Abstract
Objective
To describe current use and diagnostic and therapeutic impacts of point-of-care ultrasound (POCUS) in the intensive care unit (ICU).
Background
POCUS is of growing importance in the ICU. Several guidelines recommend its use for procedural guidance and diagnostic assessment. Nevertheless, its current use and clinical impact remain unknown.
Methods
Prospective multicentric study in 142 ICUs in France, Belgium, and Switzerland. All the POCUS procedures performed during a 24-h period were prospectively analyzed. Data regarding patient condition and the POCUS procedures were collected. Factors associated with diagnostic and therapeutic impacts were identified.
Results
Among 1954 patients hospitalized during the study period, 1073 (55 %) POCUS/day were performed in 709 (36 %) patients. POCUS served for diagnostic assessment in 932 (87 %) cases and procedural guidance in 141 (13 %) cases. Transthoracic echocardiography, lung ultrasound, and transcranial Doppler accounted for 51, 17, and 16 % of procedures, respectively. Diagnostic and therapeutic impacts of diagnostic POCUS examinations were 84 and 69 %, respectively. Ultrasound guidance was used in 54 and 15 % of cases for central venous line and arterial catheter placement, respectively. Hemodynamic instability, emergency conditions, transthoracic echocardiography, and ultrasounds performed by certified intensivists themselves were independent factors affecting diagnostic or therapeutic impacts.
Conclusions
With regard to guidelines, POCUS utilization for procedural guidance remains insufficient. In contrast, POCUS for diagnostic assessment is of extensive use. Its impact on both diagnosis and treatment of ICU patients seems critical. This study identified factors associated with an improved clinical value of POCUS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prompt diagnosis and early treatments are essential in intensive care unit (ICU) patients [1]. During the last few years, several guidelines have recommended using ultrasound for procedural guidance and diagnostic assessment [2–4]. Ultrasound can rapidly provide relevant information at the bedside [5].
As demonstrated in several monocentric studies, transthoracic echocardiography improves the performance of clinical cardiac examination [6–9]. Analogous results were obtained for pulmonary examination. Several studies showed that lung ultrasound performs better than chest radiograph [10, 11] and reduces the need for irradiative procedures [12]. In addition, the use of ultrasound was associated with up to 50 % change of patient management [6–10].
Previous studies defined point-of-care ultrasound (POCUS) as ultrasonography brought to the patient and performed by the provider [13–16]. POCUS aims to avoid delays in diagnosis and treatment initiation [17]. However, in the ICU, the actual levels of POCUS implementation and contribution to patient management remain unknown. The primary aim of our study was to evaluate the prevalence of POCUS use in ICU patients. The secondary aims were to assess the diagnostic performance and therapeutic impact of POCUS in a large cohort of ICU patients. Finally, we assessed the factors that may influence the performance of POCUS.
Materials and methods
Study design
This 1-day, prospective, observational study was approved by the institutional review board (IRB) (Nîmes, France, 13/04-0208/27/2013) and the Commission Nationale de l’Informatique et des Libertés (DE-20146005, 01/30/2014). The IRB waived the need for patient (or relative) consent. Local IRBs in other participating countries also approved the trial with waived consent.
Using several networks including AzuRea and CAR’Echo, we invited representatives of 160 ICUs to participate to the study. We recruited units from France, Switzerland, and Belgium. The representatives of 142 (89 %) ICUs accepted the invitation. The representatives of each unit prospectively collected all the ultrasound exams that were performed in their units during a 24-h period starting on 11December 2014 at 8 a.m. There was no incentive to perform POCUS that day. Apart from the local coordinator, the other doctors participating in the trial were not aware of the goals of the trial. During the study, each operator performing an ultrasound examination filled in a case report form. Details on operator training, patient conditions, type of ultrasound, diagnosis, treatment changes, and timing of assessment were reported in the case report form. The day after the study, each investigator collected the total number of patients hospitalized and the total number of central venous line (CVC) or arterial line (A-line) placements. The case report forms are available in the Electronic Supplemental Material.
