Abstract
The purpose of this study was to analyze the in vivo dimensions of each tibial plateau for planning of unicompartmental knee arthroplasty (UKA), and to compare the morphometric data to the dimensions of nine current designs of UKA tibial components. Thirty-seven knees (31 females and 6 males) operated on with UKA were studied. All patients were examined postoperatively using computed tomography (CT). There were 18 lateral and 19 medial UKAs. On the CT scan, each operated tibial plateau was measured in the transverse plane at the resection level, just below the full polyethylene tibial component. We measured the length of the anteroposterior (AP) cut as well as the maximal mediolateral dimension of the resected plateau (perpendicular to the AP cut). We compared the measurements with nine current UKA systems: Accuris (Smith and Nephew), Advance (Wright Medical), HLS Uni Evolution (Tornier), Miller-Galante and “ZUK” (Zimmer), Oxford and Oxford α (Biomet), Preservation (DePuy) and Unix (Stryker). There was good correlation between patient height and mediolateral dimension (r = 0.6), and between patient height and area of total tibial plateau (r = 0.7). The anteroposterior dimension was greater for the medial plateau (mean 50.8 mm, SD 3.3) than for the lateral plateau (mean 47.2 mm, SD 3.3). This difference was statistically significant (P = 0.0016). Some UKA implants are designed with an asymmetric femoral component, but none have an asymmetric tibial component. The present study suggests, however, that the shape of the medial tibial plateau differs from that of the lateral plateau. This difference can lead to mediolateral overhang for medial UKA, if the surgeon aims for optimal anteroposterior coverage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Encouraging results have been published about unicompartmental knee arthroplasty (UKA), mostly in the medial compartment [4, 12]. UKA is a suitable procedure for elderly patients with unilateral knee osteoarthritis. However, indications are still not well defined, especially in the lateral compartment. The clinical outcome of UKA in both compartments is difficult to assess because published studies have not compared different implant designs.
Numerous studies [7, 20] have reported anatomical analyses of the tibial plateau, although most authors considered implications for total knee arthroplasty [6–9, 18, 19] or allograft sizing [11, 15]. Furthermore, during a UKA procedure, the tibial resection is made at different levels, usually between 7 and 9 mm below the joint line, regardless of implant design. The choice of tibial implant size is made either preoperatively using templates [3], or more often interoperatively by the surgeon’s visual estimate and measurement. However, the variety of available UKA implants may not perfectly fit the resected tibial plateau.
The purpose of this study was to analyze the dimensions of the medial and lateral tibial plateaus for planning of unicompartmental knee arthroplasty; and compare different current UKA tibial component designs to the anatomy of the medial and lateral tibial plateaus.
Material and methods
We studied UKAs in thirty-seven knees (31 females and 6 males). All patients were examined postoperatively using computed tomography (CT) with three-dimensional reconstruction analysis. There were 18 lateral and 19 medial UKAs: the mean patient height was 162 cm (±8.4; 147–178) and the mean weight was 65 kg (±10.5; 49–93).
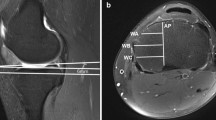
All patients were scanned following an identical protocol by the same senior radiologist (SC). The CT scans were taken with a thickness of 1 mm, from the superior margin of the patella to the anterior tibial tuberosity. We used image-processing software dedicated to DICOM images, OsiriX (open-source software; http://homepage.mac.com/ rossetantoine/osirix) for analysis. The operated tibial plateau was digitized at the resection level in the transverse plane. The anteroposterior (AP) cut was digitized and the maximal mediolateral (ML) width was measured by drawing a line perpendicular to the AP cut (Fig. 1). The total area of the tibial plateau (AT) was also measured and the area of the resected tibial plateau (AR), both of which were obtained by digitizing closed loop bone contours in Osirix at the resection level (Fig. 2). All measurements were done by the same author (ES). In all patients, the implanted tibial component was full-thickness polyethylene and accordingly, there were no artifacts due to metal-backed components.
We compared the AP and ML measurements, as well as the aspect ratio (AP/ML), to the dimensions of nine current prosthetic systems: Accuris (Smith and Nephew, Memphis, TN, USA), Advance (Wright Medical Technology, Arlington, TN, USA), HLS Uni Evolution (Tornier, St-Ismier, France), Oxford and Oxford α (Biomet, Warsaw, IN, USA), Miller-Galante (Zimmer, Warsaw, IN, USA), Preservation (DePuy, Warsaw, IN, USA), Unix (Stryker, Mahwah, NJ, USA) and “ZUK” Zimmer unicompartmental knee system (Zimmer, Warsaw, IN, USA). Data from lateral tibial and medial tibial plateaus were analyzed independently.
Statistical analysis was performed by using Student’s t-test and Pearson’s correlation by using Microsoft Excel (Microsoft Corp, Redmond, WA, USA). The morphometric data (age, AP and ML dimension, tibial area) were compared in medial and lateral UKAs. Correlations between variables were calculated using the Pearson product moment coefficient of correlation (r). The significance level was set at P < 0.05.
