Abstract
Biomechanical studies suggest a suture bridge technique enhances rotator cuff tendon footprint contact area, holding strength, and mean contact pressure. Based on these studies, we asked whether (1) the suture bridge technique would provide a high rate of cuff integrity after surgery, (2) the status of the repaired cuff would change with time, (3) preoperative factors could predict postoperative cuff integrity, and (4) patients with retears had less favorable pain, functional scores, range of motion (ROM), and muscle strength compared with those with intact repairs. We prospectively followed 78 patients with arthroscopic repairs in whom we used the suture bridge technique. The integrity of the rotator cuff repair was determined using ultrasonographic evaluation at 4.5 and 12 months after surgery. Ultrasonography revealed intact cuffs in 91% at 4.5 months postoperatively, all of which were maintained at the 12-month followup. Failure rates were 17.6% (three of 17) for massive tears, 11.1% (two of 18) for large tears, 6.3% (two of 32) for medium tears, and no failures for small tears. Preoperative fatty degeneration of the supraspinatus muscle was a strong predictor of cuff integrity. We found no correlation between the integrity and clinical outcomes except for a temporary decrease of abduction strength at 6 months. Arthroscopic repair using suture bridge technique can achieve a low retear rate in shoulders treated for rotator cuff tears, but the occurrence of retear did not influence the outcome.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Arthroscopic rotator cuff repairs have gained popularity owing to rapid improvement in the techniques and instrumentations and reportedly provide satisfactory clinical outcomes [5, 15, 31]. However, persistent retear remains one of the most common complications after rotator cuff repair [2, 10, 21, 34]. The standard single-row arthroscopic rotator cuff repair reportedly is unsuccessful in restoring footprint contact area [3, 4, 17]. This has led to the development of more secure fixation methods.
Experimental evidence suggests the holding strength of the repair technique plays an important role in the prevention of retear [30]. Based on biomechanical studies, a suture bridge rotator cuff repair technique has been suggested as one of the effective alternatives that can enhance rotator cuff tendon footprint contact area and reduce mean pressure, while retaining strength [28, 29]. The suture bridge technique has an advantage over traditional double-row repair as it uses the suture limbs from the medial suture knots to bridge and compress the repaired tendon, and therefore reduces the surgical steps. Frank et al. [9], in a study of 25 patients, reported 88% (22 of 25 patients) with cuff integrity after arthroscopic repair using suture bridge technique assessed by MRI at 1 year.
We performed this study to determine whether (1) the suture bridge technique would provide a high rate of cuff integrity after surgery, (2) the status of the repaired cuff would change with time, (3) preoperative factors could predict postoperative cuff integrity, and (4) patients with retears had less favorable pain, functional scores, range of motion (ROM), and muscle strength compared with those with intact repairs.
Materials and Methods
We prospectively followed all 99 patients treated with arthroscopic rotator cuff repair using the suture bridge technique from July 2006 to September 2007. We included patients with the following: (1) diagnosis of full-thickness rotator cuff tear with physical examination and with MRI; (2) failure of nonoperative treatment (medication and strengthening of rotator cuff, deltoid, and scapular stabilizer); and (3) no previous history of fractures or operations around the shoulder. We excluded patients with the following: (1) arthritic changes of the glenohumeral joint on radiographs; (2) failure of arthroscopic repair using the suture bridge technique owing to severe retraction or poor quality of the torn rotator cuff; and (3) refusal to receive postoperative ultrasonography. We excluded 17 patients owing to the lack of followup. Four patients with massive rotator cuff tears were excluded in this study owing to irreparable defects. One patient had MRI performed 4.5 months postoperatively at an outside institution, which showed retear. Although he refused to undergo ultrasonographic examination at 12 months, we decided to include him in this study as his clinical features at 12 months were available and provided sufficient information regarding the status of the retear. The exclusions left 78 of the 99 patients (78 shoulders) for this study. There were 49 men and 29 women, and the average age was 59.2 years (range, 38–78 years) (Table 1). Fifty-seven patients underwent rotator cuff repair on the dominant shoulder. The interval from onset of symptoms to surgery ranged from 3 months to 10 years (mean, 29.8 months). Minimum followup was 12 months (mean, 13.1 months; range, 12–17 months). All patients had a complete clinical examination, preoperative MRI, and postoperative serial ultrasound examination at 4.5 and 12 months.
