Abstract
Purpose
To investigate the prevalence of patellofemoral osteoarthritis (OA) and to explore the association between radiographic patellofemoral OA and symptoms and function 12 years after anterior cruciate ligament (ACL) reconstruction.
Methods
The study participants (n = 221) were consecutively included at the time of an ACL reconstruction in the period from 1990 to 1997. Knee laxity (KT-1000), isokinetic quadriceps strength, triple jump, stair hop, and the Cincinnati knee score were measured 6 months, 1 year, 2 years, and 12 years after surgery. At the 12-year follow-up, visual analogue scale for pain, the Knee injury and Osteoarthritis Outcome Score, the Tegner activity scale, and radiographic examination (Kellgren and Lawrence score) were added. To analyse the association between patellofemoral OA, symptoms, and function, binary regression analyses presenting odds ratios and 95 % confidence intervals were used. The analyses were adjusted for age, gender, and body mass index.
Results
One hundred and eighty-one of the 221 subjects (82 %), including 76 females (42 %) and 105 males (58 %), were evaluated at the 12.3 ± 1.2-year follow-up. Mean age at the follow-up was 39.1 ± 8.7 years. Additional meniscal or chondral injuries at the time of reconstruction or during the follow-up period were detected in 116 subjects (64 %). Radiographic patellofemoral OA was found in 48 subjects (26 %), including 3 subjects with isolated patellofemoral OA (1.5 %). Those with patellofemoral OA were older, had more tibiofemoral OA, and had significantly more symptoms and impaired function compared with those without patellofemoral OA.
Conclusions
Patellofemoral OA was found in 26 % 12 years after ACL reconstruction. Patellofemoral OA was associated with increased age, tibiofemoral OA, increased symptoms, and reduced function. It is of clinical importance to include functional and radiographic assessment of the patellofemoral joint in the examination of long-term consequences following an ACL reconstruction.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellofemoral osteoarthritis (OA) is identified on radiographs as osteophytes and loss of articular cartilage on patella or in the femoral trochlear groove [26]. Symptoms of pain, stiffness, and functional limitations are disabilities found in patients with patellofemoral OA [8, 18]. Population-based studies of individuals above 40 years have reported a prevalence of radiographic patellofemoral OA between 3 and 9 % [7, 43]. In a systematic review from 2009 presenting the prevalence of OA after anterior cruciate ligament (ACL) reconstruction, only 7 of 31 included studies reported the results for the patellofemoral joint, with a prevalence between 0 and 22 % [30]. A limitation with most follow-up studies is that they either do not report results from the patellofemoral joint, or the prevalence of OA is merged for the patellofemoral and tibiofemoral joints [10, 31, 33, 42, 44, 46]. Furthermore, few studies have reported long-term clinical and functional findings on ACL reconstructed subjects with patellofemoral OA.
The patellofemoral joint is stabilized primarily by the medial and lateral patellofemoral and patellotibial structures including muscles, ligaments, and bone formations [26]. ACL and meniscus injuries have been shown to affect knee articular cartilage and bone morphology [2]. Furthermore, it has been suggested that single-bundle ACL reconstructions may change the patellofemoral contact area. The following cartilage load changes may initiate osteoarthritis and symptoms in the patellofemoral joint [48]. However, few studies have described the prevalence of patellofemoral OA after ACL reconstruction using bone-patellar-tendon-bone (BPTB) graft, and the relationship between radiographic patellofemoral OA and symptoms and function 12 years after ACL reconstruction.
Therefore, the first objective of this study was to report the prevalence of patellofemoral OA in patients on average 12 years after ACL reconstruction with or without additional injuries. Secondly, the objective was to evaluate the association between radiographic patellofemoral OA and symptoms and function. The hypothesis was that there is a significant association between patellofemoral OA, symptoms, and impaired function.