Definitions
The prevalence of POCUS was defined as the number of POCUS/number of patients hospitalized in the unit during the study period. The POCUS were classified into “procedural guidance” (ultrasound was used for an invasive procedure) or “diagnostic assessment” in the other cases [13]. We studied diagnostic and therapeutic impact as well as clinical value of POCUS in the “diagnostic assessment POCUS” group. “Procedural guidance POCUS” was excluded from this analysis. The “diagnostic impact” was defined as an ultrasound-induced confirmation or change in the current diagnosis according to the physician who performed the examination. The “therapeutic impact” was defined as an ultrasound-induced change in treatment and/or imaging ordering and/or patient triage according to the physician who performed the POCUS. These variables were determined during the study period. The “global clinical value” was defined as the combination of either the diagnostic impact or therapeutic impact [18]. An emergent ultrasound was defined as a POCUS performed in the first hour after the occurrence of the first clinical sign. We classified POCUS performed at ICU admission, during the hospitalization, during the day shift (from 8 a.m. to 6 p.m.), and during the night shift (6 p.m. to 8 a.m.). The operator classified the quality of images obtained for each procedure as good (full visualization of structures), average (partial visualization allowing assessment), or poor (no visualization or no possible assessment).
A trained physician was defined as a specialist skilled in a given procedure (cardiologists for echocardiography, radiologists for the other types of ultrasound evaluations). For intensivists, a certified physician was defined as an intensivist who received specific training in critical care echography, according to international guidelines [19]. Ultrasound guidance rates for CVC and A-line were defined as the ratio of the total number of CVC or A-line placements divided by the number of ultrasound-guided placements.
Statistical analysis
Statistical analysis was performed using R-Project 3.1 for GNU Linux Ubuntu (Vienna, Austria). For categorical variables, percentages were computed. Comparisons of percentages were performed with Fisher’s exact test. We performed a multivariate analysis to assess the independent factors of therapeutic and diagnostic impact. Variables with a significance level at least 0.1 were included in the logistic regression model. The variables were selected by a step-by-step forward–backward model to minimize the Akaike’s criterion. The statistical threshold for final significance was 0.05.
Results
During the study day, 1073 (55 %) POCUS were performed in 709 (36 %) out of 1954 patients hospitalized in the 142 ICUs. The quality of images was classified as good, average, and poor for 794 (74 %), 236 (22 %), and 43 (4 %) POCUS, respectively. Features of patients and units are sumarized in Table 1.
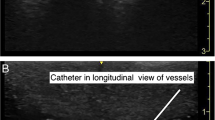
The use of POCUS was aimed at assessing diagnosis in 932 (87 %) cases and procedural guidance in 141 (13 %) cases (Fig. 1). The diagnostic and therapeutic impacts were 84 and 69 %, respectively (Fig. 2). The clinical value combining either the diagnostic impact or the therapeutic impact was assessed at 85 %. With respect to diagnostic impact, the use of POCUS confirmed or changed the diagnosis in 63 and 21 % of cases, respectively. Heart, lung, brain, and miscellaneous other sites represented 51, 17, 16, and 16 % of POCUS, respectively (Fig. 2). Performing POCUS resulted in the initiation of 373 therapeutic interventions, the decision to stop interventions in 73 cases, or not to perform additional examinations in 108 cases (Fig. 1); (Table 2). Hemodynamic interventions including fluid bolus (n = 115), fluid depletion (n = 80), and catecholamine administration (n = 43) were the most prominent POCUS-driven interventions. With respect to 183 central venous line placements and 127 arterial catheter placements, POCUS was used in 99 (54 %) cases and 15 (13 %) cases, respectively.
The factors associated with diagnostic and therapeutic impacts in the univariate analysis are shown in Table 3. In the multivariate analysis, being a certified operator, managing a shocked patient, having a disinfection protocol, and using an algorithm of management were associated with significant changes in the diagnostic impact (Table 3). Being an intensivist, having a daily practice, assessing a child, processing in emergency, working in a university hospital, and transthoracic echocardiography were independent variables associated with therapeutic impact (Table 3).
Discussion
In this large 1-day observational trial we observed that at least one POCUS is performed in one-third of the patients hospitalized in the ICU that day and that it impacted patient management in 85 % of cases.
POCUS was used in 36 % of our patients/day. Even though ICU guidelines recommend a large use of POCUS [2, 4, 19], the prevalence of POCUS use has been poorly described. Only a few monocentric studies assessed the performance of POCUS in ICUs [6, 7, 9, 10, 20]. A previous French survey showed that in the majority of ICUs echocardiography was used about once a day [21]. Interestingly, intensivists performed POCUS in 90 % of cases. This finding confirms the good diffusion of this technique among intensivists. In addition, more than 80 % of operators were board-certified and used ultrasound on a daily basis.
