Abstract
Increased patellofemoral contact pressure was described after total knee arthroplasty (TKA). Aim of this in vitro study was to compare the influence of a posterior stabilized (PS) design in comparison to a cruciate retaining (CR) design on patellofemoral contact pressure. Patellofemoral area contact pressure, peak contact pressure and the centre of pressure motion were determined in eight fresh frozen human cadaveric specimens using a Tekscan sensor (K-Scan 4000). A robotic knee simulator was used simulating an isokinetic knee extension cycle from 120° of flexion to full extension. All knees were tested in a first test cycle after implantation of a CR design and in a second test cycle after replacement by a PS design, both using a 11 mm PE inlay (Genesis II, Smith & Nephew, Memphis, TN, USA). The patella remained unresurfaced. A paired sampled t test to compare mean values (significance, P ≤ 0.05) was used for statistical analysis. After implantation of the PS design, average patellofemoral area contact pressure was significantly lower (P ≤ 0.006) compared with the CR design (PS: 3.58 ± 1.25 MPa; CR: 4.31 ± 1.40 MPa). Accordingly, average patellofemoral peak contact pressure decreased significantly (P ≤ 0.02) with the PS design (6.12 ± 2.37 MPa) in comparison with the CR design (7.17 ± 2.41 MPa). On average, the centre of pressure motion was more physiological with the PS design compared to the CR design over the complete extension cycle. However, this was not significant. In conclusion, the data suggest less patellofemoral contact pressure of a posterior stabilized TKA design in comparison to a cruciate retaining design.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) has traditionally been used as an effective treatment for osteoarthritis (OA), relieving pain and restoring function of these patients. However, a considerable amount of patients are dissatisfied with their knee arthroplasty [40]. Anterior knee pain after TKA is one of the most common patient complaints leading to revision procedures [1, 7, 8, 29]. Surgical technique and prosthesis design are considered the most important factors affecting the extent of this problem [1, 29, 38]. The bearing surface forces and contact patterns generated at the patellofemoral joint are altered after TKA compared to the normal knee [27, 41]. In this context, increased patellofemoral contact pressures after TKA are held responsible for anterior knee pain [18, 31, 42].
In the knee, the posterior cruciate ligament (PCL) is the only isolated ligament that provides initial restraint against anterior posterior translation of the tibia at all angles of flexion undergoing a complex twisting motion [12, 19]. Furthermore, the PCL plays an important role in the control of the medial contact point during flexion [30, 32]. To restore the normal function of the PCL after TKA, however, remains difficult. The use of a cruciate retaining (CR) TKA was shown to result in more clinical and radiological laxity [13, 14, 46]. In a fluoroscopic analysis, subjects having a posterior cruciate substituting (posterior stabilized—PS) TKA were observed having greater and more consistent posterior femoral rollback of the lateral condyle (but less in magnitude than in normal knees), less paradoxical anterior sliding of the femur and more normal tibiofemoral axial rotation patterns than those determined for subjects having a CR TKA [14, 16, 46, 47]. This was attributed to engagement of the femoral component cam with the tibial post. However, both posterior cruciate retaining and posterior cruciate substituting TKAs have shown good or excellent scores at mid- and long-term follow-up [6, 20].
Little is known about the influence of the use of a CR or PS design on patellofemoral contact pressure and kinematics with a potential effect on anterior knee pain. The purpose of this in vitro study was to compare the influence of different prosthesis designs (PS vs. CR) on patellofemoral contact mechanics.
Materials and methods
Eight fresh frozen cadaveric knee specimen (7 male, 1 female; mean age 76 ± 10 years) from donors, who consented in writing during their lifetime to the use of their body for research and education were tested in an isokinetic extension test in an in vitro simulation initially published by Stukenborg-Colsman et al. and Ostermeier et al. [37, 43]. This simulation allows approximation of loadings close to the magnitude of the physiological forces and moments about the knee.
