Abstract
The weak point in an ACL reconstruction immediately after surgery is the tibial fixation of the graft. This factor will often limit the return to load-inducing activities. Many new hamstring-graft fixation devices have been introduced for cruciate ligament reconstruction, but there is little comparative data on their performance. This work tested the hypotheses that some of these devices will resist graft slippage under cyclic loads better than others, and that some will have higher ultimate strength than others. Five devices were tested: WasherLoc, Intrafix fastener; and RCI, Delta Tapered, and Bicortical interference screws. Cyclic loads representing normal walking activity (1000 cycles from 70 to 220 N) and ultimate strength tests were done, using calf tibiae (similar bone density to young human tibiae) and four-strand tendon grafts, with eight tests of each device for each of cyclic and ultimate tensile strength tests. A series of graft creep tests under cyclic loads was also done. The results showed that there was no significant difference in graft construct elongation under cyclic loads (range 0.7–1.3 mm) after allowing for 0.4 mm mean graft creep. The WasherLoc gave the highest ultimate strength (945 N, p <0.001, range 490–945 N). We concluded that all devices performed well under cyclic loads that represented normal walking activity, but the ultimate strengths differed. The performance under cyclic load was better than has been published for conventional interference screws. This evidence suggests that it may now be safe to mobilise younger patients less cautiously immediately after hamstring-graft ACL reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction continues to develop on many fronts as it has done since the early 1980s. In the USA about one in three thousand people undergo an ACL reconstruction per annum, with revision surgery also on the increase [15]. However, there are aspects of the operation that still need further improvement and development. The pressure from both top athletes and non-professional sportsmen for a speedier return to competitive activities has forced surgeons and biomechanical engineers to explore and improve all aspects of cruciate ligament reconstruction.
Major advances have occurred in many areas, including the better understanding of ACL anatomy leading to a more exact placement of autologous grafts, for instance [6, 10, 11]. Also, there have been advances in the selection of autologous grafts, which have tended recently to move away from the bone–patellar tendon–bone graft to the use of hamstring-tendon grafts.
The improved operation has meant that patients are undergoing more intensive rehabilitation programmes and stressing the reconstruction much earlier [18]. This has highlighted the role of graft fixation, because the grafts are being stressed almost immediately, before any bone or tendon osseo-integration within either the tibial or femoral tunnels has occurred. The reconstructions are most vulnerable to elongation at their fixation points in this critical period, which may lead to a slack graft [7].
Quadruple-strand hamstring-graft reconstruction has become more popular in recent years, and there have been a number of studies demonstrating its equivalence to bone–patellar tendon–bone grafts [5, 12]. The low co-morbidity of hamstring-graft harvest [19, 22] means that patients are eager to return to activity soon after their surgery. However, fixation of the quadruple hamstring-tendon graft in the tibial tunnel can be a problem, and several advances have been made to minimise elongation of the construct in the early post-operative stage.
Ideally, the fixation of the construct should be similar in strength to that of a native human ACL, but this has proved elusive with current fixation devices. The problem is not with the graft, which has similar biomechanical properties to the ACL, but with the bony fixation in the tibia [8, 13, 16, 21]. The fixation needs to be strong enough to allow early rehabilitation and hold the graft in place until the histological transition to calcified fibrocartilage has occurred at the bone–tendon interface.
The purpose of the work described in this paper is to experimentally evaluate the ultimate strength, and security of fixation under cyclical conditions, of five different tibial ACL graft-fixation systems, and assess their ability to prevent graft construct elongation at the tibial fixation point.
Materials and methods
The tibial bones used for the testing came from calves aged between four and six months. These have similar bone density to young adult human bones [20]. The tibias were frozen at −20°C until they were required for testing. The ACL grafts were bovine digital extensor tendons. These have the same elastic properties as human hamstring tendons [4]. The diameter of the multistrand bundle of tendons was between 8 and 9 mm, as this is most commonly found clinically. This ensured that the experimental tests used the same diameter screws to compare different fixation systems.
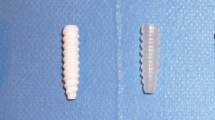
The tibial fixation devices were selected to cover a range of concepts, including interference screws placed within the tibial tunnel—engaging either the distal tibial cortex or both distal and proximal cortices—as well as fixation devices applied outside the tunnel (Fig. 1). The five devices selected were:
-
1. The RCI screw from Smith and Nephew
-
2. The bioabsorbable Bicortical interference screw fixation from Arthrex
-
3. The Delta Tapered bioabsorbable screw from Arthrex
-
4. The WasherLoc device from Arthrotek
-
5. The Intrafix ACL tibial fastener from Mitek
The RCI screw
The RCI screw was designed to engage both distal and proximal cortices and was 8 mm in diameter and 40 mm long. The testing used 8 mm-diameter grafts in an 8 mm tibial tunnel that was 40 mm long.
