralateral patellar tendon graft in anterior cruciate ligament revision surgery. A comparison of two methods. Am J Sports Med 26(4):499–504
Keene GC, Bickerstaff D, Rae PJ, Paterson RS (1993) The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am J Sports Med 21(5):672–679
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Laxdal G, Kartus J, Hansson L, Heidvall M, Ejerhed L, Karlsson J (2005) A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction. Arthroscopy 21(1):34–42
Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J (2007) Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med 35(5):740–748
Lind M, Lund B, Fauno P, Said S, Miller LL, Christiansen SE (2012) Medium to long-term follow-up after ACL revision. Knee Surg Sports Traumatol Arthrosc 20(1):166–172
Lind M, Menhert F, Pedersen AB (2009) The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc 17(2):117–124
Lind M, Menhert F, Pedersen AB (2012) Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the danish registry for knee ligament reconstructions. Am J Sports Med 40(7):1551–1557
Matsumoto A, Yoshiya S, Muratsu H, Yagi M, Iwasaki Y, Kurosaka M, Kuroda R (2006) A comparison of bone-patellar tendon-bone and bone-hamstring tendon-bone autografts for anterior cruciate ligament reconstruction. Am J Sports Med 34(2):213–219
Mayr HO, Willkomm D, Stoehr A, Schettle M, Suedkamp NP, Bernstein A, Hube R (2012) Revision of anterior cruciate ligament reconstruction with patellar tendon allograft and autograft: 2- and 5-year results. Arch Orthop Trauma Surg 132(6):867–874
Mohtadi NG, Chan DS, Dainty KN, Whelan DB (2011) Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev 9:CD005960
Musahl V, Kopf S, Rabuck S, Becker R, van der Merwe W, Zaffagnini S, Fu FH, Karlsson J (2012) Rotatory knee laxity tests and the pivot shift as tools for ACL treatment algorithm. Knee Surg Sports Traumatol Arthrosc 20(4):793–800
Niki Y, Matsumoto H, Enomoto H, Toyama Y, Suda Y (2010) Single-stage anterior cruciate ligament revision with bone-patellar tendon-bone: a case-control series of revision of failed synthetic anterior cruciate ligament reconstructions. Arthroscopy 26(8):1058–1065
Noyes FR, Barber-Westin SD (1996) Revision anterior cruciate ligament surgery: experience from Cincinnati. Clin Orthop Relat Res 325:116–129
Pallis M, Svoboda SJ, Cameron KL, Owens BD (2012) Survival comparison of allograft and autograft anterior cruciate ligament reconstruction at the United States military academy. Am J Sports Med 40(6):1242–1246
Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J (2007) A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med 35(4):564–574
Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M (2005) A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med 33(9):1337–1345
Roos EM, Toksvig-Larsen S (2003) Knee injury and osteoarthritis outcome score (KOOS)—validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 1:17
Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K (2011) Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: an 11-year follow-up of a randomized controlled trial. Am J Sports Med 39(10):2161–2169
Salmon LJ, Pinczewski LA, Russell VJ, Refshauge K (2006) Revision anterior cruciate ligament reconstruction with hamstring tendon autograft—5- to 9-year follow-up. Am J Sport Med 34(10):1604–1614
Sherman MF, Warren RF, Marshall JL, Savatsky GJ (1988) A clinical and radiographical analysis of 127 anterior cruciate insufficient knees. Clin Orthop Relat Res 227:229–237
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Thomas NP, Kankate R, Wandless F, Pandit H (2005) Revision anterior cruciate ligament reconstruction using a 2-stage technique with bone grafting of the tibial tunnel. Am J Sports Med 33(11):1701–1709
Trojani C, Beaufils P, Burdin G, Bussiere C, Chassaing V, Djian P, Dubrana F, Ehkirch FP, Franceschi JP, Hulet C, Jouve F, Potel JF, Sbihi A, Neyret P, Colombet P (2012) Revision ACL reconstruction: influence of a lateral tenodesis. Knee Surg Sports Traumatol Arthrosc 20(8):1565–1570
Weiler A, Schmeling A, Stohr I, Kaab MJ, Wagner M (2007) Primary versus single-stage revision anterior cruciate ligament reconstruction using autologous hamstring tendon grafts: a prospective matched-group analysis. Am J Sports Med 35(10):1643–1652
Wirth CJ, Kohn D (1996) Revision anterior cruciate ligament surgery: experience from Germany. Clin Orthop Relat Res 325:110–111
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gifstad, T., Drogset, J.O., Viset, A. et al. Inferior results after revision ACL reconstructions: a comparison with primary ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 21, 2011–2018 (2013). https://doi.org/10.1007/s00167-012-2336-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2336-4