Results
The mean area of the resected tibial plateau was 37% (10.9 cm²) of the total area of the tibial plateau (29 cm²). The AP dimension averaged 49 mm (±2.4; 42.6–60.5) and the ML dimension averaged 29 mm (±2.4; 24.2–35.4). The aspect ratio (AP/ML) was 1.7 (±0.2; 1.4–2.0).
For the medial plateau, the mean resected area was 10.9 cm² (±1.4; 8.1–13.6) and the total plateau area was 29.4 cm² (±4.1; 23.4–39.0). The medial tibial plateau represented 37.2% (±3.8; 32.6–46.4) of the total tibial area.
For the lateral plateau, the mean resected area was 10.5 cm² (±2.1; 7.2–16.5) and the total plateau area was 28.4 cm² (±4.2; 24.0–40.8). The lateral tibial plateau represented 36.7% (±3.0; 28.5–41.6) of the total tibial area.
The AP and ML dimensions and the aspect ratio (AP/ML) for lateral and medial plateaus are summarized in Table 1. There were significant differences between the medial and lateral tibial plateaus in the AP dimension (P = 0.0016) and the aspect ratio (P = 0.0005). There was a correlation between patient height and ML dimension (r = 0.62) and between patient height and the total tibial area (r = 0.70).
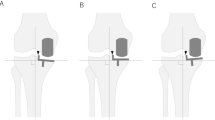
Comparison between our data and the different designs of tibial components revealed that some implant systems had an inadequate AP size range (Table 2), and that one had an inadequate ML size range (Table 3). For some implants, even the largest size tibial component had an insufficient AP dimension in the study (Fig. 3).
Comparison between lateral/medial plateau dimensions and dimensions of different designs of tibial components. The AP and ML dimensions of the Oxford, Miller-Gallante and HLS Uni evolution are closer to the lateral plateau dimension. The AP and ML dimensions of the Preservation, Oxford α and ZUK are closer to the medial plateau dimension. The Accuris implant seems too small for the present population. Lateral versus medial tibial plateau: morphometric analysis and adaptability with current tibial component design
Some tibial implants had an aspect ratio closer to that of the lateral tibial plateau, while others were closer to the medial plateau (Table 4). The Oxford α and the ZUK tibial implants covered the entire population range and their aspect ratio was closest to the medial plateau (Table 2). The Accuris, Oxford, Miller-Galante, Unix and HLS Uni Evolution tibial implants had a closer aspect ratio, i.e., a closer shape to the lateral plateau (Fig. 3).
Discussion
Our study suggests that the shape of the medial tibial plateau differs from that of the lateral plateau. Because of a different aspect ratio (AP/ML) between the medial and the lateral plateaus at the level of the cut, some implant designs may lead to a medio-lateral overhang to obtain good antero-posterior coverage. In practice, surgeons do not favor implants with insufficient tibial coverage as this induces the possibility of tibial implant collapse [2, 10] as load will be transmitted to cancellous bone as opposed to cortical bone. Another concern with insufficient coverage would be posterior loosening during to the femoral rollback. There are no reports to date that suggest a link between early tibial implant failure and insufficient bone coverage even though we may expect that cortical bearing of the tibial component should be better.
Few studies [5, 16] have analyzed the correlation between tibial anatomy and implant design for UKA. Fitzpatrick et al. [5] measured the shape of the tibial plateau by modeling of the tibial resection as described by Surendran et al. [16]. Furthermore Surendran et al. analyzed a large cohort of cadavers with gender analysis. Our series contains a majority of female patients and for this reason we could not undertake a gender analysis. In terms of the anatomy of the tibial plateau, we found a correlation between the patient height and the AP dimension as Surendran et al. [16]. In a recent study performed for sizing of meniscal allograft, Stone [15] found a linear correlation (r = 0.7) between patient height and the total tibial plateau width which is in line with results of the present study.
Because of the different anatomy and movement in the lateral compartment, Baré et al. [1] suggested use of different components on the lateral side. In our experience [14], the results of lateral UKA are as good and reliable as those of medial UKA. However, some surgeons remain reluctant to perform UKA on the lateral side because of discouraging results in the literature [12, 17]. We believe the main cause of failure in lateral UKA is due to improper selection, indication or technique (overcorrection) rather than an inadequate tibial implant, except mobile bearing implants [13] in the lateral compartment. Some implants appear closer to the lateral tibial plateau anatomy than the medial plateau. In the study of Surendran et al. [16], the Depuy design (preservation) followed the population anatomy more closely for the medial plateau. In the present study, the Oxford α and the ZUC appeared closest to the shape of tibial cut on the medial plateau. Accordingly, some implant designs might be more suitable for lateral compartment.