A diagnostic impact was reported in 84 % of cases. The use of POCUS changed the diagnosis in 21 % of cases, while a suspected diagnosis was confirmed in 63 % of cases. This striking result highlights the emergence of POCUS as a diagnostic tool at the bedside. We did not collect the specific diagnosis. However, as transthoracic echocardiography represented more than 50 % of POCUS, our study underlines that ultrasounds play a key role for the hemodynamic management of ICU patients.
In 69 % of cases, the use of POCUS was associated with interventions including treatment, imagery ordering, and patient triage. In line with the diagnostic impact, most interventions were related to hemodynamics, underlining once again the key role of transthoracic echocardiography. Fluid loading, fluid depletion, and vasopressor administration were among the most frequent interventions. Several studies showed that hemodynamic-related interventions based on echocardiography are efficient [22–25]. Elsewhere, Aliaga et al. reported 54 % of therapeutic changes after chest computed tomography [26]. However, the type of expectations probably differs between POCUS and computed tomography scan.
In our study, cardiac examination was the most common indication for POCUS. Transthoracic echocardiograhy has been associated with improvement of diagnosis in patients with acute respiratory failure and/or shock [6–8, 27] and is now recommended in guidelines [28]. In our cohort, lung ultrasound was the second most common type of POCUS used. The steep learning curve favors the use of this procedure, which provides interesting information about pleura, parenchyma, and lung aeration state in critical situations [10, 29–31]. Lung ultrasound was associated with reduced requirements for chest radiographs and computed tomography. This shift was associated with a decreased amount of irradiation and medical cost [12, 32]. In recent studies, a global approach combining heart and lung assessment improved diagnostic performance [27, 33]. Thus, one may expect a larger use of this promising technique. The gap between echocardiography and lung ultrasound probably reflects the differences in the penetration rate of the two techniques. Recent guidelines should reduce this gap [2, 34]. In our study, transcranial Doppler was the third most common type of POCUS used. Transcranial Doppler aimed to monitor cerebral hemodynamics, as an alternative or complement to intracranial pressure monitoring [22, 23].
POCUS was used to guide procedures in less than 15 % of indications. Only half of CVC insertions were ultrasound-guided, despite a strong level of evidence and recommendations for using ultrasound guidance during CVC placement [4]. This result is surprising since an ultrasound device was available in all the units. Ultrasound was used in 15 % for the placement of A lines. This procedure is supported by guidelines with a strong level of evidence [35]. Therefore our results show that, in the study group of ICUs, compliance with this recommendation can be improved.
Finally, we identified independent factors associated with the diagnostic and therapeutic impacts. Operator experience (trained or certified physician), disinfection protocol, and presence of shock were associated with increased diagnostic impact. The disinfection protocol may be an indirect marker of appropriate use of POCUS and quality of care. The operator’s experience probably reflects a certain level of expertise. With respect to shock management, several studies reported the performance of ultrasound in those patients [21, 26]. In terms of diagnostic impact, having pre-established therapeutic algorithms was associated with reduced performance. In our opinion, this result reflects the challenge to show the relevance of algorithms in ICU patients [36, 37]. With respect to therapeutic impact, our results showed that being an intensivist, having a routine use of POCUS, and performing an emergency POCUS were associated with an increased impact. Those findings suggest that at the bedside POCUS facilitates the intensivist’s decision-making process. This also encourages the development of specific training for intensivists [38]. Unsurprisingly, transthoracic echocardiography also has a stronger therapeutic impact than other procedures. Hemodynamic assessment represented more than half of the interventions, probably explaining these associations.
Our study has several limitations. Although this was not requested, only units with an available ultrasound device participated. This represents probably an intrinsic bias of recruitment. In addition, we conducted the study in Belgium, Switzerland, and France. As we cannot determinate the rate of uptake of POCUS in other countries, it is difficult to determine how our findings are able to be extrapolated elsewhere. As the study was open, the investigators were aware of the study day. Therefore, they may have been encouraged to use the POCUS during the study day. However, this deviation should result in decreased rates of diagnostic and therapeutic impacts, which are high in our study. Moreover, the impact of ultrasound on the medical decision was also determined by the operator. In relation to our aims, the loss of data would have been a bias exceeding that of the non-blinded assessment. In terms of diagnosis and treatment, POCUS was not compared with a standard of care. Nevertheless, this process was confirmed in several previous studies [6, 7, 10, 11]. Finally, our study was not aimed at assessing the appropriateness of interventions and the patient outcomes. Our goal was to determine the use of POCUS in real life.