Bicortical two-screw system
This was in two parts; the first screw was inserted into the tibial tunnel until it engaged the subchondral bone, while the second screw fixed the graft against the distal cortex. Its head was cut at an angle, so that it lay flush with the cortex. This system was bioabsorbable. The proximal screw was 9 mm in diameter and the distal screw 10 mm in diameter. The tunnel was 40 mm long and 9 mm in diameter.
Delta Tapered screw
The Delta Tapered screw was made of bioabsorbable PLLA and engaged the distal cortex of the tibia. This non-cannulated interference screw was tapered, with a diameter of 8.5 mm near the tip and 10 mm at the head. The screw was 35 mm long and the tunnel was 8.5 mm in diameter and 40 mm long.
WasherLoc device
The WasherLoc device differed from the above systems in that the screw had a spiked washer and was not placed within the tibial tunnel. The WasherLoc lay within the first 16 mm of the distal part of the tibial tunnel, and was recessed into the anterior cortex. The washer trapped the tendons at the distal tunnel entrance and was then secured by a bicortical screw that was not placed into the tunnel but was inserted from anterior to posterior across the proximal tibial. The tibial tunnel was again drilled to 8 mm for the diameter of the graft and 40 mm long.
Tibial fastener
This device consisted of a sheath that was split longitudinally into four parts, each of which included a gutter for one strand of the graft. A screw of 10 mm diameter by 30 mm long was driven up the centre of the fastener, thus pressing the four tendons against the tunnel wall. A tensioner was used to precondition the grafts before insertion of the screw to ensure equal tension on all strands of the graft.
The calf tibias were defrosted immediately prior to usage and kept moist throughout experimentation. Each tibia was sectioned through the isthmus of the tibial diaphysis and then mounted into a steel cylinder and secured by eight pointed screws that penetrated the tibial cortex.
The ACL was excised and the tibial tunnels were prepared as per each manufacturer’s surgical technique, using the tibial jigs, guide wires and drill bits. The tunnel diameter depended on the graft size and information from the manufacturer, and the tunnel length was 40 mm. The distal entrance to the tunnel was placed in the antero-medial tibial cortex, and the proximal exit was placed in the ACL footprint, between the tibial spines.
The steel cylinder holding the tibia was placed in a steel fixture that was bolted to the base of an Instron 5565 computer-controlled materials-testing machine (Instron Ltd, High Wycombe, UK). This fixture had several degrees of freedom of movement that allowed the vertical angle and rotation of the tibia to be adjusted before it was locked, with the tibial tunnel aligned with the loading axis of the Instron machine (Fig. 2). This alignment meant that graft tension acted directly onto the fixation, with no friction effects due to angulation where it entered the tibial plateau, and so it represented the mechanical worst-case scenario.
The tendon grafts were prepared as per standard intra-operative technique. Three digital extensor tendons could be harvested from each calf leg specimen. The tendons were removed using sharp dissection, and then any connective tissue or muscle stripped from the length of the tendon. Each harvested graft was then kept moist in Ringer’s solution until it was required. The multistrand graft was looped through a stainless-steel shackle above the tibial plateau to act as the femoral component. Using the shackle with a broad cylindrical barrel of 4 mm in diameter eliminated any fixation slippage that may have occurred in a femoral bone attachment. Vicryl 1–0 was then sutured onto the distal ends of each graft, as per a normal ACL reconstruction, with an interlocking stitch for 40 mm. The ends of the Vicryl were then pulled distally through the bone tunnel and the Vicryl was then used to obtain the correct graft tension. The ‘femoral’ shackle was then lowered to 10 mm above the tibial plateau and the grafts were tensioned through the tunnel. The grafts were placed under 70 N of tension before each fixation device was applied. This could be measured accurately on the Instron machine, and correlated well with the intra-operative pull of a surgical assistant.
All testing was done on the Instron 5565 materials-testing machine using Merlin control software, that was able to capture data via ASCII files that were then transferred to a database for statistical analysis.
