Abstract
Purpose
The objective of this study was to analyze the morphology of the medial tibial plateau and lateral tibial plateau in Chinese knees and compared these measurements and features with those of commercial unicondylar tibial baseplates.
Methods
Three-dimensional knee models were reconstructed from computed tomography slices of 81 subjects. Among the series, 27 knees were from male subjects and 54 knees from female subjects. The dimensions and shape of the medial and lateral tibial plateaus were measured and compared with six commercially available unicondylar tibial baseplates.
Results
The results showed significant differences between the shapes of the medial and lateral tibial plateaus. For the lateral tibial plateau, the shape was symmetric about the mediolateral axis. The medial plateaus presented their widest mediolateral width in an obviously more posterior position than the lateral compartment. Additionally, the plateau aspect ratio decreased with increasing mediolateral dimensions, in contrast to the constant aspect ratio shown by conventional unicondylar knee prostheses.
Conclusion
Compartment-specific designs may optimize coverage between the prosthesis and resected tibial surface. The morphometrical measurements presented may allow manufacturers to design tibial baseplates that accommodate the structural variability between different ethnic groups.
Level of evidence
Prospective comparative study, Level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, unicondylar knee arthroplasty (UKA) has been the treatment of choice for isolated medial or lateral tibiofemoral osteoarthritis (OA) [11, 14]. The functional advantages of UKA over total knee arthroplasty (TKA) include greater range of motion (2 years, 127° vs. 118°, P < 0.01) [9], improved proprioception, more normalized joint kinematics, and excellent long-term survival rates [10, 13]. Whereas medial UKA is already used extensively, lateral UKA’s are increasing in popularity, with an incidence of 5–10% being reported. [15, 16]. Although previous studies suggested that the same baseplates and surgical principles might be unsuitable for use in both compartments [3, 12], there is insufficient information regarding the geometrical differences seen between the medial and lateral tibial plateau and how well current UKA tibial components conform to the plateau geometry.
Most surgeons agree that for a unicondylar replacement, the knee should be slightly under-corrected [12]. In this situation, the replaced tibial plateau will share some of the imposed loads with the contralateral component and sustain a higher external loading after UKA [5]. An undersized tibial baseplate could lead to component subsidence from loss of cortical bone support. Conversely, an oversized baseplate might overhang the resected surface, resulting in impingement of soft tissue. Currently available UKA prostheses in the Asian-Pacific market are produced to conform to Caucasian physiology. It is known that knee sizes in Asian people are smaller than in Western ethnicities [4, 24]. Thus, it is important to looking at the medial and lateral tibial plateau morphology to achieve a better anatomic match and clinical outcome for various ethnic groups.
The present study hypothesized that morphometrical parameters and the plateau aspect ratio of the lateral tibial plateau differed from those of the medial tibial plateau. Identical plateau designs may not provide adequate bone coverage of the resected tibial surface if a compartment-specific design is not considered. The study analyzed the morphology of the medial tibial plateau and lateral tibial plateau in Chinese knees and compared these measurements and features with plateau dimensions of different commercial unicondylar tibial baseplates.
Materials and methods
This study was approved by the ethics committee of the author’s institution. The study recorded the morphology of eighty-one normal knees (27 men, 54 women) without congenital anomalies or pathological deformities around the knee joint. The median age was 57 years (28–75). The median height was 155 cm (142–178), and the median weight was 60 kg (40–90).
Morphologic data were measured from three-dimensional proximal tibial models that were reconstructed from computed tomography (CT) images (HiSpeed CT/I system, GE Medical, USA). The patients were placed supine in the scanner with their knees taped to the scanner platform in the fully extended position. The bones were scanned with thicknesses ranging from 1.5 to 2.5 mm from the distal femur to proximal tibia, including the region 150 mm above and below the joint line. Image-processing software was used to punctuate and draw the cortical outline for reconstructing the bone model (Fig. 1). The resections and measurements were analyzed using the software, Pro/Engineer Wildfire 4.0 (Parametric Technologies Corp., Needham, MA, USA).