Materials and methods
Between 1990 and 1997, a total of 221 patients who underwent ACL reconstruction were included in four prospective studies with identical inclusion and exclusion criteria [4, 36, 37]. The included patients have been followed up as one longitudinal cohort with prospective assessments of knee function outcomes. The inclusion criteria comprised ACL reconstructed subjects between 14 and 50 years, either with isolated ACL injury, or combined with meniscal, and/or cartilage injury, and/or medical collateral ligament (MCL) injury. Patients with ACL injuries to the contralateral knee or other injuries to both extremities during the last year before surgery were excluded [31]. BPTB autograft procedure as previously described by Aune et al. [4] was used for ACL reconstruction: A 10-mm graft including tibial and femoral bone blocks was harvested via a longitudinal incision. From the medial side of the tibial tubercle, a guidewire was drilled using a drill guide (Linvatec Corp, Largo, FL, USA) and advanced to the preserved ligament stump in the posterior portion of the ACL footprint. With the knee flexed, a femoral aimer with 7-mm offset (Linvatec) was used through the tibial tunnel and positioned at 11 or 1 o’clock. Partial meniscal resections or sutures were performed for the meniscal injuries that needed treatment. Grade I and II MCL injuries were left untreated, but grade III injuries were repaired. The chondral lesions were shaved, and loose edges were removed. All subjects went through supervised rehabilitation over a 6–9 months period. The programme emphasized neuromuscular exercises and strength exercises to re-establish the knee function as described by Risberg et al. [34].
Two-year results on knee function have previously been published on 191 of these patients [4, 35], and long-term results for tibiofemoral OA and function and symptoms have recently been published [31]. The 221 included subjects have been followed for 12.3 ± 1.2 years with laxity tests, the Cincinnati knee score, isokinetic muscle strength test, triple jump test, and stair hop test at 6 months, 1 year, 2 years, and 12 years after surgery. In addition, radiographic assessment and the Knee injury and Osteoarthritis Outcome Score (KOOS), the Tegner activity scale, and a visual analogue scale (VAS) for pain were included at the 12-year follow-up.
The study has been approved by The Regional Committee for Medical and Health Research Ethics in Norway.
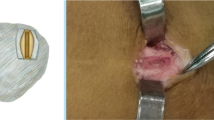
Radiological assessment
Standardized standing radiographs with the knee flexed approximately 40° in a specially designed frame were performed for the skyline projections. Lateral images were taken from the mediolateral side with the knees flexed 30–40°. For the tibiofemoral joint, posteroanterior radiographs using the SynaFlexer frame (Synarc, Inc., Copenhagen, Denmark), ensuring 20° of knee flexion and 5° external foot rotation, was used [19]. Both knees were examined for all the patients. The definition of patellofemoral OA was corresponding to Kellgren and Lawrence ≥ grade 2 [16], where grade 0 refers to no radiographic changes, grade 1 to minimal changes, grade 2 to definite osteophytes, grade 3 to multiple osteophytes and definite joint space narrowing, and grade 4 to severe radiographic changes. The radiological assessment was performed by one experienced radiologist who has shown intra-rater reliability (kappa) of 0.77 for Kellgren and Lawrence classification of the tibiofemoral joint [31].
Clinical and functional assessments
The KT-1000 manual maximum test was included at all the follow-ups [3]. We measured the difference (in millimetres) between the uninjured and the injured legs. The Cincinnati knee score (6–100 points) [29] was included at all the follow-ups to measure self-reported knee function. The KOOS [40] was used to measure self-reported knee function at the final follow-up. The questionnaire comprises 5 subscales of pain, other symptoms, activities of daily living (ADL), function in sports and recreation (Sport and Rec), and knee-related quality of life (QOL). Total sum for each score is transformed to a 0–100 scale, where 0 indicates severe problems with knee function and 100 indicates normal knee function. The KOOS questionnaire has been validated for measuring knee function in subjects with post-traumatic OA [39]. The Tegner activity scale was included at the 12-year follow-up. This scale includes questions related to weekly activity level and work activity and goes from 0 (sick leave) to 10 (pivoting sport at competitive level). The scale is validated for ACL injured subjects [24]. VAS for pain was included to measure self-reported pain during kneeling and activities. The patients marked on a 0–10 cm line, where 10 indicated no pain and 0 indicated severe pain. In addition, we included a question ‘Have you had knee pain during the last 4 weeks?’ to assess symptomatic knee OA corresponding to other literature [41]. Those who had knee pain and radiographic grade 2–4 on Kellgren and Lawrence classification were defined as having symptomatic radiographic patellofemoral OA.
