Abstract
Appropriate graft tension and secure graft incorporation in bone tunnels are essential for successful anterior cruciate ligament (ACL) reconstruction using hamstring tendon autografts. Permanent viscoplastic elongation in response to cyclic loading in the early postoperative period and the interposition of suture material in the tendon–bone interface might negatively affect graft function and rigid graft incorporation in the bone tunnels. A modified Prusik knot is an alternative option to the commonly used whipstitch technique for soft tissue fixation in ACL reconstruction. This is a controlled laboratory study. Sixteen formalin-fixed human cadaver semitendinosus tendons were armed with a modified Prusik knot or a whipstitch and tested in a load-to-failure test with a constant displacement rate of 1 mm/s, 14 in the cyclic loading test with 100 cycles from 10 to 50 N followed by 100 cycles from 10 to 75 N. The modified Prusik knot showed smaller force-induced displacements and higher stiffness of the entire construct in the load-to-failure test. Smaller preconditioning displacements were the only significant differences in the cyclic loading test. The modified Prusik knot has equal or superior mechanical properties and provides a larger area in the tendon–bone interface without suture material compared with the whipstitch technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) rupture is a common knee injury. Restoration of the ACL function is very important, with ACL reconstruction using autografts currently being the preferred technique [3, 19, 22]. The most commonly used grafts are bone–patellar–tendon–bone (BPTB) and hamstring tendon autografts. BPTB grafts allow rigid fixation using interference screws and secure bone-to-bone healing [4, 7, 13, 14], whereas hamstring grafts have a lower donor-site morbidity and allow multiple bundle reconstruction [11, 12, 20].
In the early postoperative period graft fixation is the mechanically weak link within the entire system [5]. No commonly used graft fixation device has mechanical properties comparable with the intact ACL [11, 12]. Therefore, fixation methods must be rigid and stiff to withstand mechanical loading during daily activities, which are estimated as 454 N at most [17], and allow current rehabilitation principles.
It has been suggested that permanent viscoplastic elongation of the graft constructs in response to cyclic loading in the early postoperative period might negatively affect graft function [9]. It occurs in particular with the use of indirect fixation devices such as endobutton/polyester tape or screw post-fixation.
Furthermore, fixation devices of soft tissue grafts have to facilitate biologic incorporation by providing a large free contact area between tendon and bone tunnel wall [6].
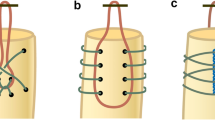
The Prusik knot is a commonly used knot in mountain climbing (Fig. 1). A modified Prusik knot may be an alternative option for tibial fixation of soft tissue grafts in ACL reconstruction. The objective of this study was the investigation of the mechanical properties of the modified Prusik knot compared to the whipstitch technique in a load-to-failure and a cyclic loading test [2].
Scheme of tying a Prusik knot (a–d). Modification of the Prusik knot implies piercing of the tendons with suture material to build the initial loop (a) instead of wrapping. Then the free ends of the suture are passed through the loop (b) followed by a subsequent loop going through the inside of the previous wrap (c). Finally, the knot is pulled tight and the wraps are neatened up (d)
Material and methods
Sixteen formalin-fixed human cadaver semitendinosus tendons were used for the load-to-failure test, 14 for the cyclic loading test. Specimens were kept moist with saline spray during all preparations and testing. The tendons were divided into two groups with the same number of tendons and equal average tendon diameters in each group.
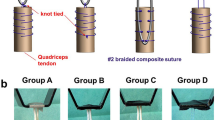
Using an Ethibond® 2.0 suture, the tendons were either armed with a whipstitch or a modified Prusik knot. Modification of the Prusik knot implied piercing of the tendons with suture material to build an initial loop instead of wrapping (Fig. 1a). When using the whipstitch technique both tendon ends were whipstitched together (Fig. 2b). Small suture loops using the same material were attached between the tendon loops and the armed part of the tendons (Fig. 2). The length of the free tendon loop (L T) was determined at 50 mm (Fig. 3). The tendon loops were wrapped around a steel bar with a diameter of 10 mm. The upper ends of the sutures were secured to the load cell of a servohydraulic material testing machine (Walter and Bai, Loehningen, Switzerland) using a custom-built clamp. The suture material was mounted between the jaws of the clamp. A small tape marker was set on the suture material next to the clamp in order to recognize potential suture slippage from the clamp.