All operations were performed by the senior author (J-YP). The patients were placed in the beach chair position under general anesthesia. Four routine arthroscopic portals (anterior, posterior, lateral, posterolateral) were used to perform the rotator cuff repair. A posterior portal was established as the primary viewing portal. After the bursectomy was completed, arthroscopic subacromial decompression was performed to create a flat acromial undersurface in all patients. We then inspected the bursal side of the rotator cuff and débrided the margin of the tear to gain better quality of tendon tissues. If mobility of a tendon was insufficient for repair, procedures to mobilize the tendon, such as release of the coracohumeral ligament at the base of coracoid process and detachment of the rotator cuff from the bursal and articular sides, were performed. Tear size was measured at the time of surgery by the surgeon using a calibrated measuring device to obtain medial-to-lateral and anterior-to-posterior dimensions of the tear. We followed the rating system proposed by DeOrio and Cofield [7], which classifies a tear with a length smaller than 1 cm as a small tear, a tear 1 to 3 cm as medium, a tear 3 to 5 cm as large, and a tear greater than 5 cm as a massive tear. There were 17 massive, 18 large, 32 medium, and 11 small tears in this study. The footprint was thoroughly débrided of any soft tissue until bleeding occurred. To insert a suture anchor, we made a small incision just lateral to the acromion, named the suture anchor portal. The portal was placed on the extension line of the clavicle posterior border. A 5.0-mm Bio-Corkscrew™ suture anchor (Arthrex, Naples, FL) was inserted at the junction of the articular cartilage and the medial aspect of the footprint on the greater tuberosity. Sutures were passed through the tendon in a mattress fashion. In small- to medium-sized rotator cuff tears, so as to restore the footprint of the rotator cuff more anatomically, the suture hook should be inserted at the rotator cuff with an equal dimension of the footprint on the greater tuberosity, and it should come out just medial to the torn edge in the articular side. In cases involving a laminated rotator cuff, the repair was performed en masse by passing the suture through the whole cuff. The sutures then were tied with a sliding knot (SMC knot). Each suture limb from the medial row was placed through the hole at the end of the push-lock device (3.5-mm Bio-PushLock™; Arthrex). While viewing through the posterolateral portal, pilot holes for the push-lock device were created using a punch 2 cm distal to the lateral edge of the footprint via the lateral portal. While maintaining a constant tension, a push-lock device was inserted into the pilot hole. After the device was fully engaged in the pilot hole, the sutures were cut (Fig. 1).
(A) An arthroscopic view shows a massive rotator cuff tear involving the upper border of the subscapularis, supraspinatus, and infraspinatus, with medial retraction and subluxation of the long head of the biceps tendon. (B) An arthroscopic view from the lateral portal shows a completed repair of a massive rotator cuff tear with three suture anchors and three push-lock devices, resulting in 10 suture bridges.
Postoperatively, we prescribed a shoulder-immobilizing sling with abduction pillow to each patient with instructions to maintain the shoulder at 30° to 40° internal rotation and 20° abduction. The patients began gentle passive forward flexion on the first postoperative day. The time required for immobilization by the abduction pillow depended on the size of the tear, the quality of the cuff and bone tissue, and the security of the repair. For patients with small to medium tears, the sling with abduction pillow was removed 5 weeks postoperatively, and active ROM mobilization, including stick exercise, was started. Active resistance muscle strengthening exercises were started after 8 weeks using Thera-Band® (HCM-Hygenic Corp, Batu Gajah, Malaysia). For patients with large to massive tears, patients were allowed to start active ROM and stick exercises in 6 to 8 weeks, and external sling appliances were maintained until 8 weeks after surgery. Active resistance muscle strengthening exercises were allowed after 10 weeks. At 3 to 4 months after surgery, patients were permitted to do light activities. Sports activity and heavy labor were allowed after 6 months.