Cyclical loading
The load readout on the test machine was zeroed at 70 N, the load at which the grafts had been secured. A 0 N to 150 N load cycle was then applied 1000 times at a crosshead speed of 100 mm/min. This gave approximately 80 cycles per minute, with the graft tension varying from 70 to 220 N. This protocol reflects the combination of the graft pretension applied by the surgeon, plus the cyclic load applied to the ACL in normal walking [14], and is also in line with the in vitro testing protocols of cruciate ligaments set out by Beynnon and Amis [2]. Changes in maximum crosshead movement relative to the extension at the first load peak were recorded. This represented slippage of the graft relative to the tibia, plus creep elongation. Eight constructs were tested with each fixation device.
Ultimate strength testing
The experimental set up for the ultimate strength testing was identical to that of the cyclical load testing. However, the Instron machine was set for just one increasing cycle, and was stopped after pullout of the construct. The highest value recorded by the Instron machine at failure was taken as the ultimate strength in Newtons (N). Failure was deemed to have occurred at the point where no further load could be applied due to slip of the graft past its fixation device. Eight constructs were tested with each fixation device.
Creep testing
Before testing the devices, the tendons and experimental test fixture were assessed for creep. This was done by taking a multi-strand tendon graft, and instead of placing the sutured ends into a tibial tunnel they were placed into the jaws of a steel-ridged clamp whose locking nuts were tightened gently; the clamp and graft within the clamp were then frozen with liquid CO2 and the clamp then tightened around the frozen graft. This left 50 mm of unfrozen graft above the clamp leading to the proximal ‘femoral’ shackle fixation. This was intended to represent the ‘worst case’ with graft fixation at the distal end of the tibial tunnel. The graft was marked with an ink line across the exit point from the jaws, so that the construct could be checked to ensure that there had been no slippage at that point. This construct was then subjected to the normal cyclical load testing protocol. Five tendon constructs were tested. Changes in crosshead position at peak load were caused by creep in the graft and graft deformation over the shackle barrel. The data obtained was used to construct calibration curves, thus accounting for creep within the experimental set-up. The mean creep from these tests could be deducted from the cyclical load test results, thus leaving the length change caused by fixation slippage, which was movement of the graft relative to the bone at the point of fixation.
Data analysis
The slippages of the best- and worst-performing devices under cyclical loading were compared against those of the other devices using one-way analysis of variance (ANOVA), followed by Newman-Keuls and Tukey’s Multiple Comparison Test. The significance level was set at p =0.0125. A similar analysis was used for the ultimate strength results. The upper 95% prediction intervals for the amount of graft slippage (mm), and the lower 95% prediction intervals for the failure strength (N) were also calculated.
Results
Creep tests
The mean creep was 0.38 mm. This was subtracted from the fixation testing results before analysis of fixation slippage, leaving a maximum error of 0.23 mm due to inter-specimen variation.
Cyclical loading
From Fig. 3 and Table 1 it can be seen that the mean slippage ranged from the tibial fastener at 0.69 mm to the RCI screw at 1.3 mm after 1000 load cycles. There was no statistically-significant difference on any of the comparison testing to suggest that one method was better at reducing slippage than another ( p >0.05). A post hoc power calculation found that the experiments had an 80% power to detect a difference in graft slippage of 1.17 mm with 95% confidence. It is therefore very unlikely that these experiments missed a clinically-significant difference in performance, given that the IKDC score is “normal” until the side-to-side difference reaches 3 mm. The upper 95% prediction interval was greater than 3 mm for the RCI and Delta screws, and below 2 mm for the WasherLoc.
Ultimate strength
Fig. 4 shows that the devices had a different ranking for ultimate strength from that for graft slippage. The WasherLoc device had a mean ultimate strength of 946 N, and this was significantly greater than the ultimate strengths of the RCI screw, Delta Tapered screw and the Intrafix tibial fastener ( p <0.001) and the Bicortical two screw system ( p <0.05; see Fig. 4, Table 2).
Among the interference-screw systems the Bicortical screw had the highest ultimate strength (770 N), which was significantly greater than the RCI screw and the Intrafix Tibial Fastener ( p <0.01). The Bicortical screw system statistically did not outperform the Delta Tapered screw ( p >0.05).
The lower 95% prediction interval for ultimate strength ranged from 284 N for the Intrafix to 396 N for the Bicortical screw system (Table 2).