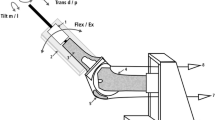
The specimens were frozen directly after harvest to −20°C, and subsequently thawed for 24 h at room temperature before preparation and testing. The knees were transected approximately 30 cm proximal and distal to the knee joint line. Skin and subcutaneous tissue were removed preserving the articular capsule, ligaments, and tendons. In each testing condition, the tibia was attached to the simulator at mid-length by means of a linear-rotational bearing, which permitted axial sliding and turning as well as rotation transverse to the axis of the tibia. The bearing in turn was attached to a swing arm, which allowed varus–valgus rotation. The weight of the swing arm itself with the mounted knee specimen was equalised by a counter-weight, the load measuring sensor of the swing arm itself was self weight compensated. The swing arm was equipped with a strain-gage based load measuring device, which allowed the extending moment applied to the tibia to be monitored continuously. Movement of the tibia was generated by the coordinated activation of three hydraulic cylinders, one to simulate variable quadriceps muscle force, the second to simulate a constant 100 N flexion force of the hamstrings during the extension cycle, and the third cylinder to apply an external flexion moment. Quadriceps force was transmitted through a special clamp, which was attached on the quadriceps tendon. Hamstring force was divided evenly between the clamps attached to the biceps femoris muscle on the lateral and the gracile and semimenbranosus muscle on the medial side. An isokinetic extension cycle with an angular velocity of 10°/s was simulated between 120° knee flexion and full extension using an extension moment of 31 Nm which represents a physiological extension moment, flexion angle was measured by an electronic goniometer attached to the swing arm with an accuracy and repeatability of 0.1° at a sampling frequency of 10 Hz [37, 43].
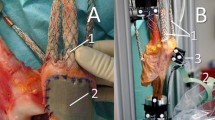
Patellofemoral contact pressures were evaluated using a 33 × 22 mm electronic pressure sensitive film (K-Scan 4000, Tekscan, Boston, USA) as described previously [35]. The pressure films were first preconditioned ten times by repeated loading and unloading to 1,500 N, and subsequently calibrated according to the manufacturer’s guidelines with a two-point method at 1,000 and 1,500 N load levels which were applied on the entire area of the pressure film in a material testing device (Minibionix 858, MTS Corporation, Minneapolis, USA). Using the recorded pressure distribution and the load on each ‘‘sensel’’, the pressure calibration was computed by the software (Tekscan® software v4.23, Tekscan, Boston, USA). A 0.1 mm Teflon film was glued on the sensor to allow stable suture fixation. The sensor was attached to the unresurfaced patella by silicone glue and sutured to the patella surrounding soft tissue by 1–0 sutures [35]. Area contact pressure (ACP) and peak contact pressure (PCP) were evaluated. In addition, the centre of pressure as the geometric centre of the loaded pressure area was used to follow patellar tracking during the extension cycle.
The knees were operated according to the Genesis II system (Smith & Nephew, Memphis, TN, USA). An intramedullary alignment rod was referenced for the femoral resection. Tibial reference was taken from the compartment that showed more wear and 11 mm were resected applying an extramedullary alignment rod. Balancing and alignment was checked using a spacer block. The patella remained unresurfaced.
Patellofemoral pressures of all knees were recorded in a first test cycle after implantation of a cruciate-retaining (CR) design and in a second test cycle after replacement by a posterior stabilized (PS) design, both with an 11 mm PE inlay.
Mean, median and standard deviation values were evaluated using SPSS 11.0 (SPSS Inc., Chicago, IL). For statistical analysis, a paired sampled t test to compare mean values (significance, P ≤ 0.05) was used.
Results
Continuous data were obtained at every trial. The highest mean area contact pressures (ACP) and peak contact pressures (PCP) were observed at deep flexion (Figs. 1, 2; Tables 1, 2). Mean patellofemoral ACP and PCP decreased with extension in both testing conditions (Figs. 1, 2). Whereas obtained pressure values remained relatively constant between 120° and 90° flexion as well as PCP between 60° and 0° and ACP between 40° and 0°, a continuous decrease was observed between 90° and 60° (PCP) and between 90° and 40° (ACP), respectively.
Considering the complete extension cycle from 120° to 0°, average ACP was significantly lower (P ≤ 0.006) after implantation of the posterior stabilized design (PS) compared with the cruciate retaining (CR) design (PS 3.58 ± 1.25 MPa, CR 4.31 ± 1.40 MPa). Accordingly, average PCP decreased significantly (P ≤ 0.02) with the PS design (6.12 ± 2.37 MPa) in comparison with the CR design (7.17 ± 2.41 MPa). Mean values were 15–21% lower with a PS design compared to the CR design over the complete extension cycle (Tables 1, 2).