Clinical data were collected before the operation and postoperatively at 3 months, 6 months, and at final followup by two orthopaedic surgeons (K-SO, J-SK) not involved in the operations. Four outcome measures were used in this study: the visual analog scale (VAS) pain score, the American Shoulder and Elbow Surgeons (ASES) score, ROM, and muscle strength. The VAS pain score is a horizontal line, 10 cm in length, anchored by word descriptors “no pain” on the left side and “very severe pain” on the right side. The ASES score involves a score summation in a 100-point system (50 points for daily function, 50 points for pain). Muscle strength was measured with a portable myometer (Mecmesin Co, Nottingham, UK) at four times: before surgery, at 3 months, 6 months, and at final followup postoperatively. Evaluation of muscle strength was performed by one laboratory technician (J-SK). During the strength test, the participants were seated upright. The muscle strength of the supraspinatus was checked in the empty-can position. The strength of external rotators of the shoulder was checked in neutral abduction. These measurements were normalized to the opposite shoulder and reported as a ratio (shoulder strength index [SSI]) [26]. To ensure reliability, the muscle powers of both shoulders were evaluated consecutively.
Anteroposterior (AP) views of internal and external rotation and supraspinatus outlet views, axillary view, and Rockwood view [16] (30° caudally angled AP view) were obtained, and MRI of the affected shoulder was performed. We evaluated cuff muscle fatty degeneration preoperatively with MRI, using the five-stage grading system [12] and Global Fatty Degeneration Index (GFDI; mean value of three muscles) [13]: Grade 0, no fatty deposit; Grade 1, some fatty streaks; Grade 2, more muscle than fat; Grade 3, as much muscle as fat; and Grade 4, less muscle than fat. Fatty degeneration was graded by two orthopaedic surgeons (K-SO, HTS), and if necessary, a consensus was achieved with the help of a specialized radiologist (S-GM). For observer reliability using the system of Goutallier et al. [12, 13], the interclass correlation coefficient has been reported to range from 0.58 to 0.78, which was higher for radiologists than for orthopaedic surgeons [24]. In our study, the interclass correlation coefficients for grading fatty degeneration were 0.71 for supraspinatus, 0.68 for infraspinatus, and 0.65 for subscapularis muscle.
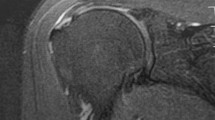
The integrity of the rotator cuff repair was determined by ultrasonographic evaluation (Fig. 2). All patients had postoperative ultrasonographic examination at 4.5 and 12 months. One specialized radiologist (S-GM) with 10 years of experience with musculoskeletal ultrasonography performed all followup examinations using an HDI 5000 system or an IU-22 system (both from Philips Healthcare, Bothell, WA). The sonographic evaluation of the rotator cuff was performed according to a standard protocol [22]. The ultrasound criteria for the diagnosis of full-thickness rotator cuff tears were as follows [6, 35]: (1) nonobservation of the supraspinatus tendon attributable to retraction under the acromioclavicular joint; (2) localized absence or focal discontinuity of the cuff with consecutive loss of the normal anterior arc of the subdeltoid bursa; (3) loss of normal supraspinatus substance with widening of the gap between the supraspinatus and biceps tendon and exposure of a bare area of bone and cartilage; (4) a hypoechoic or anechoic cleft extending through the entire substance of the cuff; and (5) coexistence of fluid in the subacromial subdeltoid bursa and/or the presence of fluid in the sheath of the long head of biceps tendon. Partial-thickness tears were diagnosed when a focal hypoechoic or anechoic defect existed in the tendon, involving either the bursal or the articular surface and manifested in two perpendicular planes [35].
(A) Ultrasonography shows failed repair of the supraspinatus tendon with multiple droplets (black arrow) in the rotator cuff defect. A long-axis view shows medial retraction of the supraspinatus (SS) tendon (white arrows). (B) The anterior-to-posterior dimension of the retear is noted on the short-axis view with the shadow of the inserted suture anchors (white arrows) observed on the humeral head (HH). The posterior part of the remaining tendon is also noted (black arrows). D = deltoid muscle; GT = greater tuberosity.