Discussion
The most important finding in this work was that the recently-developed tibial fixation methods that were tested performed much better under cyclic loading than did the conventional shorter interference screws tested in earlier studies of hamstring-tendon fixation. Previous tests using the same animal model and cyclic loading regime [7, 9] had found that 25 mm- and 35 mm-long interference screws that were not engaging both ends of the tibial tunnel allowed approximately twice as much graft slippage under load: approximately 3 mm after 1000 cycles of 150 N. This had led to a recommendation that rehabilitation exercises should be prescribed with caution pending extra security arising from graft–bone healing. In contrast, the present results suggest that modern ACL hamstring-graft fixation methods may not allow clinically-significant graft slippage to occur if the patient is allowed to walk immediately after ACL reconstruction.
The fixation systems with the highest ultimate strength also gave the most consistent behaviour under cyclic load. Table 1 shows that two of the fixation systems tested had an upper-95% prediction interval of more than 3 mm graft slippage under 1000 load cycles. Outlying data points increased the standard deviations and prevented the statistical tests from showing significant differences in mean behaviour. The variability in construct behaviour was found to give an 80% power to detect a difference of 1.2 mm with 95% confidence. The consistency of graft construct behaviour is very important when considering which of these devices to choose for clinical use, because each of the outlying data points in these experiments in vitro may represent individual patients whose grafts will tend to become loose under rehabilitation loading.
The clinical relevance of this study must be judged while noting the limitations inherent in the methods used. The principal point relates to the use of young bovine (calf) tibiae. Clearly the ideal situation would have been to obtain a sufficient number of young human adult tibiae, but this was not practical. Previous studies have shown that the calf tibia has similar proximal bone density to the young human [20], and comparative tests [3] showed that the results obtained from calf bones were closer to those of young humans than were results from elderly human bones. The massive strength of adult bovine bones suggests the possibility that the calf bones used in this study may also have given greater holding power than human bone, leading to optimistic results. However, previous tests using this protocol [7, 9] caused more graft slippage than is found clinically—the opposite tendency. This study also used bovine tendons, for similar reasons to those noted above. Our subjective impression, when handling these specimens, was that their quality was closer to that of young human tendons than was the elderly material that could be obtained post mortem. It has been shown that the differences in structural and material properties between bovine digital extensor tendons and young human hamstring tendons are negligible [4]. The reader should also note that the data presented in all studies of graft fixation in vitro relates only to the situation immediately post operation, before graft–bone healing has added greater security. Because of this, it is not realistic to continue these bench tests to high numbers of load cycles, because the reconstructions would also be affected by biological processes in longer timescales in vivo. Prior work [7, 9] has shown that the cyclic test protocol used in this work is severe enough to discover significant differences in graft fixation performance.
Critical judgement is required if these tests on bovine tissues in vitro are to be related to the clinical scenario. There is clinical evidence of good results for ACL reconstructions that used conventional 25 mm-long interference screws [17], and the present study found better performance for the devices tested than in previous work [7, 9] on the conventional 25 mm- and 35 mm-long screws. In this study, the constructs with the worst performance slipped by enough to allow the laxity of a knee to increase from “normal” to “nearly normal” on the IKDC scale. On the other hand, Yasuda et al. [22] deliberately set up knees with different levels of graft tension and joint laxity, yet these initial objective differences were not recognised by the subjective evaluations of their patients at follow-up.
The ultimate strength test results gave further evidence that graft security is related to engagement with strong cortical bone. The WasherLoc device not only clamped the tendon graft directly against the tibial cortex, it also allowed a large torque to be applied to the clamping screw, because it passed through two cortices. In earlier work on artificial graft-fixation devices [1], it was shown that their holding strength depended on the local thickness of cortical bone, even if their designers had claimed that they were intended to grip cancellous bone. It was also noted in that work that cortical bone is approximately thirty times stronger than cancellous. More recent work [9] has shown that whilst a longer interference screw tended to increase holding strength, a much more significant improvement in performance came from engaging the screw head and graft against the tibial cortex at the tunnel entrance. This explains why the Bicortical system gave the best results among the interference screws tested in this study, because it was designed with separate components that were intended to engage in both the proximal subchondral bone plate and the distal tunnel entrance. The variability of the integrity of individual graft–bone constructs led some to fail at low loads well below the mean ultimate strengths, and this is shown by the lower 95% ultimate strength intervals in Table 2.
The later generation of ACL hamstring graft fixation devices tested here gave much better results, when tested under the same conditions, than the shorter interference screws that have been in use for some years. This suggests that it may now be safe to allow young patients undergoing ACL reconstruction to mobilise and to walk normally immediately post operation—a clinically significant advance, assuming that this is not ruled out by other factors such as cartilage or meniscal damage. However, the variability of the performance of some of the devices tested suggests caution in transferring these findings to specific patients. Further work, using higher cyclic loads, may determine the safety of allowing more vigorous activities before graft healing to bone is expected.
