Abstract
Purpose
Assessment of repair integrity and clinical outcome after arthroscopic repair of rotator cuff tears in double-row suture-bridge technique with the use of a new knotless suture-anchor system.
Methods
The first treated 25 patients with arthroscopic rotator cuff repair in the suture-bridge technique using a novel knotless anchor and chain-link suture system were evaluated. Patients with isolated full-thickness supraspinatus tears were selected. They were followed clinically with functional scores (Constant score, ASES index), visual analog scale (VAS), and instrumentally with Isobex digital strength analyzer preoperatively, at 6 and 14 months postoperatively. The repair integrity was evaluated with MRI at an average of 14 months postoperatively.
Results
Significant improvement of pain, strength, range of motion, and functional scores occurred (P < 0.05). There was a re-tear rate of 20%. The subjective parameters (VAS and ASES Index) showed non-significant (n.s.) differences between the re-tear and intact repair groups, whereas the objective parameters (Constant score, muscle power and active ROM) showed significant differences between both groups (P < 0.05).
Conclusion
The functional outcome has improved significantly with this new knotless anchor-chain system and was more superior in shoulders with intact repair, whereas the resulted repair integrity was not better than other types of double-row repair techniques mentioned in the recent literature. However, this early report of the novel technique may show limited power for comparison due to the relatively small sample size.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several technical evolutions have recently occurred in arthroscopic rotator cuff repair. A controversial advance from single-row to double-row and recently to double-row suture-bridge repair took place. Suture-bridge technique was introduced to maximize the utility of the repair construct by using the suture limbs from the medial mattress suture to bridge and compress the repaired tendon to the bone using knotless suture anchors for lateral row fixation [3, 15].
Classic double-row repair of cuff tears, where each suture anchor is tied separately, is a technically demanding as well as time-consuming procedure especially if the operation is performed in elderly patients where anesthesia time is particularly considered. In addition, classic double-row repair technique was found to be biomechanically inferior to suture-bridge technique in terms of ultimate load, resistance to shear, and rotational forces as well as gap formation [5, 11, 21, 26]. Furthermore, the suture-bridge technique combines self-reinforcement, maximal compression on the cuff, and decreased operation time [2, 3, 5]. However, suture-bridge technique might lead to progressive tensile loading during fixation with elevated friction between suture and tendon and can eventually cause failure by suture cutout through the tendon. Another disadvantage is the possibility of suture slipping or pull-out of the anchor at the lateral row as seen in osteoporotic bone leading to weakness of the construct [3, 14].
Burkhart et al. [3] found in a biomechanical study that double-row rotator cuff repair with a new knotless SwiveLock-FiberChain system™ (Fig. 1) (Arthrex, Karlsfeld, Germany) had yield load, ultimate load, and cyclic displacement that were statistically equivalent to those of classic double-row repair. This suture-anchor system composed of flexible chain of woven FiberWire suture links captured via the bifurcated tip of the SwiveLock anchor. Advantages of this suture-anchor system include that the repaired tendon is spanned under a captured chain-link suture which possesses a self-reinforcing character, a hard stop that prevents slipping of the suture, and a large surface area relative to the ordinary suture in contact with the tendon [3].
To our knowledge, this suture-anchor system has not been reported in a clinical study up till now. Therefore, the purpose of the present study is to evaluate the repair integrity and clinical outcome of suture-bridge repair using this novel knotless suture-anchor system. Our hypothesis was that double-row rotator cuff repair in suture-bridge technique using this suture-anchor system yields clinical and structural results, which are comparable to other types of double-row repair techniques mentioned in the literature.
Materials and methods
Between 2007 and 2008, a consecutive series of 25 patients with isolated full-thickness supraspinatus (SSP) tear underwent arthroscopic repair. Two patients out of this series underwent partial reconstruction with margin convergence technique and in one patient the diagnosis of rheumatoid arthritis was established in the postoperative interval, so that they were excluded. Another two patients were lost to follow-up. Therefore, this study was conducted on 20 patients (follow-up rate 91%). The average follow-up was 14 months (range, 12–18 months, SD ± 4).