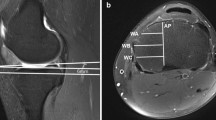
First, the line AB, defined in the mediolateral direction, was drawn over the upper tibial surface, and it was parallel and collinear to the surgical epicondylar axis of the femur in the coronal plane [21]. Another line CD was drawn perpendicular to the line AB in the anteroposterior direction and passed through its mid-point. Line M_AP, defined as the cut on the medial plateau in the sagittal plane, was drawn parallel to the line CD and tangential to the medial border of the cruciate ligament insertion. The assumed surgical techniques are expected to avoid damage to cruciate ligament attachments (Fig. 2a), as is currently the case for all UKA procedures. The same procedure was performed to draw another line L_AP for a lateral UKA. The line L_AP was drawn parallel to the line CD and tangential to the lateral border of the cruciate ligament insertion. A tibial surface cut to a depth of 5 mm was made along the tibial mechanical axis. Afterward, the desired cutting plane with 5° posterior and inferior slopes off the horizontal axis was simulated as the optimal cutting thickness (Fig. 2b).
Schematic representation of measurement methods used for the resection of the medial tibial plateau using a 3D solid model. a The line AB, taken as the widest mediolateral length over the upper tibial surface, drawn parallel and collinear to the surgical epicondylar axis of the femur. b The upper tibial cut was made 5 mm below the medial and lateral tibial plateau with a 5° posterior slope
The contours of the medial and lateral tibial plateaus were then measured for all models. The measurement accuracy was validated according to the authors’ previous study [6] with an accuracy of 0.1 mm. Six morphometrical parameters were measured on the resected surface (Fig. 3): the largest anteroposterior dimension (AP), the widest mediolateral dimension (ML), the perpendicular bisectors, MA and MP (anterior and posterior to the ML line along the AP line), the distance AD (from the point at the anterior of the AP line to the ML line), and the location ratio of anteroposterior direction (AD/AP × 100). In order to reduce the bias of morphometrical measurements, each measurement was done by two coauthors and ratified by the coauthors with a tolerance level of 0.1 mm of this study.
Schematic representation of the anthropometric parameters measured on the resected surface of the medial and lateral tibial plateau, including the anteroposterior dimensions (AP), the widest mediolateral dimension (ML), the distance AD (from the point at the anterior of the AP line to the ML line), the perpendicular bisectors, and MA and MP (anterior and posterior to the ML line along the AP line)
In addition, this study compared the AP, ML, and the plateau aspect ratio (AP/ML) of the resected medial and lateral tibial plateaus with six different commercially available unicondylar tibial baseplates: Accuris (Smith and Nephew, Memphis, TN, USA), Advance (Wright Medical Technology, Arlington, TN, USA), High Flex (Zimmer, Warsaw, IN, USA), Oxford (Biomet, Warsaw, IN, USA), Preservation (DePuy, Johnson and Johnson, Warsaw, IN, USA), and Unix (Stryker, Mahwah, NJ, USA) (Table 1).
Statistical analysis
For the statistical analysis, the Student’s t test and Pearson’s correlation were performed using SPSS (Version 12.0, SPSS, Chicago, IL, USA). The morphology of the medial and lateral tibial plateaus was compared using the paired t test with a level of significance set at P < 0.05.
Results
The mean overall values of AP and the ML were 47.1 ± 3.9 mm and 25.3 ± 2.3 mm, respectively. The medial tibial plateau displayed larger dimensions than the lateral tibial plateau (P < 0.05), and there were significant differences in shape. The morphologic measurements are summarized in Table 2.
In order to compare the shape of medial and lateral tibial plateau, the anthropometric data of MA, MP, AD, and location ratio (AD/AP × 100) were measured in this study. The results of MA and MP showed the medial side to be smaller than the lateral, but statistically, there were no significant differences. However, the results of AD and location ratio revealed the medial tibial plateau to be larger and with asymmetric geometry (Table 2). Additionally, the values of plateau aspect ratio (AP/ML) showed a significant difference between the two plateaus (P < 0.05). These results further demonstrated that the structure of the lateral tibial plateau differs from that of the medial side and is symmetric about the mediolateral axis.