Measurements are expressed as mean ± standard deviation. The unpaired t test and Mann-Whitney U test were used to compare the average of the measurements between intact and retorn cuffs. Bivariate analysis (Pearson correlation coefficient for continuous data, Spearman correlation coefficient for categorical data) was used to determine the correlation of cuff integrity to age, duration of symptoms, preoperative tear size, retraction, and muscle fatty degeneration. Multiple regression analysis was used to determine the independent variables affecting outcomes. Statistical analysis was performed using SPSS® software (Version 13.0; SPSS Inc, Chicago, IL).
Results
Ultrasonography revealed intact cuffs in 71 of the 78 patients (91%) 4.5 months postoperatively; all repairs were maintained at the 12-month followup. Failure rates were 18% (three of 17) for massive tears, 11% (two of 18) for large tears, 6% (two of 32) for medium tears, and no failures for small tears.
In six patients with retears, serial ultrasound examinations revealed the tear sizes remained unchanged. The average anterior-to-posterior tear dimension was 2.5 cm (range, 0.8–3.5 cm) and the average medial-to-lateral tear dimension was 2.4 cm (range, 1.1–4 cm) (Table 2). Compared with preoperative tear dimensions, all but one patient with failed results had smaller cuff defects. The patient with increased tear size showed poor quality of the torn tendon edge at the time of the operation.
The postoperative cuff integrity correlated with preoperative fatty degeneration of the supraspinatus muscle (r = 0.365, p = 0.001) and preoperative retraction status of the cuff (Spearman coefficient = 0.303, p = 0.01). We observed no correlation (r = 0.122, p = 0.287) between the cuff integrity and fatty degeneration of the infraspinatus muscle. A correlation (r = −0.263, p = 0.050) was seen between the cuff integrity and preoperative tear size. In multiple regression analysis, preoperative fatty degeneration of the supraspinatus muscle predicted (p = 0.007) the integrity of the repaired cuff. Only abduction power correlated with preoperative structural factors, which included fatty degeneration of the supraspinatus and infraspinatus muscles, GFDI, tear size, and retraction of the cuff (Table 3). Preoperative clinical factors such as age, gender, dominance, and symptom duration did not correlate with postoperative functional outcomes. After fitting stepwise linear regression, fatty degeneration of the supraspinatus muscle (p = 0.050), infraspinatus muscle (p = 0.050), and GFDI (p = 0.027) remained associated with abduction power.
Compared with patients with retears, those with intact cuffs did not show any differences in postoperative clinical evaluations except abduction power at the 6-month followup (Table 4).
Discussion
For durability of rotator cuff repair, the process of reattaching the torn cuff to a larger contact area of the original footprint has been proposed [21]. Double-row repair is one of the methods developed to achieve better bone-tendon contact area and superior mechanical properties, such as lesser cyclic displacement, gap formation, and higher failure load [17, 23]. However, potential disadvantages are that it is technically demanding and time-consuming. The suture bridge technique was first described by Park et al. [27] to overcome the disadvantages of double-row repair and to have similar mechanical properties to the transosseous repair technique. The distinct advantages of this technique include improvement of the pressurized contact area and mean footprint pressure, which may result in maximizing healing potential between the tendon and the tuberosity [28, 29]. Although biomechanical data showed promising outcomes, only one clinical study has confirmed its advantages in healing. Frank et al. [9] conducted a retrospective study of cuff integrity after suture bridge rotator cuff repair and reported a high healing rate, 88%, on MRI at 1-year followup. However, only 25 cases, including three cases of massive tears, were evaluated in that study. We therefore asked whether (1) the suture bridge technique would provide a high rate of cuff integrity after surgery, (2) the status of the repaired cuff would change with time, (3) preoperative factors could predict postoperative cuff integrity, and (4) patients with retears had less favorable pain, functional scores, ROM, and muscle strength compared with those with intact repairs.