Our inclusion criteria were patients with symptomatic isolated full-thickness SSP-tears, failed to improve to initial conservative treatment (physiotherapy and analgesics). Findings were confirmed during surgery, and the tendon repair was performed with a complete reconstruction in double-row suture-bridge technique. There were no age or sex differences. Exclusion criteria were combined tendon tears (subscapularis, infraspinatus or teres minor tears), partial-thickness SSP lesions, incomplete repair of the SSP, humeral head or glenoid fracture, patients with shoulder instability, osteoarthritis of the shoulder, rheumatoid arthritis, recurrent rotator cuff tears or previous surgery on the rotator cuff and cuff arthropathy.
The average age was 58 years (range, 46–65, SD ± 8) at the time of surgery. There were 10 women and 10 men, 17 right and 3 left shoulders. The dominant shoulder was affected in 18 patients. According to medical history given by the patients, the cause of rotator cuff tear was degenerative in 12 and traumatic in 8 patients. In traumatic cases, the average period between trauma and surgery was 3.5 months (range, 0.5–8.0 months, SD ± 4.3). In degenerative tears, the average time lag between the start of complaints and presentation was 8.0 months (range, 3.0–15.0 months, SD ± 7.0).
Using the classification of Snyder et al. [25], there were 2 patients with C1 tear, 9 patients with C2 tear, 6 patients with C3 tear, and 3 patients with C4 tear. Regarding the acromion type according to Bigliani [1], there were 7 patients (35%) with acromion type III, 9 patients (45%) with type II, and 4 patients (20%) with type I.
The patients were assessed clinically including functional tests, scores, and instrumental strength measurement using Isobex digital analyzer (Medical Device Solutions, Burgdorf, Germany). Clinical evaluation was done preoperatively, at 6 weeks, 3, 6, and at least 12 months, postoperatively. The structural integrity of SSP was examined by MRI preoperatively and again at least 12 months, postoperatively.
The medical history of the patients was reported through a prepared patient questionnaire including pain during activity and nocturnal pain, quantification of pain using the visual analog scale (VAS) and pain medication, sports activity and return to sports after surgery, and the degree of subjective satisfaction.
The patients were examined for the range of motion (ROM), where the ranges of passive and active movements of the shoulder (flexion, extension, abduction, low external and internal rotation) were recorded with a goniometer while the patient was standing and the thumb directed forward. The shoulder was manually fixed during examination according to Codman [4]. The strength of flexion and abduction (extended elbow) as well as external and internal rotation (90° flexed elbow) was recorded using manual muscle testing (grade 0 to V). The strength of the SSP was measured with Isobex strength analyzer in 90° abduction, bilaterally performed for comparison preoperatively, 6 and 12 months postoperatively. In addition, functional tests and scores, Constant score [6] and American Shoulder and Elbow surgeon index (ASES) [23], were performed. A single experienced examiner performed these measurements to avoid an inter-observer variability.
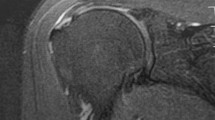
Assessment of MRIs was done by one experienced radiologist specialized in musculoskeletal radiology, who was blinded for the clinical picture of the patients, preoperatively and at follow-up. MRIs were performed in axial, coronal, and sagittal views in T1- and T2-weighted image sequences. Rotator cuff tears were identified on an oblique coronal T2-weighted non-fat-saturation image, as this provides the sharpest margins and therefore the most accurate measurement. The standard criterion for the identification of isolated full-thickness SSP-tear preoperatively or at follow-up was high-signal intensity (fluid-filled) gap in the low-signal intensity tendon on T2-weighted images. Analysis of the SSP-tear was performed. Retraction of SSP-tendon was classified according Patte [22], fatty degeneration according to Fuchs et al. [8], supraspinatus atrophy according to Thomazeau et al. [28], and Tangent sign according to Zanetti et al. [29], both preoperatively and at follow-up.
Surgical technique
All patients were operated by the senior author. Initial diagnostic arthroscopy was performed under general anesthesia in beach-chair-position for assessment of the tear and shoulder joint. Subacromial soft-tissue decompression was performed for all patients. In 7 patients with acromion type III, additional acromioplasty was performed. After tendon mobilization according to its mobility, the footprint was debrided.