Isokinetic muscle strength tests were performed at 6 months, 1 year, 2 years, and 12 years after the ACL reconstruction (Cybex 6000, Cybex Lumex Inc., Ronkonkoma, New York). The strength tests included 5 repetitions at 60°/s with 4 trial repetitions before the test. The results were presented for peak torque (PT) in Newtonmeter (NM) and for the leg symmetry index (LSI) for the 60°/s test. The LSI shows the per cent strength of the injured leg in comparison with the opposite leg. The triple jump test and stair hop test were included at all the follow-ups as complementary tests to assess knee function. For the triple jump test, the subjects started on two legs, jumped two steps on one leg before landing on two legs. For the stair hop test, the subjects hopped 22 steps up and down a stair on time. LSI values (%) are presented for the hop tests.
Other assessments
Body mass index (BMI) was calculated for all the follow-ups based on height (cm) and weight (kg). The additional injuries reported at the ACL reconstruction or sustained during the follow-up period were retrospectively registered by asking the patients on additional injuries and from the hospital chart for the entire period from the index operation to the 12-year follow-up. Additional injuries included medial or lateral meniscal injuries, cartilage lesions, or MCL injuries (grade III). Patients with isolated injury had to have isolated ACL injury for the entire follow-up period.
Statistical analysis
Descriptive data are given as frequencies and per cent or means and standard deviations. Binary logistic regression analysis was used to compare patellofemoral OA with those without patellofemoral OA (dependent variable) for a set of independent variables (age, gender, BMI, time from injury to surgery, KT-1000 results, VAS, the Cincinnati score, the KOOS scores, quadriceps strength, the triple jump test, and the stair hop test). Each analysis with the independent variables was adjusted for gender, age, and BMI at the 12-year follow-up. Odds ratios (OR), 95 % confidence intervals (CI), and p values were calculated for the logistic regression models. A p value of <0.05 was considered statistical significant. No sample size calculation was performed before the study started in 1990 as this study did not intend to compare two groups, but had a descriptive purpose.
Results
Of the 221 patients included at the time of surgery, 181 patients (82 %), 76 females (42 %) and 105 males (58 %) with a mean age of 39.1 ± 8.7 years, were available for the 12.3 ± 1.2-year follow-up. Seventeen subjects could not be found, 6 subjects lived abroad, 14 subjects did not want to participate, 1 subject was pregnant, 1 subject appeared to be included with both the left and the right knee and were excluded from the analyses, and 1 person had died. No differences in gender, age, or BMI at 6 months, 1 year, or 2 years were found between those who met and those lost to the 12-year follow-up. Patient characteristics for those with and without patellofemoral OA are presented in Table 1. Sixty-five subjects (36 %) had isolated ACL injury, and 116 subjects (64 %) had combined injuries reported at the time of ACL reconstruction (n = 108) or sustained during the 12-years follow-up (n = 8) (Table 2). Of those with meniscal injuries, 95 % had undergone a partial meniscal resection. Graft ruptures were seen in 15 subjects (8 %) of which all were revised. Other surgical procedures during follow-up have been presented previously including the following: shaving of chondral lesion and removing loose edges (n = 7), osteotomy (n = 1), removal of scar tissue (n = 12), removal of screws (n = 3), and arthroscopic procedures (n = 14). No other complications during the follow-up were found in surgical files or reported by the patients at the 12-year follow-up.
Prevalence of patellofemoral OA
The prevalence of OA in the patellofemoral and the tibiofemoral joints are presented in Table 3. A total of 48 subjects (26 %) had patellofemoral OA. Of these, 3 subjects (1.5 %) had isolated patellofemoral OA. Of those with patellofemoral OA, 27 (15 %) subjects had knee pain corresponding to symptomatic radiographic OA, but of those without radiographic patellofemoral OA, 70 subjects (39 %) had knee pain. Of patients with isolated ACL reconstruction 13 % had patellofemoral OA, and of patients with an additional injury, mainly meniscal injury, 34 % had patellofemoral OA (p < 0.05, but this association was non-significant after adjusting for tibiofemoral OA). Eleven subjects (6 %) had patellofemoral OA in the uninvolved knee. Of these, 5 subjects had no injury (2.5 %) and 6 subjects had either ACL or meniscal injury (3.5 %).