The principal weakness in the present study is that we took all measurements immediately below the full-polyethylene tibial component, at about 9 mm below the joint line, and we cannot be certain that dimensions would be identical if measured 7 mm below the joint line, for instance. We believe, however, that every implant (with the adequate polyethylene thickness) should be suitable for a cut 9 mm below the joint line. Another critique to our methodology is that, whereas data were obtained in vivo, we followed the AP resection line selected by the surgeon during surgery, which may not always be at the correct or ideal level.
This study could help surgeons understand some cases of failure. Some of the patients in the present study had good indications for UKA (no overweight, slight postoperative undercorrection) but continue to suffer from pain. In some patients, notably medial UKAs, the tibial component may have an ML overlap. This may be a cause of pain due to soft tissue impingement.
Conclusion
The present study highlights that some implant designs are more suitable for the lateral plateau anatomy and vice versa. We suggest that a better coverage of the tibial plateau could be a key success factor. In fact the surgeon selects a smaller tibial implant to avoid ML overhang, while compromising AP coverage for a medial UKA. Conversely, those implants should be more suitable for the lateral compartment with a better coverage.
References
Bare JV, Gill HS, Beard DJ, Murray DW (2006) A convex lateral tibial plateau for knee replacement. Knee 13:122–126
Bohm I, Landsiedl l (2000) Revision surgery after failed unicompartmental knee arthroplasty: a study of 35 cases. J Arthroplasty 15:982–989
Bothra V, Lemon G, Lang D, Smith DM, Ali AM (2003) Reliability of templating in estimating the size of uni-condylar knee arthroplasty. J Arthroplasty 18:780–783
Deshmukh RV, Scott RD (2001) Unicompartmental knee arthroplasty: long-term results. Clin Orthop Relat Res 392:272–278
Fitzpatrick C, FitzPatrick D, Lee J, Auger D (2007) Statistical design of unicompartmental tibial implants and comparison with current devices. Knee 14:138–144
Hitt K, Shurman JR, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA (2003) Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am 85:115–122
Incavo SJ, Ronchetti PJ, Howe JG, Tranowski JP (1994) Tibial plateau coverage in total knee arthroplasty. Clin Orthop Relat Res 299:81–85
Kwak DS, Surendran S, Pengatteeri YH, Park SE, Choi KN, Gopinathan P, Han SH, Han CW (2007) Morphometry of the proximal tibia to design the tibial component of total knee arthroplasty for the Korean population. Knee 14:295–300
Lemaire P, Pioletti DP, Meyer FM, Meuli R, Dorfl J, Leyvraz PF (1997) Tibial component positioning in total knee arthroplasty: bone coverage and extensor apparatus alignment. Knee Surg Sports Traumatol Arthrosc 5:251–257
McAuley JP, Engh GA, Ammeen DJ (2001) Revision of failed unicompartmental knee arthroplasty. Clin Orthop Relat Res 392:279–282
McDermott ID, Sharifi F, Bull AM, Gupte CM, Thomas RW, Amis AA (2004) An anatomical study of meniscal allograft sizing. Knee Surg Sports Traumatol Arthrosc 12:130–135
Murray DW, Goodfellow JW, O’Connor JJ (1998) The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br 80:983–989
Robinson BJ, Rees JL, Price AJ, Beard DJ, Murray DW, McLardy Smith P, Dodd CA (2002) Dislocation of the bearing of the Oxford lateral unicompartmental arthroplasty. A radiological assessment. J Bone Joint Surg Br 84:653–657
Servien E, Verdonk PM, Aïtsiselmi T, Neyret P (2007) How to select candidates for lateral unicompartmental prosthesis. Techn Knee Surg 6:51–59
Stone KR, Freyer A, Turek T, Walgenbach AW, Wadhwa S, Crues J (2007) Meniscal sizing based on gender, height, and weight. Arthroscopy 23:503–508
Surendran S, Kwak DS, Lee UY, Park SE, Gopinathan P, Han SH, Han CW (2007) Anthropometry of the medial tibial condyle to design the tibial component for unicondylar knee arthroplasty for the Korean population. Knee Surg Sports Traumatol Arthrosc 15:436–442
Svard UC, Price AJ (2001) Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br 83:191–194
Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y (2002) Anthropometry of the proximal tibia to design a total knee prosthesis for the Japanese population. J Arthroplasty 17:1028–1032
Westrich GH, Haas SB, Insall JN, Frachie A (1995) Resection specimen analysis of proximal tibial anatomy based on 100 total knee arthroplasty specimens. J Arthroplasty 10:47–51
Yoshioka Y, Siu DW, Scudamore RA, Cooke TD (1989) Tibial anatomy and functional axes. J Orthop Res 7:132–137
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Servien, E., Saffarini, M., Lustig, S. et al. Lateral versus medial tibial plateau: morphometric analysis and adaptability with current tibial component design. Knee Surg Sports Traumatol Arthr 16, 1141–1145 (2008). https://doi.org/10.1007/s00167-008-0620-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-008-0620-0