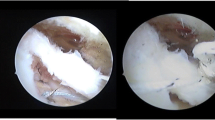
For the medial row, Bio-Corkscrew FT suture anchors (Arthrex) preloaded with FiberChain were inserted at the medial edge of the footprint. A suture passing instrument (Scorpion, Arthrex) was used for passing the FiberWire leader through the SSP-tendon, 2–3 mm lateral to the musculotendinous junction, followed by the FiberChain. A lateral row was placed after preparing bone sockets just lateral to the free edge of SSP-tendon. The FiberChain was brought under tension and then the SwiveLock anchor with its forked tip captures the second chain link from the lateral edge of the tendon and drives it to the bottom of the bone socket, so that the FiberChain spans itself over the tendon (Figs. 2, 3a–d). Successive anchors were inserted similarly according to the size of the defect [3].
Intra-operative photographs showing: a The SwiveLock anchor while trying to capture the FiberChain with its bifurcated tip. b SwiveLock holds the FiberChain and introduces it into the bottom of the prepared bone socket. c Driving the SwiveLock with the captured FiberChain in the prepared bone socket. d The tensioned FiberChain extends over and holds the supraspinatus tendon on the footprint
All cases were accompanied by pathology of the long head of biceps, either subluxation in 12 (60%) or tendinitis in 8 (40%) shoulders. They were treated by suture-tenodesis in loop technique using titanium anchors (FT2 Corkscrew, Arthrex).
Postoperative protocol
A shoulder-immobilizing abduction pillow (MEDI® SAK) (Medi, Bayreuth, Germany) was applied in 30° abduction for 4–6 weeks postoperatively. The patient was encouraged to perform a planned physiotherapy program; in the first 3 weeks, the shoulder was mobilized passively to 60–90° flexion/abduction and in the next 3 weeks actively, starting with active-assisted to light active exercises. Free-range of active exercises were allowed from the 7th week and light sport activities after 3 months.
Statistical analysis
Statistical analyses were performed using the software package SPSS (Version 15, SPSS Inc, Chicago, Illinois). Statistical significance was evaluated for the functional scores between the preoperative and postoperative measurements using Student’s two-tailed t-test for continuous data. A p-value <0.05 was considered to indicate statistical significance. One-factor analysis of variance was used to compare the groups of repair and the functional scores. Descriptive results were displayed as mean ± SD (standard deviation).
Results
Clinical outcome of the total patient population is presented in Tables 1 and 2. Regarding repair integrity assessed with MRI, there were 16 shoulders (80%) with intact repair and 4 shoulders (20%) with re-tear.
At final follow-up, there were 12 patients (60%) free of pain, 8 (40%) patients with occasional pain, and nocturnal pain was reported by 5 patients (25%). Twelve patients (60%) returned to their preoperative level of sports and 8 patients (40%) reduced their level or changed the type of sports, but no patient was incapable to practice sport activities again. No patient received pain medication any more. Nine patients (45%) were highly satisfied and 11 patients (55%) were satisfied.
The relation between the re-tear and preoperative size as well as the relation between the re-tear and cause of tear are presented in Table 3. Differential analysis of the clinical parameters at final follow-up is shown in Tables 4 and 5. Active ROM in both repair groups at final follow-up is presented in Table 5.
At final follow-up, 9 patients (56%) were pain free and 7 patients (44%) were still having occasional shoulder pain in the intact repair group, whereas 3 (75%) patients were pain free and 1 patient with occasional shoulder pain (25%) in the group of re-tears. Nine patients (56%) were able to perform their sports activity similar to the preoperative level and 7 patient (44%) reduced or changed their sports activities in the intact repair group, whereas in the group of re-tear the values were 3 (75%) and 1 (25%), respectively. Nine patients (56%) were highly satisfied and 7 patients (44%) were satisfied in the group of intact repair, whereas all patients in the group of re-tear were satisfied.
Analysis of MRIs preoperatively and postoperatively is presented in Table 6.