Factors associated with radiographic patellofemoral OA
Patellofemoral OA was significantly associated with increased age (OR, 1.08; 95 % CI, 1.03–1.122) and tibiofemoral OA (OR, 5.67; 95 % CI, 1.62–19.84). Furthermore, patellofemoral OA was significantly associated with impaired knee function and more symptoms as presented in Fig. 1. In addition, patellofemoral OA was significantly associated with pain during activity (OR, 0.85; 95 % CI, 0.72–0.99) and kneeling pain (OR, 0.89; 95 % CI, 0.80–0.99). Those with patellofemoral OA had lower quadriceps muscle strength than those without patellofemoral OA (OR, 0.989; 95 % CI, 0.979–0.999). No significant association was found neither between patellofemoral OA and knee laxity, nor patellofemoral OA and self-reported knee function, quadriceps strength or hop tests up to two years post-operatively.
Discussion
The most important finding of the present study was a prevalence of patellofemoral OA of 26 % on average 12 years after ACL reconstruction, including 1.5 % isolated patellofemoral OA. The prevalence of patellofemoral OA for the contralateral knee was 6 %, but only 2.5 % for uninjured contralateral knee. Symptomatic radiographic patellofemoral OA was shown in 15 %. In line with our hypothesis, significant associations were found between patellofemoral OA and more symptoms, pain, and impaired function.
Most of the subjects with patellofemoral OA had mild OA (22 %) reflecting definite osteophytes (grade 2). Only 4 % had moderate OA and none had severe patellofemoral OA (grade 4). In comparison, Hui et al. [14] found mild radiographic patellofemoral OA in 14 % and moderate radiographic patellofemoral OA in 2 % 15 years after endoscopic ACL reconstruction in patients with isolated ACL injury as classified by the IKDC classification. Furthermore, Ahn et al. [1] reported 7.6 % patellofemoral OA 10 years after ACL reconstruction with BPTB graft. Other long-term follow-up studies have reported a similar prevalence of patellofemoral OA between 0 and 22 % [5, 6, 9, 12, 17, 21–23, 25, 27, 28], indicating that the true prevalence of radiographic patellofemoral OA more than 10 years after ACL injury and reconstruction seems to be below 25–30 %. To evaluate OA, The Kellgren and Lawrence classification system was used in this study. Radiographic evaluation may give different results compared with arthroscopy when it comes to evaluation of structural changes in the joint. In addition, it could be questioned whether OA in the patellofemoral joint should be investigated as an isolated form of OA. The knee has three main compartments—the medial and the lateral tibiofemoral compartments, and the patellofemoral compartment. There is today limited knowledge supporting that OA in the patellofemoral joint is influenced by OA in one of the tibiofemoral compartments, but future studies may evaluate the knee joint as tri-compartmental with respect to assessment of OA.
Significant associations were found between patellofemoral OA and pain and symptoms (Table 3). However, most of those with patellofemoral OA had tibiofemoral OA as well. In comparison, others have found that knee pain and impaired function were more likely associated with combined patellofemoral and tibiofemoral OA than to OA in one compartment only [47]. Englund and Lohmander [9] reported that those with combined patellofemoral and tibiofemoral OA had more symptoms, lower function in sports and recreation, and worse knee-related QOL than subjects with tibiofemoral OA 15–22 years after meniscal resection. Their KOOS scores showed lower mean values compared with our results. This may be due to a 6-year longer follow-up period in their study or that our cohort also included subjects with isolated ACL injury. An isolated ACL injury has been shown to cause a high prevalence of mild radiographic OA (Kellgren and Lawrence classification), but it is not associated with self-reported or performance-based impaired knee function [31]. Few other studies have investigated the association between performance-based tests and patellofemoral OA for surgically treated ACL injured subjects. Neuman et al. [28] showed no differences between non-operatively treated ACL injured subjects with and without patellofemoral OA 15 years after ACL injury for the one-leg hop for distance test. However, in the present study, those with patellofemoral OA had significantly lower quadriceps strength at the 12-year follow-up than those without patellofemoral OA. Stefanik et al. [45] detected a significant relationship between quadriceps weakness and patellofemoral OA in a cross-sectional study. The authors speculated that the structural damage leads to symptoms and pain that induce muscle weakness. Furthermore, in a case series of 21 patients it was found that quadriceps weakness was associated with patellofemoral OA in older patients who had gone through ACL revision surgery [11]. It was also detected that activation failure was associated with patellofemoral OA in younger patients. Activation failure was calculated as the central activation ratio between maximal, voluntary isometric contraction torque and peak super imposed burst torque [11]. Thus, assessing muscle function prospectively after an injury to adjust the rehabilitation is important to improve muscle function, as normalized muscle function may contribute to prevent the development of OA [38].
