Abstract
Purpose
This study evaluated knee laxity in anterior tibial translation and rotation following removal of anterior cruciate ligament (ACL) remnants using a computer navigation system.
Methods
This prospective study included 50 knees undergoing primary ACL reconstruction using a navigation system. ACL remnants were classified into four morphologic types: Type 1, bridging between the roof of the intercondylar notch and tibia; Type 2, bridging between the posterior cruciate ligament and tibia; Type 3, bridging between the anatomical insertions of the ACL on the lateral wall of the femoral condyle and the tibia; and Type 4, no bridging of ACL remnants. Anterior tibial translation and rotatory laxity were measured before and after remnant resection using a navigation system at 30°, 60°, and 90° of knee flexion. The amount of change in anterior tibial translation and rotatory laxity of each type was compared among the types.
Results
The different morphologic types of ACL remnants were as follows: Type 1, 15 knees; Type 2, 9 knees; Type 3, 6 knees; and Type 4, 20 knees. The amount of change in anterior tibial translation and rotatory laxity at 30° knee flexion in Type 3 was significantly larger than in the other types. There were no significant differences in either tibial translation or rotatory laxity at 60° and 90° knee flexion among the types.
Conclusions
In Type 3, ACL remnants contributed to anteroposterior and rotatory knee laxity evaluated at 30° knee flexion. The bridging point of the remnants is important to knee laxity. The Type 3 remnant should be preserved as much as possible when ACL reconstruction surgery is performed.
Level of evidence
Prognostic study, Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The occurrence of anterior cruciate ligament (ACL) injuries has significantly increased in recent times, and reconstruction of the ACL is one of the most frequently performed procedures in orthopaedic surgery [6]. It has been assumed that the clinical success of the ACL reconstruction depends on correct positioning of the graft tunnel [5, 13].
The computer navigation system used in ACL reconstruction not only improves the accuracy of the procedure, but also enables researchers to collect objective and quantitative data [6, 10–12, 16]. Previous studies regarding the relationship of the computer navigation system to conventional clinical examinations, including the Lachman test and the pivot-shift test, have already corroborated its validity as a kinematic evaluation tool [13–15, 17, 21].
In some cases, ACL remnants are found during knee arthroscopy for ACL injury. Recent studies have reported that ACL remnants contain several types of mechanoreceptors and that they may contribute to proprioceptive functioning in the knee [2, 20], but their biomechanical function is unknown. Particularly, there is no report about the contribution of the remnant to knee rotatory laxity. The purpose of this study was to assess anterior tibial translation and rotatory laxity of the knee depending on the type of ACL remnants and the knee joint angle. The hypothesis was that ACL remnants contribute to knee laxity.
Materials and methods
The study design was approved by the ethics committee at our institution, and all patients provided informed consent to participate in this study. From 2010 to 2012, ACL reconstruction was performed using a navigation system (OrthoPilot, B. Braun-Aesculap, Tuttlingen, Germany) on a consecutive series of 65 patients with ACL injury. Of these patients, 50 were included in this study. Exclusion criteria were revision ACL reconstruction, multiple knee ligament injury, bucket-handle tear of the medial or lateral meniscus, and navigation fixator loosening during surgery. There were 18 males and 32 females with a mean age of 22.9 ± 7.0 years (range 13–48 years). The diagnosis of ACL injury was determined by the Lachman test and the pivot-shift test, as well as a side-to-side difference of 3 mm or more measured using the KT-1000 arthrometer (MEDmetric, San Diego, CA, USA). MRI was performed in all patients to confirm the diagnosis of ACL injury and provide additional information on meniscal and other ligament injuries.
Arthroscopic evaluation
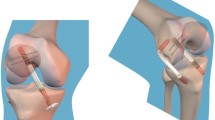
All surgeries were performed with patients under general anaesthesia. Arthroscopic intra-articular inspections were performed through lateral and medial infrapatellar portals with a 45° oblique arthroscope to identify any remaining ACL fibres and determine the nature of their attachment. A thorough arthroscopic probing is needed to precisely assess the ACL remnants, especially on the femoral attachment. The attachment of the ACL remnants was classified from the video of the arthroscopy by an orthopaedic surgeon who did not participate in the surgery. The ACL remnants were classified into 4 morphologic patterns: Type 1, bridging between the roof of the intercondylar notch and tibia; Type 2, bridging between the posterior cruciate ligament and tibia; Type 3, bridging between the anatomical attachments of the ACL on the lateral wall of the femoral condyle and the tibia; and Type 4, no bridging ACL remnants (Figs. 1, 2). All meniscal treatments were performed after testing for knee laxity to avoid any influence on the analysis results.