There were no intraoperative or perioperative complications. One patient developed a secondary frozen shoulder 3 months postoperatively, which was successfully conservatively treated with oral prednisolone for 4 weeks and physiotherapy. No patient suffered from wound infection, neurovascular injury, and suture-anchor displacement, and no revision surgery was indicated.
Discussion
The most important finding of this study was a significant improvement of the clinical outcome with this novel arthroscopic double-row suture-bridge rotator cuff repair, confirming the first part of our hypothesis. However, the improvement in the subjective evaluation of patients including pain, subjective satisfaction, passive motion, and function during daily activities was non-significant between both groups of repair (Tables 4, 5). Therefore, we conclude that with patient questionnaire alone a re-tear cannot be predicted. This observation is supported by the work of Harryman [12] and Rockwood [24], where subacromial decompression, denervation, and an attempted repair of the cuff even with a re-tear had yielded good functional results. Whereas the objective evaluation of the shoulder regarding muscle power testing and active ROM showed significant differences between shoulders with intact repair and re-tear (Tables 4, 5).
The significant difference in active ROM and muscle strength between intact repair and re-tear patients may be explained by an improvement in centering of the humeral head with intact repair and consequently improvement of load transmission, joint kinematics, and muscle power. Similar clinical results were obtained by Sugaya et al. [27] and Huijsmans et al. [13].
In the present study, the functional scores improved significantly from preoperative to postoperative follow-up. Similar reports of significant functional improvement following arthroscopic double-row repair of rotator cuff tears were published by Sugaya et al. [27], where ASES index improved from 42 to 94 points and by Nho et al. [19] from 51 to 93 points. Similarly, Constant score improved in the study of Lafosse et al. [17] from 43 to 80 points.
Although some studies have not shown a relationship between repair integrity and functional results [16, 18], our results correlate with the findings of studies, where significantly better results were reported in patients with intact repair [12, 13, 27]. Therefore, we believe that achieving a complete healing of the rotator cuff is necessary for a favorable outcome. However, the comparison between the 2 groups in this study lacks the statistical power because of the small sample size.
There was a re-tear rate of 20% in our series. Explanation of re-tear in the presence of this biomechanically strong construct could be a reflection of the age as 70% of our patients were over 60 years old, this can consequently be a reason for reduced healing power and quality of tissue. In addition, the effect of excessive mobilization of the retracted tendon on the viability of the tendon tissue or additional new tearing of the degenerated tissue of the rotator cuff has to be discussed [12].
The second part of our hypothesis was not confirmed, as the re-tear rate was slightly higher than mentioned in the current literature [13, 17, 20, 27]. A re-tear rate after arthroscopic classic double-row repair found to be 17% by Sugaya et al. [27] after 14 months diagnosed by MRI and also 17% found by Hujismans et al. [13] after 12 months diagnosed by ultrasonography.
In comparison with other fixation systems of the rotator cuff in the suture-bridge technique, Park et al. found a re-tear rate of 9% after 12 months diagnosed by ultrasonography using push-lock device and FiberWire suture (Arthrex) for lateral row fixation [20]. Frank et al. found a re-tear rate of 12% after one year diagnosed by MRI using Bio-Tenodesis screw in some cases and push-lock device in other cases for lateral row fixation [7]. Consequently, this novel SwiveLock-FiberChain system was less favorable than others in reducing the re-tear rate. However, a solid conclusion could not be reached due to the relatively small sample size.
Burkhart et al. [3] postulated that SwiveLock-FiberChain system results in combination of self-reinforcement, knotless management, and decreased operation time. The self-reinforcing character is particularly useful in poor-quality tendon as it strengthens the construct. Regarding the ease and speed of suture management, the knotless character of this novel system allows saving time and effort required for each arthroscopic knot with multiple suture anchors, therefore, definitely reduces operation steps and may be the operation time [2]. Unfortunately, this observation was not confirmed with our data, as we could not record and compare the duration of SSP-repair from the overall operation time in our series because of technical difficulties in selective time measurement. Notably, variations in the duration of subacromial decompression, associated pathology of long head of biceps, and the time required for tendon mobilization can influence the overall operation time.