During the extension cycle, the mean centre of patellar pressure was initially medialised in deep flexion degrees in both the testing conditions followed by a lateralization from approximately 80°–100° flexion to full extension (Fig. 3). On average, lateralization was less with the PS design compared to the CR design over the complete extension cycle (120°: −3.1 ± 0.7 mm; 80°: −0.5 ± 1.7 mm; 40°: −1.5 ± 1.3 mm; 0°: −2.4 ± 1.0 mm). The mean centre of patellar pressure of the CR design remained relatively constant during the extension cycle between 90° and 25° with an obvious proximalisation in the last 25° to extension. An apparent distalisation in deep flexion degrees, relatively constant position between 100° and 50° and a following considerable proximalisation to full extension was observed with the PS design (Fig. 3). On average, the position of the mean centre of patellar pressure of the PS design was more proximal than with the CR design (120°: −2.9 ± 0.5 mm; 80°: −0.4 ± 2.5 mm; 40°: −2.2 ± 0.5 mm; 0°: −2.9 ± 0.8 mm). However, these observations were not significantly different.
Discussion
The extensor mechanism and the patella are one of the most frequent causes for complications after TKA reasons leading to revision procedures [1, 7, 8, 29, 39]. To resurface or not to resurface the patella has been the major discussion to address the problem of anterior knee pain in recent years [23]. However, other factors for being associated with anterior knee pain as abnormal rotational placement of the tibial and femoral components and design features have also to be considered [2, 11, 22, 28, 29, 38].
Whether the posterior cruciate ligament should be retained or resected has been the subject of argument for many years. We investigated the influence of the use of a CR or PS design on patellofemoral contact pressure and kinematics over a full extension cycle of the knee after TKA in vitro. The applied method is well established and numerous publications have resulted from the previously described setup [34, 35, 42].
Patella kinematics are altered after TKA, quite possibly due to changes in the bearing surface forces generated at the patellofemoral joint [27, 41]. Low patellofemoral pressure was considered to be advantageous as high pressures might be accountable for anterior knee pain [18, 31, 42]. The setup described in this study measures dynamic changes of patellofemoral pressure in a constant moment extension cycle at 31 Nm. The ratio of forces between patellar tendon and quadriceps tendon varies significantly with the flexion angle [25]. Among other things, the ratio is determined by the relative position of load and lever arms to each other [26]. The patella is considered to serve as a linkage for the lever arm over the knee joint. Changes of anteroposterior stability and of the position of the tibia directly influence the relative length of the lever arms and thus transmitted forces and patellofemoral pressure.
Our results suggest significantly lower mean area and peak contact pressures with a PS design compared to the CR design after TKA over an extension cycle from 120° flexion to full extension. Area contact pressure values measured with the PS design were comparable as measured in intact knees in the same testing setup [35]. Thus, contact pressures with a CR design were increased compared to intact conditions which is consistent with reports from the literature [17, 31, 42]. Patellofemoral forces have been experimentally estimated using three-dimensional fluoroscopic kinematic analysis in the patellofemoral joint in vivo. Findings suggested significant kinematic differences between cruciate retaining and posterior stabilized arthroplasties with a greater and more consistent posterior femoral rollback and less paradoxical anterior sliding of the femur for subjects having a posterior stabilized TKA [14, 16, 46, 47]. These findings along with our results are consistent with the conclusion of a finite element model by D′Lima et al. [11] to get better insight into the effects of design parameters on patellofemoral forces and on local contact stresses. The model supported the hypothesis that femoral rollback reduces patellofemoral pressure by improving the efficiency of the extensor mechanism.
With the determination of the centre of patellar pressure motion, the relative patellar tracking to the femur during the extension cycle could be followed. Correlation with the patella motion was shown using an ultrasound based threedimensional motion analysis system in the same testing setup [33, 35]. During the extension cycle, the centre of mean patella pressure moved laterally and proximally in both testing conditions during the extension cycle. Although not significant, knees with a PS design showed less lateral shifting but increased longitudinal shifting in the proximal direction. The centre of mean patella pressure tracking of our study in the longitudinal direction confirms results of the patella motion observed in other in vitro studies evaluating patella contact after TKA [24, 33]. The contact positions of a PS versus CR design of the patellofemoral joint were compared under fluoroscopic surveillance measured from the patella mass center in subjects performing deep knee bends to maximum flexion. Observed differences in the superior/inferior average contact positions were comparable to our findings showing a difference of 0.4 ± 2.6 mm at 90° flexion and 3.3 ± 2.5 mm at full extension [27]. The femorotibial contact point of knees with a PS design rolls back posteriorly during flexion similar to normal knees whereas knees with a CR design translate anteriorly during midflexion (30–90°) in a substantial number of cases [15]. This was confirmed in other studies [3, 46, 47] and may explain the relatively constant position of the centre of patellar pressure of the CR design in our study in contrast to the apparently more physiological tracking of the PS design.