Intra-operative measurement with navigation system
The navigation system was used to evaluate the laxity of the knee in three dimensions including anteroposterior translation of the tibia as well as internal and external rotations of the tibia [12]. The accuracy of this system is extremely precise, and the cameras can track the position of the instruments to within <1 mm and <1° [23]. To begin the navigation process, after fixing the transmitters firmly to the femur and tibia with two Steinman pins of 2.0-mm diameter, extra-articular and intra-articular landmarks were registered with a pointer. After arthroscopic registration, the arthroscope was removed and arthroscopic fluid in the knee joint was evacuated as much as possible. All navigation processes and knee laxity tests were performed by a single surgeon (J, N). Maximum anterior load was applied manually to the tibia in neutral rotation, as well as internal rotation and external rotation of the tibia at 30°, 60°, or 90° of knee flexion. When the surgeon measured knee laxity, assistant surgeon held the thigh and kept knee flexion angle. This flexion angle indicated the monitor of navigation system. The surgeon held tibia by both hand and maximum anterior load was applied to the tibia in neutral rotation, as well as internal and external rotation of the tibia. In the first 10 cases, we measured it three times for anterior and rotatory laxity, and intra-class reliability was 0.983 and 0.988 at anterior laxity and rotatory laxity at 30° of knee flexion, respectively.
After the ACL remnants were resected, the anterior and rotatory laxity of the knee was evaluated in the same manner. Since there was no continuity in Type 4 remnants, the changes in anterior tibial translation and rotatory laxity before and after remnant resection were not examined (Fig. 3).
Statistical analysis
All data (the amount of change in anterior laxity and tibial rotation laxity) are presented as means and standard deviations. The amount of change in anterior tibial translation and rotatory laxity was compared among the morphologic types. Statistical analysis was conducted via Tukey’s analysis with SPSS for Windows software v 19.0 (SPSS Inc, Chicago, IL, USA). The minimum level of significance was set at P < 0.05.
Results
The percentage of patients presenting with ACL remnant patterns 1–4 was 30, 18, 13, and 40 %, respectively. The time between injury and surgery for patterns 1–4 was 6.8 ± 2.4, 2.7 ± 1.6, 4.3 ± 3.4, and 12.6 ± 7.3 months. The amount of change in anterior tibial translation and rotatory laxity at 30° of knee flexion in Type 3 was significantly larger than that in Types 1 and 2. There were no significant differences in either tibial translation or rotatory laxity at 60° or 90° of knee flexion among the types. The data for knee laxity before and after resection of the ACL remnants are summarized in Tables 1 and 2 (there was no change in Type 4, so it is not listed).
Discussion
The most important finding of the present study was that Type 3 ACL remnants contributed to anteroposterior and rotatory knee laxity evaluated at 30° of knee flexion. The femoral bridging point of the remnants is important to knee stability. Remnant-preserved ACL reconstruction may be beneficial for biomechanical stability.
Crain divided ACL remnants into four categories according to their morphology: (1) ACL remnant with scarring to the posterior cruciate ligament (PCL 38 %); (2) ACL remnant with scarring to the roof of the notch (8 %); (3) ACL remnant with scarring to the lateral wall of the notch or the medial aspect of the lateral femoral condyle (12 %), and (4) no identifiable ligament tissue remaining (42 %) [7]. In this study, remnants were initially categorized using this classification as a reference. However, there were remnants that were continuous near the ACL anatomical insertion. Thus, a new type was added to the evaluation. Compared with remnants at other insertion sites, the remnant that was continuous near the ACL anatomical insertion on the femur contributed significantly more to anterior and rotatory knee laxity at 30° knee flexion. ACL remnants with a small amount of ligament components (one quarter or less of the normal ACL) were classified as Type 4. However, the ligament components varied even for Type 3 remnants. That is, some Type 3 remnants had more ligament components and others had less. Thus, it is necessary to perform studies on the amount of remnant. In addition, the time between the injury and reconstruction can affect the remnants [7, 18, 19]. One study compared cases <1 year after injury and cases 1 year or more after surgery. In the current study, there were eight cases that underwent reconstruction 1 year or more after injury. These cases were all Type 4 in which there was no continuity of the remnant. Examinations were not performed in the period between the injury and surgery at 1 year after injury. Chronicity had a significant effect on changes in anteroposterior knee laxity evaluated at 30° of knee flexion after resection of the ACL remnant. Chronicity did not influence changes in rotatory knee stability after resection of the remnant [20].