Several limitations to our study warrant review. First, the number of retears was small and the followup was relatively short, which may lead to failure of differentiation between intact cuffs and retears. Second, although all patients were evaluated serially using ultrasonography by an experienced musculoskeletal radiologist, this modality is examiner-dependent. Fotiadou et al. [8], in a recent study investigating the accuracy of ultrasonography for detection of rotator cuff tears, reported the accuracy of ultrasonography was as much as 98% for full-thickness tears and 87% for partial-thickness tears, which were comparable to the MRI results of 100% and 90% for full-thickness and partial-thickness tears, respectively. Although some authors reported high accuracy of a surgeon interpreting office-based ultrasonography, we did not perform ultrasound examination by ourselves to avoid surgeon’s prejudice [1, 36]. Third, large to massive tears in 13 patients were not included in this study owing to the lack of followup. Considering the relatively high failure rate in the large to massive tears, there is the possibility of a higher retear rate than that found in our study. The dropout rate for patients with large to massive tears was 27% (13 of 48 patients). Of the 13 patients, three underwent the 4.5-month followup ultrasound examination, which showed intact cuff integrity. One reason for this high rate of followup loss is that elderly patients living in rural areas with larger tears (average age of these patients, 63 years) were reluctant to revisit the clinic for postoperative evaluation. Fourth, we intended to see early fixation failure of repaired cuffs by evaluating shoulders at 4.5 months postoperatively. However, the healing process is in progress during this period. This makes it difficult to determine whether the defects seen are the result of initial fixation failure or incomplete healing.
Reported failure rates after arthroscopic cuff repair have varied (Table 5). Sugaya et al. [32] reported a failure rate of 40% for large to massive tears using double-row repair. Lafosse et al. [20] reported the overall retear rate of large to massive tears as 17%. Huijsmans et al. [14] stated the failure rate of cuff repairs of large to massive tears using the double-row technique, as confirmed by ultrasonography, was 36%. In cases of chronic large to massive tears, reattaching the lateral-most aspect of the rotator cuff tendon to the footprint is technically difficult and time-consuming owing to the poor tissue quality or severe retraction. Especially with double-row repair, the fastening procedure for the lateral edge of the compromised tendon is difficult and sometimes the tissue may be torn out. Furthermore, some authors indicated arthroscopic rotator cuff repair may not yield as strong of a repair as a traditional open or mini-open technique [10]. However, in our experience using the suture bridge technique as described by Park et al. [27], it is more convenient to firmly fasten the compromised tendon to the footprint using the suture limbs from medial suture knots, which is one of the advantages over double-row repair. We believe this technical aspect may have contributed to the encouraging results of cuff integrity for large to massive tears. Recently, Park et al. [28, 29] performed two serial laboratory studies to compare pressurized contact area, mean pressure at footprint, and initial biomechanical properties between the suture bridge and double-row techniques. The mean pressurized contact area between the tendon and tuberosity insertion footprint amounted to 77.6% footprint coverage with the suture bridge technique, which was superior to that of the double-row technique (39.6%). The suture bridge technique had greater ultimate-to-load failure and less gap formation than the double-row technique. The biomechanical superiority of the suture bridge technique may contribute partly to the low structural failure of the repaired cuff.
Preoperative fatty degeneration measured by MRI is reportedly a predictor of structural failure after rotator cuff repair [19, 33]. Thomazeau et al. [33] reported the rate of retearing dramatically increased when supraspinatus atrophy was exacerbated, which is in accordance with our finding. However, this correlation has not been proven in every study. Some authors suggest fatty degeneration of the infraspinatus muscle is a strong predictor for cuff integrity rather than that of the supraspinatus muscle [12, 25]. One reason for this inconsistency is attributable to the small patient population, especially the numbers with retears, included in each study. Moreover, it is not easy to remove the bias in determining the grade of fatty degeneration on MRI, even though most studies tried to achieve consensus by two or more doctors. Sugaya et al. [32] noted the approximation of a retracted rotator cuff in the presence of Grade 3 or 4 fatty degeneration was difficult. In their opinion, preoperative fatty degeneration was a key point in patient selection for arthroscopic rotator cuff repair. Although agreement exists regarding the effect of the fatty degeneration on postoperative cuff integrity, there is discrepancy in specific details regarding the effect of fatty degeneration grades. Actually, we had only one case of failure among the 16 with Grade 3 fatty degeneration, which was considerably lower than those with Grade 4 fatty degeneration. From our experience with the suture bridge technique, the cuff healing rate is better than with conventional fixation methods, even with the poor quality of the tendon associated with high-grade fatty degeneration of cuff muscles.