A limitation inherent to all cadaver biomechanical models is that only approximation of the living system can be achieved. Area and peak contact pressures were determined by an electronic pressure sensitive sensor. The reliability of the K-Scan sensor was verified in several studies [4, 21, 35]. Limitations of the sensor include the thickness (0.1 mm), its sensitivity to temperature changes, its disposition for crinkling and the establishment of the position [5]. The simulated extension cycle in this study did not include a weight bearing component. Nonetheless, unlike other in vitro simulations, physiological muscle forces were applied (up to 1,500 N), and the kinematics of knee motion attained using this simulator have been shown to be similar to physiological on physiological specimens [36]. Correct balancing of the joint with tensioning of the PCL is of utmost importance to obtain optimal kinematics after CR TKA. Errors are less forgiving than after PS TKA. The spacer block method that we used in our study is well established. However, a spring loaded tensioning device appeared to result in better radiographic alignment data and decreased manipulation rates after TKA compared to the spacer block method [44]. An increase of 1 mm in the flexion gap in the tensed CR TKA knee was shown to result in a mean anterior tibial translation of 1.25 ± 0.79 mm [9]. A possible impact on the patellofemoral joint contact pressure must be considered, respectively.
The clinical relevance of our findings remains unclear. A recent multicenter prospective randomized clinical trial compared the use of a CR versus PS TKA design using the Genesis II TKA system. While results were comparable in regards of clinical outcomes, the PS design appeared to support significantly improved range of motion when compared with the CR design [20]. These findings confirmed previous reports comparing a CR versus a PS design [10, 16, 45]. However, none of these studies explicitly put attention to the patellofemoral joint. At least Harato et al. [20] reported of five patients with anterior knee pain and seven patients having a stiff knee with a CR design compared to only two patients with anterior knee pain and one patient with a stiff knee with a PS design. Although this difference was not statistically significant, the authors concluded that an explanation may be related to differences in knee kinematics; specifically, the replication of PCL functions with the PS design.
In conclusion, our data suggest less patellofemoral contact pressure and superior patellofemoral kinematics of a posterior stabilized TKA design in comparison to a cruciate retaining design. It is hypothesised that decreased patellofemoral contact pressure with a PS design is caused by greater and more consistent posterior femoral rollback and less paradoxical anterior sliding and may result in less frequent anterior knee pain in an in vivo application.
References
Aglietti P, Baldini A, Buzzi R, Indelli PF (2001) Patella resurfacing in total knee replacement: functional evaluation and complications. Knee Surg Sports Traumatol Arthrosc 9(Suppl 1):S27–S33. doi:10.1007/s001670000160
Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT (1993) The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 287:170–177
Banks SA, Markovich GD, Hodge WA (1997) In vivo kinematics of cruciate-retaining and -substituting knee arthroplasties. J Arthroplasty 12:297–304. doi:10.1016/S0883-5403(97)90026-7
Becher C, Huber R, Thermann H, Paessler HH, Skrbensky G (2008) Effects of a contoured articular prosthetic device on tibiofemoral peak contact pressure: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 16:56–63. doi:10.1007/s00167-007-0416-7
Beck PR, Thomas AL, Farr J, Lewis PB, Cole BJ (2005) Trochlear contact pressures after anteromedialization of the tibial tubercle. Am J Sports Med 33:1710–1715. doi:10.1177/0363546505278300
Bourne RB, Laskin RS, Guerin JS (2007) Ten-year results of the first 100 Genesis II total knee replacement procedures. Orthopedics 30:83–85
Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL (2007) A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res 464:65–72
Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, Stevenson TM (2006) Patellar resurfacing in total knee replacement: a ten-year randomised prospective trial. J Bone Joint Surg Br 88:734–739. doi:10.1302/0301-620X.88B6.16822
Christen B, Heesterbeek P, Wymenga A, Wehrli U (2007) Posterior cruciate ligament balancing in total knee replacement: the quantitative relationship between tightness of the flexion gap and tibial translation. J Bone Joint Surg Br 89:1046–1050. doi:10.1302/0301-620X.89B8.18976
Clark CR, Rorabeck CH, MacDonald S, MacDonald D, Swafford J, Cleland D (2001) Posterior-stabilized and cruciate-retaining total knee replacement: a randomized study. Clin Orthop Relat Res 392:208–212. doi:10.1097/00003086-200111000-00025
D’Lima DD, Chen PC, Kester MA, Colwell CW Jr (2003) Impact of patellofemoral design on patellofemoral forces and polyethylene stresses. J Bone Joint Surg Am 85A(Suppl 4):85–93
DeFrate LE, Gill TJ, Li G (2004) In vivo function of the posterior cruciate ligament during weightbearing knee flexion. Am J Sports Med 32:1923–1928. doi:10.1177/0363546504264896
Dejour D, Deschamps G, Garotta L, Dejour H (1999) Laxity in posterior cruciate sparing and posterior stabilized total knee prostheses. Clin Orthop Relat Res 364:182–193. doi:10.1097/00003086-199907000-00024
Dennis DA, Komistek RD, Colwell CE Jr, Ranawat CS, Scott RD, Thornhill TS, Lapp MA (1998) In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res 356:47–57. doi:10.1097/00003086-199811000-00009
Dennis DA, Komistek RD, Hoff WA, Gabriel SM (1996) In vivo knee kinematics derived using an inverse perspective technique. Clin Orthop Relat Res 331:107–117. doi:10.1097/00003086-199610000-00015
Dennis DA, Komistek RD, Mahfouz MR (2003) In vivo fluoroscopic analysis of fixed-bearing total knee replacements. Clin Orthop Relat Res 410:114–130. doi:10.1097/01.blo.0000062385.79828.72
Fuchs S, Schutte G, Witte H, Rosenbaum D (2000) Retropatellar contact characteristics in total knee arthroplasty with and without patellar resurfacing. Int Orthop 24:191–193. doi:10.1007/s002640000140
Fuchs S, Skwara A, Tibesku CO, Rosenbaum D (2005) Retropatellar contact characteristics before and after total knee arthroplasty. Knee 12:9–12. doi:10.1016/S0968-0160(02)00045-5
Gollehon DL, Torzilli PA, Warren RF (1987) The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am 69:233–242
Harato K, Bourne RB, Victor J, Snyder M, Hart J, Ries MD (2008) Midterm comparison of posterior cruciate-retaining versus -substituting total knee arthroplasty using the Genesis II prosthesis. A multicenter prospective randomized clinical trial. Knee 15:217–221. doi:10.1016/j.knee.2007.12.007
Harris ML, Morberg P, Bruce WJ, Walsh WR (1999) An improved method for measuring tibiofemoral contact areas in total knee arthroplasty: a comparison of K-scan sensor and Fuji film. J Biomech 32:951–958. doi:10.1016/S0021-9290(99)00072-X
Healy WL, Wasilewski SA, Takei R, Oberlander M (1995) Patellofemoral complications following total knee arthroplasty. Correlation with implant design and patient risk factors. J Arthroplasty 10:197–201. doi:10.1016/S0883-5403(05)80127-5
Helmy N, Anglin C, Greidanus NV, Masri BA (2008) To resurface or not to resurface the patella in total knee arthroplasty. Clin Orthop Relat Res 466:2775–2783. doi:10.1007/s11999-008-0420-3
Hsu HC, Luo ZP, Rand JA, An KN (1997) Influence of lateral release on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthroplasty 12:74–83. doi:10.1016/S0883-5403(97)90051-6
Huberti HH, Hayes WC (1984) Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am 66:715–724
Kaufer H (1971) Mechanical function of the patella. J Bone Joint Surg Am 53:1551–1560
Komistek RD, Dennis DA, Mabe JA, Walker SA (2000) An in vivo determination of patellofemoral contact positions. Clin Biomech (Bristol, Avon) 15:29–36. doi:10.1016/S0268-0033(98)00061-8
Kulkarni SK, Freeman MA, Poal-Manresa JC, Asencio JI, Rodriguez JJ (2001) The patello-femoral joint in total knee arthroplasty: is the design of the trochlea the critical factor? Knee Surg Sports Traumatol Arthrosc 9(Suppl 1):S8–S12. doi:10.1007/s001670000155