Tendon armed with a Prusik knot (a) and a whipstitch (b). Arrows suture loop for mounting a displacement transducer. The length of the suture augmentation using the Prusik knot is approximately 5 mm (bracket) with a large area without suture augmentation. A whipstitch provides suture material over the whole extent of the tendon–bone interface
The length of the entire construct (L C) was determined at 85 mm (Fig. 3). An LVDT (Hottinger Baldwin Messtechnik GmbH, Darmstadt, Germany, maximum linearity deviation ±0.15%) was mounted at the suture loop in order to differ between the displacement of the tendon loop (ΔL T) and total displacement (ΔL C) (Fig. 3b). Residual displacement (ΔL R) was calculated by subtraction. The experimental setup was used for the load-to-failure test as well as for the cyclic loading test.
In the load-to-failure test, a preload of 10 N was applied for 1 min. The resulting length was defined as ΔL = 0. A tensile load was applied at a constant displacement rate of 1 mm/s, which is a standard testing mode for ACL fixation devices [8, 10, 16, 18, 21]. While loading the specimens, the displacements and forces were recorded with a sampling rate of 10 Hz. The following parameters were determined from the recorded data:
-
Maximum force to failure
-
Total displacement (ΔL C) at maximum force
-
Total displacement (ΔL C), displacement of the tendon loop (ΔL T) und residual displacement (ΔL R) at 50, 75 and 100 N
-
Stiffness at 50, 75 and 100 N.
Stiffness was determined by using a linear regression employing data in an interval of ±1 s when reaching forces of 50, 75 and 100 N. The slope of the regression line was defined as stiffness in N/mm. The mode of failure was also determined.
In the cyclic loading test, a preload of 10 N was applied for 1 min. The specimens were loaded accordant to a triangular force controlled loading protocol for 100 cycles from 10 to 50 N followed by 100 cycles from 10 to 75 N at a rate of 0.5 Hz (Fig. 4). This loading protocol is comparable to those of Becker [1] and Hoher [8]. While loading the specimens, the displacements and forces were recorded with a sampling rate of 10 Hz. The first five cycles were defined as preconditioning cycles. The displacement during preconditioning was recorded. The resulting length after the fifth cycle was defined as ΔL = 0. For data analysis, ΔL R displacement values of the cyclic loading test were used. Determined parameters from the recorded data are:
-
Preconditioning displacement (ΔL precon)
-
Displacement from cycle 5 to cycle 100 (ΔL 5–100)
-
Displacement from cycle 5 to cycle 200 (ΔL 5–200)
-
Displacement during cycle 100 (ΔL 100)
-
Displacement during cycle 200 (ΔL 200)
-
Displacement from the local minimum of cycle 100 to the local maximum of cycle 101 (ΔL 100–101).
All numerical data are expressed as mean and standard deviation. SPSS for Windows 12.0 (SPSS, Chicago, Illinois) was used for the statistical analysis. An unpaired Student’s t test was performed if the samples were normally distributed and the homogeneity of variance was given. Otherwise, the non-parametric Mann–Whitney U test was used. The Kolmogorov–Smirnov test was performed to determine whether the distributions differ significantly from a normal distribution. The Levene test was used for determination of the homogeneity of variances. The probability level was set at P < 0.05.
Results
Sixteen specimens were tested successfully in the load-to-failure test. Rupture of the suture material was the mode of failure in all 16 specimens with complete (10 specimens) or partial ruptures (6 specimens). In each specimen, the time of suture rupture was identical with the time of maximum force. The force–displacement curve after that incident was not further analyzed. Maximum force to failure did not significantly differ between the Prusik knot group and the whipstitch group. The modified Prusik knot was significantly stiffer at 50 N (P = 0.015), 75 N (P = 0.007) and 100 N (P = 0.018) and showed significantly smaller total displacements at 50 N (P = 0.002), 75 N (P = 0.002), 100 N (P = 0.003) and at maximum force (P = 0.028).