Partial medial meniscal resection has been associated with cartilage defects in the patellofemoral and tibiofemoral joints measured by magnetic resonance imaging (MRI) up to 4 years after surgery [49]. In addition, cartilage defects were suggested to be early signs of development of OA in the patellofemoral and tibiofemoral joints. Due to a high correlation between meniscal resection and tibiofemoral OA as reported previously [32], the data in our study did not detect an association between patellofemoral OA and meniscus injuries. In a multiple regression model, Ahn et al. [1] did not identify predictors for developing patellofemoral OA 10 years after ACL reconstruction with BPTB graft. However, this may be due to the relatively low number of patients with patellofemoral OA (n = 9). Contrarily, Keays et al. [15] found a trend towards more patellofemoral OA for patients with higher age at the time of the ACL reconstruction in combination with cartilage damage and meniscectomy.
It is suggested that changes in patellofemoral contact area and pressures after single-bundle ACL reconstruction with BPTB graft may cause development of post-traumatic patellofemoral OA [48]. For instance, patella may tilt more laterally during flexion and tends to translate more laterally after an ACL reconstruction [48], and lack of normalized tibial rotation may contribute to altered loading areas contributing to the onset of a degenerative process. The surgical procedure in the present study may not have been optimal with respect to anatomical positioning of the graft leading to altered biomechanical environment in the patellofemoral joint. Hinman and Crossley [13] reviewed the literature on patellofemoral OA and reported that the properties of the patella cartilage differ biochemically and mechanically from that of tibia and femur. These divergent cartilage properties may be involved in the different experience of pain and symptoms for patients with respectively patellofemoral and tibiofemoral OA.
The present study has some limitations. A dropout rate of 19 % may have resulted in selection bias. Most of those who dropped-out lived abroad or could not be found indicating that the knee was not a direct reason for the dropout. We found no significant differences between dropouts and the study group for age or gender. Follow-up rates over 80 % have been considered as acceptable for long-term follow-up studies if the loss is missing at random, as we have assumed for our dropouts [20].
In summary, all follow-up studies after ACL reconstruction should include evaluation of the patellofemoral joint. The subjects with patellofemoral OA have significantly impaired function, including reduced quadriceps muscle strength and pain; thus, careful rehabilitation targeting patellofemoral structures should be implemented in early and long-term rehabilitation phases after ACL reconstruction.
Conclusion
Patellofemoral OA was found in 26 % 12 years after ACL reconstruction compared with 6 % in the contralateral knee, including 2.5 % OA in the contralateral non-injured knee. Patellofemoral OA was associated with increased age, tibiofemoral OA and reduced self-reported and performance-based function.