Lindstrand A, Robertsson O, Lewold S, Toksvig-Larsen S (2001) The patella in total knee arthroplasty: resurfacing or nonresurfacing of patella. Knee Surg Sports Traumatol Arthrosc 9(Suppl 1):S21–S23. doi:10.1007/s001670000154
Logan M, Williams A, Lavelle J, Gedroyc W, Freeman M (2004) The effect of posterior cruciate ligament deficiency on knee kinematics. Am J Sports Med 32:1915–1922. doi:10.1177/0363546504265005
Matsuda S, Ishinishi T, White SE, Whiteside LA (1997) Patellofemoral joint after total knee arthroplasty. Effect on contact area and contact stress. J Arthroplasty 12:790–797. doi:10.1016/S0883-5403(97)90010-3
Nakagawa S, Johal P, Pinskerova V, Komatsu T, Sosna A, Williams A, Freeman MA (2004) The posterior cruciate ligament during flexion of the normal knee. J Bone Joint Surg Br 86:450–456. doi:10.1302/0301-620X.86B3.14330
Ostermeier S, Buhrmester O, Hurschler C, Stukenborg-Colsman C (2005) Dynamic in vitro measurement of patellar movement after total knee arthroplasty: an in vitro study. BMC Musculoskelet Disord 6:30. doi:10.1186/1471-2474-6-30
Ostermeier S, Holst M, Bohnsack M, Hurschler C, Stukenborg-Colsman C, Wirth CJ (2007) In vitro measurement of patellar kinematics following reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 15:276–285. doi:10.1007/s00167-006-0200-0
Ostermeier S, Holst M, Hurschler C, Windhagen H, Stukenborg-Colsman C (2007) Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: an in vitro study. Knee Surg Sports Traumatol Arthrosc 15:547–554. doi:10.1007/s00167-006-0261-0
Ostermeier S, Hurschler C, Stukenborg-Colsman C (2004) Quadriceps function after TKA–an in vitro study in a knee kinematic simulator. Clin Biomech (Bristol, Avon) 19:270–276. doi:10.1016/j.clinbiomech.2003.11.006
Ostermeier S, Hurschler C, Windhagen H, Stukenborg-Colsman C (2006) In vitro investigation of the influence of tibial slope on quadriceps extension force after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 14:934–939. doi:10.1007/s00167-006-0078-x
Poilvache PL (2001) The patella in total knee replacement: technical aspects on the femoral side. Knee Surg Sports Traumatol Arthrosc 9(Suppl 1):S13–S18. doi:10.1007/s001670000153
Rand JA (1994) The patellofemoral joint in total knee arthroplasty. J Bone Joint Surg Am 76:612–620
Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L (2000) Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 71:262–267. doi:10.1080/000164700317411852
Stiehl JB, Komistek RD, Dennis DA, Keblish PA (2001) Kinematics of the patellofemoral joint in total knee arthroplasty. J Arthroplasty 16:706–714. doi:10.1054/arth.2001.24443
Stukenborg-Colsman C, Ostermeier S, Burmester O, Wirth CJ (2003) Dynamic in vitro measurement of retropatellar pressure after knee arthroplasty. Orthopade 32:319–322. doi:10.1007/s00132-002-0442-6
Stukenborg-Colsman C, Ostermeier S, Hurschler C, Wirth CJ (2002) Tibiofemoral contact stress after total knee arthroplasty: comparison of fixed and mobile-bearing inlay designs. Acta Orthop Scand 73:638–646. doi:10.1080/000164702321039598
Swank M, Romanowski IR, Korbee LL, Bignozzi S (2007) Ligament balancing in computer-assisted total knee arthroplasty: improved clinical results with a spring-loaded tensioning device. Proc Inst Mech Eng [H] 221:755–761. doi:10.1243/09544119JEIM269
Tanzer M, Smith K, Burnett S (2002) Posterior-stabilized versus cruciate-retaining total knee arthroplasty: balancing the gap. J Arthroplasty 17:813–819. doi:10.1054/arth.2002.34814
Victor J, Banks S, Bellemans J (2005) Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg Br 87:646–655. doi:10.1302/0301-620X.87B5.15602
Yoshiya S, Matsui N, Komistek RD, Dennis DA, Mahfouz M, Kurosaka M (2005) In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty 20:777–783. doi:10.1016/j.arth.2004.11.012
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Becher, C., Heyse, T.J., Kron, N. et al. Posterior stabilized TKA reduce patellofemoral contact pressure compared with cruciate retaining TKA in vitro. Knee Surg Sports Traumatol Arthrosc 17, 1159–1165 (2009). https://doi.org/10.1007/s00167-009-0768-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0768-2