Our study clearly shows the high prevalence of POCUS use in ICUs. Moreover, we showed that POCUS is not an observational game but strongly impacts the management of the most critically ill patients. Intensivists acquired adequate skills for using ultrasound at the bedside. Future efforts should stress the placement of intravascular lines using ultrasound.
References
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R, Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup (2013) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, Melniker L, Gargani L, Noble VE, Via G, Dean A, Tsung JW, Soldati G, Copetti R, Bouhemad B, Reissig A, Agricola E, Rouby JJ, Arbelot C, Liteplo A, Sargsyan A, Silva F, Hoppmann R, Breitkreutz R, Seibel A, Neri L, Storti E, Petrovic T (2012) International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS). Intensive Care Med 38:577–591
Bouzat P, Francony G, Declety P, Genty C, Kaddour A, Bessou P, Brun J, Jacquot C, Chabardes S, Bosson JL, Payen JF (2011) Transcranial Doppler to screen on admission patients with mild to moderate traumatic brain injury. Neurosurgery 68:1603–1610
Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, Reeves ST; Councils on Intraoperative Echocardiography and Vascular Ultrasound of the American Society of Echocardiography (2011) Guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr 24:1291–1318
Laursen CB, Sloth E, Lambrechtsen J, Lassen AT, Madsen PH, Henriksen DP, Davidsen JR, Rasmussen F (2013) Focused sonography of the heart, lungs, and deep veins identifies missed life-threatening conditions in admitted patients with acute respiratory symptoms. Chest 144:1868–1875
Joseph MX, Disney PJS, Da Costa R, Hutchison SJ (2004) Transthoracic echocardiography to identify or exclude cardiac cause of shock. Chest 126:1592–1597
Orme RML, Oram MP, McKinstry CE (2009) Impact of echocardiography on patient management in the intensive care unit: an audit of district general hospital practice. Br J Anaesth 102:340–344
Bossone E, DiGiovine B, Watts S, Marcovitz PA, Carey L, Watts C, Armstrong WF (2002) Range and prevalence of cardiac abnormalities in patients hospitalized in a medical ICU. Chest 122:1370–1376
Manno E, Navarra M, Faccio L, Motevallian M, Bertolaccini L, Mfochivè A, Pesce M, Evangelista A (2012) Deep impact of ultrasound in the intensive care unit: the “ICU-sound” protocol. Anesthesiology 117:801–809
Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ (2004) Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology 100:9–15
Xirouchaki N, Magkanas E, Vaporidi K, Kondili E, Plataki M, Patrianakos A, Akoumianaki E, Georgopoulos D (2011) Lung ultrasound in critically ill patients: comparison with bedside chest radiography. Intensive Care Med 37:1488–1493
Peris A, Tutino L, Zagli G, Batacchi S, Cianchi G, Spina R, Bonizzoli M, Migliaccio L, Perretta L, Bartolini M, Ban K, Balik M (2010) The use of point-of-care bedside lung ultrasound significantly reduces the number of radiographs and computed tomography scans in critically ill patients. Anesth Analg 111:687–692
Moore CL, Copel JA (2011) Point-of-care ultrasonography. N Engl J Med 364:749–757
Vignon P, Dugard A, Abraham J, Belcour D, Gondran G, Pepino F, Marin B, François B, Gastinne H (2007) Focused training for goal-oriented hand-held echocardiography performed by noncardiologist residents in the intensive care unit. Intensive Care Med 33:1795–1799
Chalumeau-Lemoine L, Baudel JL, Das V, Arrivé L, Noblinski B, Guidet B, Offenstadt G, Maury E (2009) Results of short-term training of naïve physicians in focused general ultrasonography in an intensive-care unit. Intensive Care Med 35:1767–1771