There have been previous studies on remnants using the same type of navigation system [9, 10]. These studies suggested that remnants can contribute to the anteroposterior laxity at 30° knee flexion. However, there has been no report on the contribution to rotatory laxity. The current study focused on the insertion of the remnant and demonstrated, for the first time, the contribution of the remnant to both anteroposterior and rotatory laxity. Changes were compared before and after remnant resection.
There have been reports of improved proprioception and vascularity by preservation of the remnant and ACL reconstruction [2, 3, 8]. The presence of neural mechanoreceptors in the remnants of the ruptured ACL is a possible source of reinnervation of the ACL autologous graft [8]. In a rabbit model, the ACL was dissected and compared with a control group 4 months after a standardized surgically induced partial ACL tear. The results showed a significant increase in blood flow and vascular volume in the induced group [4]. Adachi et al. compared 40 patients in which they had performed a selective reconstruction of the anteromedial (AM) or posterolateral (PL) bundles to a group of patients with complete ACL reconstruction. The ACL augmentation group showed significantly better anteroposterior stability and terminal stiffness than the conventional ACL reconstruction group [1]. This study demonstrated that Type 3 remnants contributed not only to anterior stability but also rotatory stability. This finding can become a basis for recommendation of ACL augmentation surgery.
This study has some limitations. One limitation involves the method of measuring knee laxity. The navigation system is based on unmeasured manual load, which is one of the principal limitations of this study. The manually exerted load could not be precisely calibrated. However, only one practitioner performed the registration procedure for navigation and made the measurements. Therefore, errors should have been minimized. The patients with a partial tear of the ACL may have been included in Type 3 and may have influenced the results. The frequency of a partial tear of the ACL was 28 % according to Noyes et al. [19]. Otherwise the incidence of a symptomatic AM or PL bundle tear is reported to be between 5 and 10 % [22]. Based on the current concepts article [22], patients with AM bundle tears usually show a significantly increased anterior drawer test (+1) at 90° of knee flexion. The anterior translation in the Lachman test at 30° is rather small, and the pivot-shift test is negative or only slightly positive. Patients with AM bundle tears show a KT-1000 side-to-side difference between 2 and 4 mm. On the other hand, KT-1000 measurements of those with PL bundle tears show a small side-to-side difference of 1–3 mm. In this study, all patients showed a KT-1000 side-to-side difference of more than 4 mm. There is still a possibility that a partial tear was included in the remnant Type 3 in this study. Therefore, affirmation of the attachment of the ACL remnant and preservation of the Type 3 remnant are important when ACL reconstruction is performed.
A remnant has various types and attention is necessary. The surgeon performs an arthroscopic evaluation of the remnants carefully at the time of ACL reconstruction and should determine how you treat a remnant.
Conclusions
In Type 3, ACL remnants contributed to anteroposterior and rotatory knee laxity evaluated at 30° of knee flexion. The femoral bridging point of the remnants is important to knee laxity. The Type 3 remnant should be preserved as much as possible when ACL reconstruction surgery is performed.