References
Ahn JH, Kim JG, Wang JH, Jung CH, Lim HC (2012) Long-term results of anterior cruciate ligament reconstruction using bone-patellar tendon-bone: an analysis of the factors affecting the development of osteoarthritis. Arthrosc PMID 22:421–565
Anderson DD, Chubinskaya S, Guilak F, Martin JA, Oegema TR, Olson SA, Buckwalter JA (2011) Post-traumatic osteoarthritis: improved understanding and opportunities for early intervention. J Orthop Res 29:802–809
Arneja S, Leith J (2009) Review article: validity of the KT-1000 knee ligament arthrometer. J Orthop Surg (Hong Kong) 17:77–79
Aune AK, Holm I, Risberg MA, Jensen HK, Steen H (2001) Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction. A randomized study with two-year follow-up. Am J Sports Med 29:722–728
Bourke HE, Gordon DJ, Salmon LJ, Waller A, Linklater J, Pinczewski LA (2012) The outcome at 15 years of endoscopic anterior cruciate ligament reconstruction using hamstring tendon autograft for ‘isolated’ anterior cruciate ligament rupture. J Bone Joint Surg Br 94:630–637
Cohen M, Amaro JT, Ejnisman B, Carvalho RT, Nakano KK, Peccin MS, Teixeira R, Laurino CF, Abdalla RJ (2007) Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy 23:629–634
Davies AP, Vince AS, Shepstone L, Donell ST, Glasgow MM (2002) The radiologic prevalence of patellofemoral osteoarthritis. Clin Orthop Relat Res 402:206–212
Duncan R, Peat G, Thomas E, Wood L, Hay E, Croft P (2009) Does isolated patellofemoral osteoarthritis matter? Osteoarthr Cartil 17:1151–1155
Englund M, Lohmander LS (2005) Patellofemoral osteoarthritis coexistent with tibiofemoral osteoarthritis in a meniscectomy population. Ann Rheum Dis 64:1721–1726
Ferretti A, Monaco E, Giannetti S, Caperna L, Luzon D, Conteduca F (2011) A medium to long-term follow-up of ACL reconstruction using double gracilis and semitendinosus grafts. Knee Surg Sports Traumatol Arthrosc 19:473–478
Hart JM, Turman KA, Diduch DR, Hart JA, Miller MD (2011) Quadriceps muscle activation and radiographic osteoarthritis following ACL revision. Knee Surg Sports Traumatol Arthrosc 19:634–640
Hertel P, Behrend H, Cierpinski T, Musahl V, Widjaja G (2005) ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg Sports Traumatol Arthrosc 13:248–255
Hinman RS, Crossley KM (2007) Patellofemoral joint osteoarthritis: an important subgroup of knee osteoarthritis. Rheumatology (Oxford) 46:1057–1062
Hui C, Salmon LJ, Kok A, Maeno S, Linklater J, Pinczewski LA (2011) Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for “isolated” anterior cruciate ligament tear. Am J Sports Med 39:89–98
Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC (2010) Factors involved in the development of osteoarthritis after anterior cruciate ligament surgery. Am J Sports Med 38:455–463
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS (2008) Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 16:442–448
Kornaat PR, Bloem JL, Ceulemans RY, Riyazi N, Rosendaal FR, Nelissen RG, Carter WO, Hellio Le Graverand MP, Kloppenburg M (2006) Osteoarthritis of the knee: association between clinical features and MR imaging findings. Radiology 239:811–817
Kothari M, Guermazi A, Von IG, Miaux Y, Sieffert M, Block JE, Stevens R, Peterfy CG (2004) Fixed-flexion radiography of the knee provides reproducible joint space width measurements in osteoarthritis. Eur Radiol 14:1568–1573
Kristman V, Manno M, Cote P (2004) Loss to follow-up in cohort studies: how much is too much? Eur J Epidemiol 19:751–760
Li RT, Lorenz S, Xu Y, Harner CD, Fu FH, Irrgang JJ (2011) Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. Am J Sports Med 39:2595–2603
Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J (2007) Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med 35:740–748
Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50:3145–3152
Lysholm J, Tegner Y (2007) Knee injury rating scales. Acta Orthop 78:445–453
Marcacci M, Zaffagnini S, Giordano G, Iacono F, Presti ML (2009) Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: a prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med 37:707–714
Minkowitz RB, Bosco JA III (2009) Patellofemoral arthritis. Bull NYU Hosp Jt Dis 67:30–38
Nakata K, Shino K, Horibe S, Tanaka Y, Toritsuka Y, Nakamura N, Koyanagi M, Yoshikawa H (2008) Arthroscopic anterior cruciate ligament reconstruction using fresh-frozen bone plug-free allogeneic tendons: 10-year follow-up. Arthroscopy 24:285–291
Neuman P, Kostogiannis I, Friden T, Roos H, Dahlberg LE, Englund M (2009) Patellofemoral osteoarthritis 15 years after anterior cruciate ligament injury—a prospective cohort study. Osteoarthr Cartil 17:284–290