Fourteen specimens were tested successfully for 200 cycles in the cyclic loading test with no suture rupture or other failures. The modified Prusik knot showed smaller preconditioning displacements (P = 0.039) whereas no significant differences were found for the other parameters in the cyclic loading test. Results are summarized in Tables 1 and 2.
Discussion
Our data show that the constructs with a modified Prusik knot are significantly stiffer with smaller force-induced displacements at different force levels (50, 75, 100 N) and at maximum force in a single cycle load-to-failure test compared to the whipstitch technique. Maximum load to failure did not significantly differ between the two groups, as rupture of the suture material was the mode of failure in all 16 specimens (Table 1). The cyclic loading tests confirm these findings partially by showing a significant difference in the displacement occurring during the first five loading cycles which we have defined as preconditioning cycles (Table 2). As we used tendons with the same mean average diameter and a constant length of the tendon loop as well as the same suture material and length in both groups, we consider these findings as a result of the different suture techniques. Using the whipstitch technique may lead to permanent viscoplastic elongation of the constructs due to slippage of the suture material within the tendon tissue whereas the Prusik knot tightens under tensile load. These findings underline the importance of intraoperative graft preconditioning in order to prevent postoperative joint laxity, especially for the whipstitch technique [9]. However, in the cyclic loading test no differences in the mechanical properties after preconditioning were found, thus indicating that the mechanical behavior of the modified Prusik knot and the whipstitch are comparable, as long as a continuous load is applied to the graft. It is unknown if there are episodes in the early postoperative period with completely unloaded ACL grafts. To the author’s knowledge, there are no studies examining this question. If we assume complete unloading the modified Prusik knot may have superior mechanical properties compared to the whipstitch technique.
The long-term outcome of an ACL reconstruction depends on other important parameters. Besides isometric graft placement, rigid osseous incorporation of autografts in the tibial and femoral bone tunnel is a basic requirement [15]. Not until complete osseous integration an autograft can function as an ACL substitute. Greis [6] showed that the extent of the tendon–bone interface is an important factor for appropriate graft incorporation. Using a dog model it was shown that duplication of the free contact area between tendon and bone significantly increased the pullout strength of the extensor digitorum longus tendon in a tibial bone tunnel 6 weeks after implantation (154 vs. 266 N). To the author’s knowledge, there are no studies concerning the influence of suture material in the tendon–bone interface. Nevertheless, it is reasonable to assume that a high amount of suture material might impair healing. The length of the suture augmentation using the Prusik knot is approximately 5 mm (Fig. 2a) with a larger area without suture augmentation. A whipstitch provides suture material in the whole extent of the tendon–bone interface (Fig. 2b). Referring to this, the clinical relevance is unknown. We think that the Prusik knot improves biological incorporation of hamstring tendon autografts.
There are some limitations that need to be noted. Due to logistic and financial limitations posed on the project, we had to employ formalin-fixed tendons. Unfortunately, formalin changes the material properties of the tendon since it hardens the tissue, thus limiting a direct extrapolation to freshly harvested or even in-vivo tendons. Accordingly, data of the present study may have to be reconfirmed in a future study. Furthermore, the experimental setup of this study is a simplification of the clinical situation not considering different important clinical factors. Thus, we were able to particularly study the influence of the suture technique on the mechanical properties of the fixation devices. Therefore, further clinical and histological studies are needed to confirm that less suture material in the tendon–bone interface improves tendon-to-bone healing and the Prusik knot has equal or superior mechanical properties compared to the whipstitch technique.