Comparing the distribution of size and shape of the six commercially available unicondylar tibial baseplates with the collected resected surface data, most brands would display ML overhang for all ranges of AP and relatively constant values of plateau aspect ratio with increasing ML irrespective of whether the medial tibial plateau or lateral tibial plateau was under consideration. The regression lines of ML against AP of the resected surface for the medial tibial plateau and lateral tibial plateau were plotted and compared with the six commercially available components (Fig. 4). Additionally, the morphologic data showed a progressive descent in plateau aspect ratio (AP/ML) with increasing ML width (Fig. 5). Most of the commercial baseplates studied showed relatively constant values of plateau aspect ratio with increasing ML. The regression plot of AP/ML to ML for the commercial baseplates was lower than that of the morphologic data. One exception, the Preservation design, had an aspect ratio closer to that of the medial tibial plateau, showing a decreasing aspect ratio with increases in ML (Table 3).
Discussion
The most important finding of the present study was that the anatomic shape of the medial tibial plateau shows obvious differences from that of the lateral plateau. A compartment-specific baseplate design may help optimize coverage between the resected tibial surface and tibial baseplate. Tibial baseplates are designed to distribute loading over the tibial plateau, reducing stress concentrations in the underlying trabecular bone. It is suggested that surgeons should position the tibial baseplate to firmly contact the rim of the proximal tibia (stress transfer by cortical bone) [2, 22]. Previous studies have suggested the use of different UKA baseplates for the medial and lateral tibiofemoral compartments according to the differing anatomic shape and biomechanics [1, 16]. Significant dimensional and morphological differences were seen between the medial tibial plateau and lateral tibial plateau in this present study. Furthermore, the measured dimensions and plateau aspect ratio (AP/ML) of the commercial UKA prostheses were proven unsuitable for use in Asians. Therefore, based on our accumulated morphologic data, these findings demonstrate that a novel UKA system must be designed that is suitable for use in Chinese patients.
Quantification of the AP and ML revealed that the measurements of the lateral tibial plateau were significantly different from those of the medial tibial plateau in the Chinese population, comparable to finding in other studies [8, 17]. Simultaneously, our results showed that the AP and ML dimensions were obviously smaller than those reported in studies on Caucasian patients [17]. Comparing previous studies of the medial tibial plateau in Asian-Pacific knees, our results were slightly larger than the results of the Surendran et al. [19] but smaller than the results of Cheng et al. [7]. A possible cause for these inconsistencies was due to the high ratio of female patients involved in this present study, approximately 75%:25% female-to-male ratio. The proximal tibia is morphologically different for Chinese men and women [24, 25]. Therefore, further research may be needed to undertake a gender analysis for the medial tibial plateau and lateral tibial plateau.
The ratio of anteroposterior dimensions to mediolateral dimensions (AP/ML), defined as the PRA, is important in predicting the shape of knee prostheses. The results showed that the medial tibial plateau has a larger aspect ratio than the lateral tibial plateau. Furthermore, in order to accurately reveal the different morphology of the medial and lateral tibial plateaus, the AD and the location ratio for the widest mediolateral dimension on the resected surfaces were measured in this study. Both parameters were smaller for the lateral plateau. Moreover, the widest ML width was located close to the plateau center, and the shape was near symmetric about the mediolateral axis for the lateral tibial plateau. Conversely, the medial tibial plateau presented the widest ML width in a slightly more posterior position. Additionally, some reports have suggested that asymmetric tibial baseplates are more anatomic in nature and therefore cover the tibial plateau surface more completely than symmetric components in TKA [18, 20, 23]. These results may imply that compartment-specific designs could optimize the anatomic match between the prosthesis and the resected surface.