There is debate regarding the effects of cuff integrity on functional outcomes. Anderson et al. [2] reported a high correlation between cuff integrity and increased muscle strength in elevation and external rotation. However, in another prospective study, the integrity of the repair did not have any influence on the functional outcomes including muscle strength [18]. Even though the relation between these two important factors, cuff integrity and functional outcomes, has not been clearly identified, the deterioration of cuff muscle after retear should not be ignored. Gladstone et al. [11] investigated the progression of fatty infiltration in patients with rotator cuff repairs and found a successful repair did not lead to improvement or reversal of muscle degeneration and a failed repair resulted in substantial progression. They suggested rotator cuff repairs should be performed before more substantial deterioration in the cuff musculature occurs to optimize outcomes.
Arthroscopic repair with use of the suture bridge technique can achieve a low retear rate in shoulders treated for rotator cuff tears. Serial ultrasound examination showed cuff integrity in 91% of patients, a higher rate than in the previously reported repair series including the double-row methods. A high degree of fatty infiltration of the supraspinatus in the preoperative state was associated with a high occurrence of retear after rotator cuff repair.
References
Al-Shawi A, Badge R, Bunker T. The detection of full thickness rotator cuff tears using ultrasound. J Bone Joint Surg Br. 2008;90:889–892.
Anderson K, Boothby M, Aschenbrener D, van Holsbeeck M. Outcome and structural integrity after arthroscopic rotator cuff repair using 2 rows of fixation: minimum 2-year follow-up. Am J Sports Med. 2006;34:1899–1905.
Apreleva M, Ozbaydar M, Fitzgibbons PG, Warner JJ. Rotator cuff tears: the effect of the reconstruction method on three-dimensional repair site area. Arthroscopy. 2002;18:519–526.
Baums MH, Spahn G, Steckel H, Fischer A, Schultz W, Klinger HM. Comparative evaluation of the tendon-bone interface contact pressure in different single- versus double-row suture anchor repair techniques. Knee Surg Sports Traumatol Arthrosc. 2009 March 21. [Epub ahead of print].
Bennett WF. Arthroscopic repair of full-thickness supraspinatus tears (small-to-medium): a prospective study with 2- to 4-year follow-up. Arthroscopy. 2003;19:249–256.
Bianchi S, Martinoli C, Abdelwahab IF. Ultrasound of tendon tears. Part 1: general considerations and upper extremity. Skeletal Radiol. 2005;34:500–512.
DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66:563–567.
Fotiadou AN, Vlychou M, Papadopoulos P, Karataglis DS, Palladas P, Fezoulidis IV. Ultrasonography of symptomatic rotator cuff tears compared with MR imaging and surgery. Eur J Radiol. 2008;68:174–179.
Frank JB, ElAttrache NS, Dines JS, Blackburn A, Crues J, Tibone JE. Repair site integrity after arthroscopic transosseous-equivalent suture-bridge rotator cuff repair. Am J Sports Med. 2008;36:1496–1503.
Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–224.
Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719–728.
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures: pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83.
Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12:550–554.
Huijsmans PE, Pritchard MP, Berghs BM, van Rooyen KS, Wallace AL, de Beer JF. Arthroscopic rotator cuff repair with double-row fixation. J Bone Joint Surg Am. 2007;89:1248–1257.
Jones CK, Savoie FH 3rd. Arthroscopic repair of large and massive rotator cuff tears. Arthroscopy. 2003;19:564–571.