References
Becker R, Schroder M, Starke C, Ropke M, Nebelung W (2000) Mechanical properties of suture materials for anchoring cruciate ligament transplants (in German). Unfallchirurg 103:375–379
Beynnon BD, Amis AA (1998) In vitro testing protocols for the cruciate ligaments and ligament reconstructions. Knee Surg Sports Traumatol Arthrosc 6:70–76
Fink C, Hoser C, Benedetto KP, Hackl W, Gabl M (1996) Long-term outcome of conservative or surgical therapy of anterior cruciate ligament rupture (in German). Unfallchirurg 99:964–969
Gerich TG, Cassim A, Lattermann C, Lobenhoffer HP (1997) Pullout strength of tibial graft fixation in anterior cruciate ligament replacement with a patellar tendon graft: interference screw versus staple fixation in human knees. Knee Surg Sports Traumatol Arthrosc 5:84–88
Goradia VK, Rochat MC, Grana WA, Egle DM (1998) Strength of ACL reconstructions using semitendinosus tendon grafts. J Okla State Med Assoc 91:275–277
Greis PE, Burks RT, Bachus K, Luker MG (2001) The influence of tendon length and fit on the strength of a tendon–bone tunnel complex. A biomechanical and histologic study in the dog. Am J Sports Med 29:493–497
Hackl W, Fink C, Benedetto KP, Hoser C (2000) Transplant fixation by anterior cruciate ligament reconstruction. Metal vs. bioabsorbable polyglyconate interference screw. A prospective randomized study of 40 patients (in German). Unfallchirurg 103:468–474
Hoher J, Livesay GA, Ma CB, Withrow JD, Fu FH, Woo SL (1999) Hamstring graft motion in the femoral bone tunnel when using titanium button/polyester tape fixation. Knee Surg Sports Traumatol Arthrosc 7:215–219
Hoher J, Scheffler SU, Withrow JD, Livesay GA, Debski RE, Fu FH, Woo SL (2000) Mechanical behavior of two hamstring graft constructs for reconstruction of the anterior cruciate ligament. J Orthop Res 18:456–461
Honl M, Carrero V, Hille E, Schneider E, Morlock MM (2002) Bone-patellar tendon-bone grafts for anterior cruciate ligament reconstruction: an in vitro comparison of mechanical behavior under failure tensile loading and cyclic submaximal tensile loading. Am J Sports Med 30:549–557
Kousa P, Jarvinen TL, Vihavainen M, Kannus P, Jarvinen M (2003a) The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part I: femoral site. Am J Sports Med 31:174–181
Kousa P, Jarvinen TL, Vihavainen M, Kannus P, Jarvinen M (2003b) The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part II: tibial site. Am J Sports Med 31:182–188
Kurosaka M, Yoshiya S, Andrish JT (1987) A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med 15:225–229
Matthews LS, Lawrence SJ, Yahiro MA, Sinclair MR (1993) Fixation strengths of patellar tendon–bone grafts. Arthroscopy 9:76–81
Nebelung W, Becker R, Urbach D, Ropke M, Roessner A (2003) Histological findings of tendon–bone healing following anterior cruciate ligament reconstruction with hamstring grafts. Arch Orthop Trauma Surg 123:158–163
Novak PJ, Wexler GM, Williams JS Jr, Bach BR Jr, Bush-Joseph CA (1996) Comparison of screw post fixation and free bone block interference fixation for anterior cruciate ligament soft tissue grafts: biomechanical considerations. Arthroscopy 12:470–473
Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS (1984) Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 66:344–352
Robert H, Es-Sayeh J, Heymann D, Passuti N, Eloit S, Vaneenoge E (2003) Hamstring insertion site healing after anterior cruciate ligament reconstruction in patients with symptomatic hardware or repeat rupture: a histologic study in 12 patients. Arthroscopy 19:948–954
Seitz H, Chrysopoulos A, Egkher E, Mousavi M (1994) Long-term results of replacement of the anterior cruciate ligament in comparison with conservative therapy (in German). Chirurg 65:992–998
Weiler A, Hoffmann RF, Stahelin AC, Bail HJ, Siepe CJ, Sudkamp NP (1998a) Hamstring tendon fixation using interference screws: a biomechanical study in calf tibial bone. Arthroscopy 14:29–37
Weiler A, Windhagen HJ, Raschke MJ, Laumeyer A, Hoffmann RF (1998b) Biodegradable interference screw fixation exhibits pull-out force and stiffness similar to titanium crews. Am J Sports Med 26:119–126
Wittenberg RH, Oxfort HU, Plafki C (1998) A comparison of conservative and delayed surgical treatment of anterior cruciate ligament ruptures. A matched pair analysis. Int Orthop 22:145–148
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krappinger, D., Kralinger, F.S., Attal, R.E. et al. Modified Prusik knot versus whipstitch technique for soft tissue fixation in anterior cruciate ligament reconstruction: a biomechanical analysis. Knee Surg Sports Traumatol Arthrosc 15, 418–423 (2007). https://doi.org/10.1007/s00167-006-0176-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-006-0176-9