A good tibial baseplate design should conform to the size and shape of the resected surface. Comparing the morphologic data of AP and ML with the different commercially available unicondylar tibial baseplates, all of the commercial baseplates displayed an overhang for all measured AP lengths irrespective of whether the medial tibial plateau or lateral tibial plateau was under consideration, with one exception being the Preservation UKA (Fig. 4). These results were consistent with previous studies of Asian-Pacific knees [7, 19]. In practice, surgeons must avoid tibial component overhang to help prevent irritation of soft tissues and pain [5]. Additionally, in order to avoid damage to the cruciate ligament attachment sites, a smaller prosthetic size with suitable ML may be selected by the surgeon. However, insufficient tibial coverage may induce collapse or subsidence of the tibial baseplate [5]. These complications are similar to situations where the baseplate was placed in weaker cancellous bone. Insufficient coverage would induce posterior loosening or restricted movement with high flexion from the larger roll-back translation during a flexion-extension movement. Additionally, the morphologic data showed that decreasing values of the plateau aspect ratio correlated with increasing ML irrespective of whether the medial tibial plateau or lateral tibial plateau was being examined. In contrast, the majority of the baseplates showed a relatively constant value of plateau aspect ratio (AP/ML) with increasing ML, and all of the values surpassed the regression line of the morphologic data. Therefore, the baseplates should be modified with reduced ML dimensions and an inconstant value of plateau aspect ratio (AP/ML) to obtain a better anatomic fit for Chinese or Asian-Pacific populations.
A limitation of this study is that it contained a majority of female patients, so the study could not analyze differences between genders. Whether prostheses should be designed to conform to the differing morphology between male and female patients needs further study. Furthermore, in this study, the resected surface was based on the commonly performed proximal tibial cut for the medial and lateral tibial plateau. The rotational positioning of tibial baseplates is not considered. Obviating these limitations, this study not only demonstrates that a system suitable for use in Caucasians may not be suitable for other ethnic groups, but also can provide some information for design an appropriate series of unicondylar tibial baseplates.
The present study suggests that it may be useful to develop a compartmental-specific design that is more anatomically conforming to the resected surface of the medial and lateral tibial plateau of the Asian-Pacific population.
Conclusion
Examination of the resected surfaces of the Chinese knees in this study proved that the anatomic shape of the medial tibial plateau shows obvious differences from that of the lateral plateau. Additionally, the majority of unicondylar tibial baseplate in use in Asian countries was specifically designed for the Caucasian population. The present study supports the concept that compartment-specific designs or sufficient component sizes can optimize the anatomic match between the prostheses and the resected surface.
References
Ashraf T, Newman JH, Evans RL, Ackroyd CE (2002) Lateral unicompartmental knee replacement survivorship and clinical experience over 21 years. J Bone Jt Surg Br 84:1126–1130
Bartel DL, Burstein AH, Santavicca EA, Insall JN (1982) Performance of the tibial component in total knee replacement. J Bone Jt Surg Am 64:1026–1033
Baré JV, Gill HS, Beard DJ, Murray DW (2006) A convex lateral tibial plateau for knee replacement. Knee 13:122–126
Chaichankul C, Tanavalee A, Itiravivong P (2011) Anthropometric measurements of knee joints in Thai population: correlation to the sizing of current knee prostheses. Knee 18:5–10
Chau R, Gulati A, Pandit H, Beard DJ, Price AJ, Dodd CA, Gill HS, Murray DW (2009) Tibial component overhang following unicompartmental knee replacement–does it matter? Knee 16:310–313