MRI analysis showed a progression of atrophy and fatty degeneration in the supraspinatus muscle in the re-tear group, whereas in shoulders with intact repair muscle atrophy improved and no further progression of fatty infiltration occurred (Table 4). These findings correspond to those of Gerber et al. [9] who found that, successful cuff repair can moderately improve the degree of muscle atrophy and arrest further fatty infiltration. Therefore, we may conclude superior structural properties of rotator cuff muscles are associated with intact repair.
Concerning MRI examination, arthro-MRI would have been useful for a higher diagnostic accuracy instead of native MRI for the evaluation of rotator cuff tears. Indeed, beside the refusal of our patients an intra-articular injection of contrast material, it was not permitted from the responsible ethics commission.
In this series, all cases were accompanied with pathology of the long head of biceps and managed by arthroscopic tenodesis. This could be a source of complaint preoperatively or postoperatively and interfere with the complaint due to SSP-tear or re-tear; therefore, it can affect the overall clinical outcome, biasing the results.
To reduce bias in this study, a single experienced examiner for the clinical parameters, a single specialist for musculo-skeletal radiology, and a single highly experienced surgeon in arthroscopic shoulder surgery were recruited.
One female patient developed a secondary frozen shoulder 3 months postoperatively. At the scheduled three month follow-up, she was presented with a marked limitation of ROM (flexion/abduction 40°, internal rotation 30°, external rotation 10°). She was successfully conservatively treated with oral prednisolone over 4 weeks followed by intensive physiotherapy. At the 6 months follow-up, she showed a significant improvement of shoulder motion (flexion 115°, abduction 110°, internal rotation 90°, and external rotation 55°). This patient showed intact repair later on.
Weaknesses in this study include the overall small sample size, which can predispose to type II errors in our statistical analysis. The short-term follow-up may also influence results, in particular the clinical outcomes. However, according to Goutallier et al., we do not expect a re-tear of the rotator cuff to occur later than 14 months postoperatively [10]. Another limitation of this study was the small number of failures; therefore, comparisons between both groups of repair regarding functional results cannot yield a powerful conclusion.
However, a powerful issue in this study is the selection of isolated SSP-tears, as most of the studies present the outcome of rotator cuff repair with multiple tendon involvement, which may lead to a bias of their results.
For clinical relevance, the importance of intact repair for a favorable outcome and avoidance of increasing atrophy and fatty infiltration was confirmed. Although this study shows a tendency for a lower healing rate with this technique in comparison with other techniques of suture-bridge repair, the biomechanical evidence of its superiority as well as its theoretical advantages [3] encourage us to continue with this technique for a larger sample size in a longer follow-up in order to obtain a solid conclusion. We believe that this knotless anchor and chain-link technique provides an excellent initial strength as well as compression applied over the footprint of the cuff with an increased contact area and higher healing potential.
Conclusion
This study contributes to the evaluation of repair integrity after rotator cuff arthroscopic repair. The clinical outcome has improved significantly with this new chain-link suture and knotless anchor system and was more superior in shoulders with intact repair, whereas the resulted repair integrity was not better than other types of double-row repair techniques mentioned in the recent literature. However, in this early report of a new technique, a powerful conclusion could not be reached due to the relatively small sample size.