Noyes FR, McGinniss GH, Mooar LA (1984) Functional disability in the anterior cruciate insufficient knee syndrome. Sports Med 1:278–302
Oiestad BE, Engebretsen L, Storheim K, Risberg MA (2009) Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med 37:1434–1443
Oiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, Fosdahl MA, Risberg MA (2010) Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 38:2201–2210
Oiestad BE, Holm I, Gunderson R, Myklebust G, Risberg MA (2010) Quadriceps muscle weakness after anterior cruciate ligament reconstruction: a risk factor for knee osteoarthritis? Arthritis Care Res (Hoboken) 62:1706–1714
Pernin J, Verdonk P, Si Selmi TA, Massin P, Neyret P (2010) Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med 38:1094–1102
Risberg MA, Beynnon BD, Peura GD, Uh BS (1999) Proprioception after anterior cruciate ligament reconstruction with and without bracing. Knee Surg Sports Traumatol Arthrosc 7:303–309
Risberg MA, Holm I, Steen H, Beynnon BD (1999) Sensitivity to changes over time for the IKDC form, the Lysholm score, and the Cincinnati knee score. A prospective study of 120 ACL reconstructed patients with 2 years follow-up. Knee Surg Sports Traumatol Arthrosc 7:152–159
Risberg MA, Holm I, Steen H, Eriksson J, Ekeland A (1999) The effect of knee bracing after anterior cruciate ligament reconstruction. A prospective, randomized study with two years’ follow-up. Am J Sports Med 27:1–8
Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A (1999) Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 29:400–412
Roos EM (2005) Joint injury causes knee osteoarthritis in young adults. Curr Opin Rheumatol 17:195–200
Roos EM, Lohmander LS (2003) The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64
Roos EM, Roos HP, Ekdahl C, Lohmander LS (1998) Knee injury and Osteoarthritis Outcome Score (KOOS)—validation of a Swedish version. Scand J Med Sci Sports 8:439–448
Roux CH, Saraux A, Mazieres B, Pouchot J, Morvan J, Fautrel B, Testa J, Fardellone P, Rat AC, Coste J, Guillemin F, Euller-Ziegler L (2008) Screening for hip and knee osteoarthritis in the general population: predictive value of a questionnaire and prevalence estimates. Ann Rheum Dis 67:1406–1411
Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K (2011) Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: an 11-year follow-up of a randomized controlled trial. Am J Sports Med 39:2161–2169
Segal NA, Glass NA, Torner J, Yang M, Felson DT, Sharma L, Nevitt M, Lewis CE (2010) Quadriceps weakness predicts risk for knee joint space narrowing in women in the MOST cohort. Osteoarthr Cartil 18:769–775
Shelbourne KD, Urch SE, Gray T, Freeman H (2012) Loss of normal knee motion after anterior cruciate ligament reconstruction is associated with radiographic arthritic changes after surgery. Am J Sports Med 40:108–113
Stefanik JJ, Guermazi A, Zhu Y, Zumwalt AC, Gross KD, Clancy M, Lynch JA, Segal NA, Lewis CE, Roemer FW, Powers CM, Felson DT (2011) Quadriceps weakness, patella alta, and structural features of patellofemoral osteoarthritis. Arthritis Care Res (Hoboken) 63:1391–1397
Struewer J, Frangen TM, Ishaque B, Bliemel C, Efe T, Ruchholtz S, Ziring E (2012) Knee function and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft: long-term follow-up. Int Orthop 36:171–177
Szebenyi B, Hollander AP, Dieppe P, Quilty B, Duddy J, Clarke S, Kirwan JR (2006) Associations between pain, function, and radiographic features in osteoarthritis of the knee. Arthritis Rheum 54:230–235
Tajima G, Iriuchishima T, Ingham SJ, Shen W, van Houten AH, Aerts MM, Shimamura T, Smolinski P, Fu FH (2010) Anatomic double-bundle anterior cruciate ligament reconstruction restores patellofemoral contact areas and pressures more closely than nonanatomic single-bundle reconstruction. Arthroscopy 26:1302–1310
Wang Y, Dempsey AR, Lloyd DG, Mills PM, Wrigley T, Bennell KL, Metcalf B, Hanna F, Cicuttini FM (2012) Patellofemoral and tibiofemoral articular cartilage and subchondral bone health following arthroscopic partial medial meniscectomy. Knee Surg Sports Traumatol Arthrosc 20:970–978
Acknowledgments
This study was funded by the Research Council of Norway and the South Eastern Health Authority in Norway.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Øiestad, B.E., Holm, I., Engebretsen, L. et al. The prevalence of patellofemoral osteoarthritis 12 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 21, 942–949 (2013). https://doi.org/10.1007/s00167-012-2161-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2161-9