References
Amis AA (1988) The strength of artificial ligament anchorages—a comparative experimental study. J Bone Joint Surg Br 70:397–403
Beynnon BD, Amis AA (1998) In vitro testing protocols for the cruciate ligaments and ligament reconstructions. Knee Surg Sports Traumatol Arthrosc 6:S70–S76
Brown GA, Pena F, Grontvedt T, Labadie D, Engebretsen L (1996) Fixation strength of interference screw fixation in bovine, young human and elderly human cadaver knees: influence of insertion torque, tunnel-block gap, and interference. Knee Surg Sports Traumatol Arthrosc 3:238–244
Donahue TL, Gregersen C, Hull ML, Howell SM (2001) Comparison of viscoelastic, structural and material properties of double-looped anterior cruciate ligament grafts made from bovine digital extensor and human hamstring tendons. J Biomech Eng 123:162–169
Eejerhed L, Kartus J, Servert N, Kohler K, Karlsson J (2003) Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomised study with a two-year follow-up. Am J Sports Med 31:19–25
Fu FH, Bennett CH, Ma CB, Menetrey J, Lattermann C (2000) Current trends in anterior cruciate ligament reconstruction. Am J Sports Med 28:124–130
Giurea M, Zorilla P, Amis AA, Aichroth P (1999): Comparative pull-out and cyclic-loading strength tests of anchorage of hamstring tendon grafts in anterior cruciate ligament reconstruction. Am J Sports Med 27:1–5
Hamner DL, Brown CH, Steiner ME, Hecker AT, Hayes WC (1999) Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am 81:549–557
Harvey AR, Thomas NP, Amis AA (2003) The effect of screw length and position of fixation of four-stranded hamstring grafts for anterior cruciate ligament reconstruction. Knee 10:97–102
Jackson DW, Gasser SI (1994) Tibial tunnel placement in ACL reconstruction. Arthroscopy 10:124–131
Jackson DW, Schaefer RK (1990) Cyclops syndrome: loss of extension following intra-articular anterior cruciate ligament reconstruction. Arthroscopy 6:171–178
Jansson KA, Linko E, Sandelin J, Harilainen A (2003) A prospective randomised study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med 31:12–18
Kurosaka M, Yoshiya S, Andrish JT (1987) A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med 15:225–229
Morrison JB (1969) function of the knee joint in various activities. J Biomed Eng 4:573–580
Noyes FR, Barber-Westin SD (1996) Revision anterior cruciate ligament surgery: experiences from Cincinnati. Clin Orthop 325:116–129
Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS (1984) Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 66:344–352
Pinczewski LLA, Dechan DJ, Salmon LJ, Russell VJ, Clingeleffer A (2002) A five-year comparison of patellar tendon versus four-strand hamstring tendon autograft for arthroscopic reconstruction of the anterior cruciate ligament. Am J Sports Med 30:523–536
Shelbourne KD, Patel DV (1999) Treatment of limited motion after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 7:85–92
Simonian PT, Harrison SD, Cooley VJ (1997) Assessment of morbidity of semitendinosus and gracilis tendon harvest for ACL reconstruction. Am J Knee Surg 10:54–59
Weiler A, Windhagen HJ, Raschke MJ, Laumeyer A, Hoffmann RFG (1998) Biodegradable interference screw fixation exhibits pull-out force and stiffness similar to titanium screws. Am J Sports Med 26:119–126
Woo SL-Y, Hollis JM, Adams DJ (1991) Tensile properties of the human femur–anterior cruciate ligament–tibia complex. The effect of specimen age and orientation. Am J Sports Med 19:217–225
Yasuda K, Tsujino J, Ohkoshi Y (1995) Graft site morbidity with autogenous semitendinosus and gracilis tendons. Am J Sports Med 23:706–714
Acknowledgements
We thank the fixation device manufacturers Arthrex, Arthrotek, Mitek, and Smith and Nephew for donating their products and lending their instruments for this study. The Instron machine was donated by the Arthritis Research Campaign, a UK-based charity.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Coleridge, S.D., Amis, A.A. A comparison of five tibial-fixation systems in hamstring-graft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 12, 391–397 (2004). https://doi.org/10.1007/s00167-003-0488-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-003-0488-y