References
Adachi N, Ochi M, Uchio Y, Sumen Y (2000) Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg 120:128–133
Adachi N, Ochi M, Uchino Y, Iwasa J, Ryoke K, Kuriwaka M (2002) Contribution of mechanoreceptors in the anterior cruciate ligament to the joint position sense knee. Acta Orthop Scand 73:330–334
Borbon CA, Mouzopoulos G, Siebold R (2012) Why perform an ACL augmentation? Knee Surg Sports Traumatol Arthrosc 20:245–251
Bray R, Leonard C, Salo P (2002) Vascular physiology and longterm healing of partial ligament tears. J Orthop Res 20:984–989
Buoncristiani AM, Tjoumakaris FP, Starman JS, Ferretti M, Fu FH (2006) Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy 22:1000–1006
Colombet P, Robinson J, Christel P, Franceschi JP, Djian P (2007) Using navigation to measure rotation kinematics during ACL reconstruction. Clin Orthop Relat Res 454:59–65
Crain EH, Fithian DC, Paxton EW, Luetzow WF (2005) Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy 21:19–24
Georgoulis A, Pappa L, Moebius U et al (2001) The presence of proprioceptive mechanoreceptors in the remnants of the ruptured ACL as a possible source of re-innervation of the ACL autograft. Knee Surg Sports Traumatol Arthrosc 9:364–368
Gohil S, Annear PO, Breidahl W (2007) Anterior cruciate ligament reconstruction using autologous double hamstrings: a comparison of standard versus minimal debridement techniques using MRI to assess revascurisation. J Bone Joint Surg Br 89:1165–1171
Hart R, Krejzla J, Svab P, Kocis J, Stipcak V (2008) Outcomes after conventional versus computer-navigated anterior cruciate ligament reconstruction. Arthroscopy 24:569–578
Hofbauer M, Valentin P, Kdolsky R, Ostermann RC, Graf A, Figl M, Aldrian S (2010) Rotational and translational laxity after computer-navigated single- and double\bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18:1201–1207
Ishibashi Y, Tsuda E, Tazawa K, Sato H, Toh S (2005) Intraoperative evaluation of the anatomical double-bundle anterior cruciate ligament reconstruction with the orthopilot navigation system. Orthopedics 28:s1277–s1282
Lee S, Kim H, Jang J, Seong SC, Lee MC (2012) Comparison of anterior and rotatory laxity using navigation between single- and double-bundle ACL reconstruction: prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 20:752–761
Lopomo N, Zaffagnini S, Bignozzi S, Visani A, Marcacci M (2010) Pivot-shift test: analysis and quantification of knee laxity parameters using a navigation system. J Orthop Res 28:164–169
Maeda S, Ishibashi Y, Tsuda E, Yamamoto Y, Toh S (2011) Intraoperative navigation evaluation of tibial translation after resection of anterior cruciate ligament remnants. Arthroscopy 27:1203–1210
Monaco E, Labianca L, Conteduca F, De Carli A, Ferretti A (2007) Double bundle or single bundle plus extraarticular tenodesis in ACL reconstruction? A CAOS study. Knee Surg Sports Traumatol Arthros 15:1168–1174
Nakamae A, Ochi M, Deie M, Adachi N, Kanaya A, Nishimori M, Nakasa T (2010) Biomechanical function of anterior cruciate ligament remnants: how long do they contribute to knee stability after injury in patients with complete tears? Arthroscopy 26:1577–1585
Muneta T, Koga H, Ju YJ, Horie M, Nakamura T, Sekiya I (2012) Remnant volume of anterior cruciate ligament correlates preoperative patient’s status and postoperative outcome. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-2023-5
Noyes FR, Bassett RW, Grood ES (1980) Arthroscopy in acute traumatic hemarthrosis of the knee. Incidence of anterior cruciate tears and other injuries. J Bone Joint Surg Am 62(687–695):757
Ochi M, Iwasa J, Uchino Y, Adachi N, Kawasaki K (2002) Induction of somatosensory evoked potentials by mechanical stimulation in reconstructed human anterior cruciate ligaments. J Bone Joint Surg Br 84:761–766
Robinson J, Carrat L, Granchi C, Colombet P (2007) Influence of anterior cruciate ligament bundles on knee kinematics: clinical assessment using computer-assisted navigation. Am J Sports Med 35:2006–2013
Siebold R, Fu F (2008) Assessment and augmentation of symptomatic anteromedial or posterolateral bundle tears of the anterior cruciate ligament. Arthroscopy 24:1289–1298
Tsuda E, Ishibashi Y, Fukuda A, Tsukada H, Toh S (2007) Validation of computer-assisted double-bundle anterior cruciate ligament reconstruction. Orthopedics 30:S136–S140
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakase, J., Toratani, T., Kosaka, M. et al. Roles of ACL remnants in knee stability. Knee Surg Sports Traumatol Arthrosc 21, 2101–2106 (2013). https://doi.org/10.1007/s00167-012-2260-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2260-7