References
Bigliani LU, Morrison DS (1986) The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans 10:228–234
Burkhart SS, Cole BJ (2010) Bridging self-reinforcing double-row rotator cuff repair: we really are doing better. Arthroscopy 26:677–680
Burkhart SS, Adams CR, Schoolfield JD (2009) A biomechanical comparison of 2 techniques of footprint reconstruction for rotator cuff repair: the SwiveLock-FiberChain construct versus standard double-row repair. Arthroscopy 25:274–281
Codman AE (1934) The shoulder: rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. Todd, Boston
Cole BJ, ElAttrache NS, Anbari A (2007) Arthroscopic rotator cuff repairs: an anatomic and biomechanical rationale for different suture-anchor repair configurations. Arthroscopy 23:662–669
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Frank JB, ElAttrache NS, Dines JS, Blackburn A, Crues J, Tibone JE (2008) Repair site integrity after arthroscopic transosseous-equivalent suture-bridge rotator cuff repair. Am J Sports Med 36:1496–1503
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C (1999) Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Should Elbow Surg 8:599–605
Gerber C, Schneeberger AG, Hoppeler H, Meyer DC (2007) Correlation of atrophy and fatty infiltration on strength and integrity of rotator cuff repairs: a study in thirteen patients. J Should Elbow Surg 16:691–696
Goutallier D, Postel JM, Radier C, Bernageau J, Zilber S (2009) Long-term functional and structural outcome in patients with intact repairs 1 year after open transosseous rotator cuff repair. J Should Elbow Surg 18:521–528
Grimberg J, Diop A, Kalra K, Charousset C, Duranthon LD, Maurel N (2010) In vitro biomechanical comparison of three different types of single- and double-row arthroscopic rotator cuff repairs: Analysis of continuous bone-tendon contact pressure and surface during different simulated joint positions. J Should Elbow Surg 19:236–243
Harryman DT II, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA (1991) Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am 73:982–989
Huijsmans PE, Pritchard MP, Berghs BM, van Rooyen KS, Wallace AL, de Beer JF (2007) Arthroscopic rotator cuff repair with double-row fixation. J Bone Joint Surg Am 89:1248–1257
Kim KC, Rhee KJ, Shin HD (2009) Revision of a pull-out suture anchor in the lateral row during the suture-bridge technique: technical note. Knee Surg Sports Traumatol Arthrosc 17:1463–1465
Kim KC, Rhee KJ, Shin HD, Kim PS (2009) Arthroscopic footprint reconstruction of bursal-side delaminated rotator cuff tears using the suture-bridge technique. Knee Surg Sports Traumatol Arthrosc 17:840–843
Klepps S, Bishop J, Lin J, Strauss A, Hayes P, Flatow EL (2004) Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med 32:1716–1722
Lafosse L, Brozska R, Toussaint B, Gobezie R (2007) The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Bone Joint Surg Am 89:1533–1541
Liu SH, Baker CL (1994) Arthroscopically assisted rotator cuff repair: correlation of functional results with integrity of the cuff. Arthroscopy 10:54–60
Nho SJ, Adler RS, Tomlinson DP et al (2009) Arthroscopic rotator cuff repair: prospective evaluation with sequential ultrasonography. Am J Sports Med 37:1938–1945
Park JY, Siti HT, Keum JS, Moon SG, Oh KS (2009) Does an Arthroscopic Suture Bridge Technique Maintain Repair Integrity?: A Serial Evaluation by Ultrasonography. Clin Orthop Relat Res. 468(6):1578–1587
Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun BJ, Lee TQ (2007) Part I: footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Should Elbow Surg 16:461–468
Patte D (1990) Classification of rotator cuff lesions. Clin Orthop Relat Res. 254:81–86
Richards RRBL, Friedman RJ, Gartsman GM, Lannotti JP (1994) A standardaized method for assessment of shoulder function. J Should Elbow Surg 3:347–352
Rockwood CABW (1988) Management of patients with massive rotator cuff defects by acromioplasty and rotator cuff debridement. Orthop Trans. 12:190–199
Snyder SJ (1993) Evaluation and treatment of the rotator cuff. Orthop Clin North Am 24:173–192
Spang JT, Buchmann S, Brucker PU, Kouloumentas P, Obst T, Imhoff AB (2009) A biomechanical comparison of 2 transosseous-equivalent double-row rotator cuff repair techniques using bioabsorbable anchors: cyclic loading and failure behavior. Arthroscopy 25:872–879
Sugaya H, Maeda K, Matsuki K, Moriishi J (2007) Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am 89:953–960
Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F (1996) Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand 67:264–268
Zanetti M, Gerber C, Hodler J (1998) Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol 33:163–170
Acknowledgments
We thank Bettina Brenner for her great help in acquiring patients and collecting clinical data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Azab, H., Buchmann, S., Beitzel, K. et al. Clinical and structural evaluation of arthroscopic double-row suture-bridge rotator cuff repair: early results of a novel technique. Knee Surg Sports Traumatol Arthrosc 18, 1730–1737 (2010). https://doi.org/10.1007/s00167-010-1257-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-010-1257-3