Chang TW, Yang CT, Liu YL, Chen WC, Lin KJ, Lai YS, Huang CH, Lu YC, Cheng CK (2011) Biomechanical evaluation of proximal tibial behavior following unicondylar knee arthroplasty: modified resected surface with corresponding surgical technique. Med Eng Phys PMID: 21741289
Cheng FB, Ji XF, Zheng WX, Lai Y, Cheng KL, Feng JC, Li YQ (2010) Use of anthropometric data from the medial tibial and femoral condyles to design unicondylar knee prostheses in the Chinese population. Knee Surg Sports Traumatol Arthrosc 18:352–358
Cheng FB, Ji XF, Lai Y, Feng JC, Zheng WX, Sun YF, Fu YW, Li YQ (2009) Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee 16:341–347
Fisher DA, Dalury DF, Adams MJ, Shipps MR, Davis K (2010) Unicompartmental and total knee arthroplasty in the over 70 population. Orthopedics 33:668
Hamilton WG, Ammeen D, Engh CA Jr, Engh GA (2010) Learning curve with minimally invasive unicompartmental knee arthroplasty. J Arthroplasty 25:735–740
Hang JR, Stanford TE, Graves SE, Davidson DC, de Steiger RN, Miller LN (2010) Outcome of revision of unicompartmental knee replacement. Acta Orthop 81:95–98
Heyse TJ, Tibesku CO (2010) Lateral unicompartmental knee arthroplasty: a review. Arch Orthop Trauma Surg 130:1539–1548
Koskinen E, Paavolainen P, Eskelinen A, Harilainen A, Sandelin J, Ylinen P, Tallroth K, Remes V (2009) Medial unicompartmental knee arthroplasty with Miller-Galante II prosthesis: mid-term clinical and radiographic results. Arch Orthop Trauma Surg 129:617–624
Naal FD, Fischer M, Preuss A, Goldhahn J, von Knoch F, Preiss S, Munzinger U, Drobny T (2007) Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med 35:1688–1695
Pennington DW, Swienckowski JJ, Lutes WB, Drake GN (2006) Lateral unicompartmental knee arthroplasty: survivorship and technical considerations at an average follow-up of 12.4 years. J Arthroplasty 21:13–17
Sah AP, Scott RD (2007) Lateral unicompartmental knee arthroplasty through a medial approach. Study with an average five-year follow-up. J Bone Jt Surg Am 89:1948–1954
Servien E, Saffarini M, Lustig S, Chomel S, Neyret P (2008) Lateral versus medial tibial plateau: morphometric analysis and adaptability with current tibial component design. Knee Surg Sports Traumatol Arthrosc 16:1141–1145
Stulberg BN, Dombrowski RM, Froimson M, Easley K (1995) Computed tomography analysis of proximal tibial coverage. Clin Orthop Relat Res 311:148–156
Surendran S, Kwak DS, Lee UY, Park SE, Gopinathan P, Han SH, Han CW (2007) Anthropometry of the medial tibial condyle to design the tibial component for unicondylar knee arthroplasty for the Korean population. Knee Surg Sports Traumatol Arthrosc 15:436–442
Tang Q, Zhou Y, Yang D, Xu H, Liu Q (2010) The offset of the tibial shaft from the tibial plateau in Chinese people. J Bone Jt Surg Am 92:1981–1987
Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y (2002) Anthropometry of the proximal tibia to design a total knee prosthesis for the Japanese population. J Arthroplasty 17:1028–1032
Walker PS (1989) Requirements for successful total knee replacements. Design considerations. Orthop Clin N Am 20:15–29
Westrich GH, Haas SB, Insall JN, Frachie A (1995) Resection specimen analysis of proximal tibial anatomy based on 100 total knee arthroplasty specimens. J Arthroplasty 10:47–51
Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G (2011) Differences of knee anthropometry between Chinese and white men and women. J Arthroplasty 26:124–130
Yue B, Varadarajan KM, Ai S, Tang T, Rubash HE, Li G (2011) Gender differences in the knees of Chinese population. Knee Surg Sports Traumatol Arthrosc 19:80–88
Acknowledgments
The authors acknowledge the financial support from the Southern Taiwan Science Park (STSP) (BY-03-04-17-98) and the National Science Council (NSC 98-2221-E-195-001 and NSC 99-2221E-195-001).
Conflict of interest
No conflicts of interest on this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chang, TW., Huang, CH., McClean, C.J. et al. Morphometrical measurement of resected surface of medial and lateral proximal tibia for Chinese population. Knee Surg Sports Traumatol Arthrosc 20, 1730–1735 (2012). https://doi.org/10.1007/s00167-011-1749-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1749-9