Kilcoyne RF, Reddy PK, Lyons F, Rockwood CA Jr. Optimal plain film imaging of the shoulder impingement syndrome. AJR Am J Roentgenol. 1989;153:795–797.
Kim DH, Elattrache NS, Tibone JE, Jun BJ, DeLaMora SN, Kvitne RS, Lee TQ. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med. 2006;34:407–414.
Klepps S, Bishop J, Lin J, Cahlon O, Strauss A, Hayes P, Flatow EL. Prospective evaluation of the effect of rotator cuff integrity on the outcome of open rotator cuff repairs. Am J Sports Med. 2004;32:1716–1722.
Knudsen HB, Gelineck J, Sojbjerg JO, Olsen BS, Johannsen HV, Sneppen O. Functional and magnetic resonance imaging evaluation after single-tendon rotator cuff reconstruction. J Shoulder Elbow Surg. 1999;8:242–246.
Lafosse L, Brozska R, Toussaint B, Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Bone Joint Surg Am. 2007;89:1533–1541.
Lo IK, Burkhart SS. Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthroscopy. 2004;20:250–267.
McNally EG. Practical Musculoskeletal Ultrasound. Philadelphia, PA: Elsevier Churchill Livingstone; 2005.
Meier SW, Meier JD. The effect of double-row fixation on initial repair strength in rotator cuff repair: a biomechanical study. Arthroscopy. 2006;22:1168–1173.
Oh JH, Kim SH, Choi JA, Kim Y, Oh CH. Reliability of the grading system for fatty degeneration of rotator cuff muscles. Clin Orthop Relat Res. 2009 April 4. [Epub ahead of print].
Oh JH, Kim SH, Ji HM, Jo KH, Bin SW, Gong HS. Prognostic factors affecting anatomic outcome of rotator cuff repair and correlation with functional outcome. Arthroscopy. 2009;25:30–39.
Park JY, Lhee SH, Choi JH, Park HK, Yu JW, Seo JB. Comparison of the clinical outcomes of single- and double-row repairs in rotator cuff tears. Am J Sports Med. 2008;36:1310–1316.
Park MC, Elattrache NS, Ahmad CS, Tibone JE. “Transosseous-equivalent” rotator cuff repair technique. Arthroscopy. 2006;22:1360.e1–1360.e5.
Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun BJ, Lee TQ. Part I: Footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:461–468.
Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun BJ, Lee TQ. Part II: Biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:469–476.
Schneeberger AG, von Roll A, Kalberer F, Jacob HA, Gerber C. Mechanical strength of arthroscopic rotator cuff repair techniques: an in vitro study. J Bone Joint Surg Am. 2002;84:2152–2160.
Severud EL, Ruotolo C, Abbott DD, Nottage WM. All-arthroscopic versus mini-open rotator cuff repair: a long-term retrospective outcome comparison. Arthroscopy. 2003;19:234–238.
Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: a prospective outcome study. J Bone Joint Surg Am. 2007;89:953–960.
Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997;344:275–283.
Wilson F, Hinov V, Adams G. Arthroscopic repair of full-thickness tears of the rotator cuff: 2- to 14-year follow-up. Arthroscopy. 2002;18:136–144.
Yen CH, Chiou HJ, Chou YH, Hsu CC, Wu JJ, Ma HL, Chang CY. Six surgery-correlated sonographic signs for rotator cuff tears: emphasis on partial-thickness tear. Clin Imaging. 2004;28:69–76.
Ziegler DW. The use of in-office, orthopaedist-performed ultrasound of the shoulder to evaluate and manage rotator cuff disorders. J Shoulder Elbow Surg. 2004;13:291–297.
Acknowledgments
We thank Jin-Sung Kim, laboratory technician, for assistance with evaluation of muscle strength in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Konkuk University Hospital.
About this article
Cite this article
Park, JY., Siti, H.T., Keum, JS. et al. Does an Arthroscopic Suture Bridge Technique Maintain Repair Integrity?: A Serial Evaluation by Ultrasonography. Clin Orthop Relat Res 468, 1578–1587 (2010). https://doi.org/10.1007/s11999-009-0990-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-0990-8