Carrié C, Biais M, Lafitte S, Grenier N, Revel P, Janvier G (2014) Goal-directed ultrasound in emergency medicine: evaluation of a specific training program using an ultrasonic stethoscope. Eur J Emerg Med. doi:10.1097/MEJ.0000000000000172
Oks M, Cleven KL, Cardenas-Garcia J, Schaub JA, Koenig S, Cohen RI, Mayo PH, Narasimhan M (2014) The effect of point-of-care ultrasonography on imaging studies in the medical ICU: a comparative study. Chest 146:1574–1577
Lakhal K, Serveaux-Delous M, Lefrant JY, Capdevila X, Jaber S, AzuRéa network for the RadioDay study group (2012) Chest radiographs in 104 French ICUs: current prescription strategies and clinical value (the RadioDay study). Intensive Care Med 38:1787–1799
Mayo PH, Beaulieu Y, Doelken P, Feller-Kopman D, Harrod C, Kaplan A, Oropello J, Vieillard-Baron A, Axler O, Lichtenstein D, Maury E, Slama M, Vignon P (2009) American College of Chest Physicians/La Société de Réanimation de Langue Française statement on competence in critical care ultrasonography. Chest 135:1050–1060
Volpicelli G, Lamorte A, Tullio M, Cardinale L, Giraudo M, Stefanone V, Boero E, Nazerian P, Pozzi R, Frascisco MF (2013) Point-of-care multiorgan ultrasonography for the evaluation of undifferentiated hypotension in the emergency department. Intensive Care Med 39:1290–1298
Quintard H, Philip I, Ichai C (2011) French survey on current use of ultrasound in the critical care unit: ECHOREA. Ann Fr Anesth Reanim 30:e69–73
Feissel M, Michard F, Faller JP, Teboul JL (2004) The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med 30:1834–1837
Muller L, Toumi M, Bousquet PJ, Riu-Poulenc B, Louart G, Candela D, Zoric L, Suehs C, de La Coussaye JE, Molinari N, Lefrant JY; AzuRéa Group (2011) An increase in aortic blood flow after an infusion of 100 ml colloid over 1 minute can predict fluid responsiveness: the mini-fluid challenge study. Anesthesiology 115:541–547
Lamia B, Ochagavia A, Monnet X, Chemla D, Richard C, Teboul JL (2007) Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med 33:1125–1132
Brun C, Zieleskiewicz L, Textoris J, Muller L, Bellefleur JP, Antonini F, Tourret M, Ortega D, Vellin A, Lefrant JY, Boubli L, Bretelle F, Martin C, Leone M (2013) Prediction of fluid responsiveness in severe preeclamptic patients with oliguria. Intensive Care Med 39:593–600
Aliaga M, Forel JM, De Bourmont S, Jung B, Thomas G, Mahul M, Bisbal M, Nougaret S, Hraiech S, Roch A, Chaumoitre K, Jaber S, Gainnier M, Papazian L (2015) Diagnostic yield and safety of CT scans in ICU. Intensive Care Med 41:436–443
Bataille B, Riu B, Ferre F, Moussot PE, Mari A, Brunel E, Ruiz J, Mora M, Fourcade O, Genestal M, Silva S (2014) Integrated use of bedside lung ultrasound and echocardiography in acute respiratory failure: a prospective observational study in ICU. Chest 146:1586–1593
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, Jaeschke R, Mebazaa A, Pinsky MR, Teboul JL, Vincent JL, Rhodes A (2014) Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med 40:1795–1815
Bouhemad B, Brisson H, Le-Guen M, Arbelot C, Lu Q, Rouby JJ (2011) Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med 183:341–347
Bouhemad B, Liu ZH, Arbelot C, Zhang M, Ferarri F, Le-Guen M, Girard M, Lu Q, Rouby JJ (2010) Ultrasound assessment of antibiotic-induced pulmonary reaeration in ventilator-associated pneumonia. Crit Care Med 38:84–92
Volpicelli G, Melniker LA, Cardinale L, Lamorte A, Frascisco MF (2013) Lung ultrasound in diagnosing and monitoring pulmonary interstitial fluid. Radiol Med 118:196–205
Zieleskiewicz L, Cornesse A, Hammad E, Haddam M, Brun C, Vigne C, Meyssignac B, Remacle A, Chaumoitre K, Antonini F, Martin C, Leone M (2015) Implementation of lung ultrasound in polyvalent intensive care unit: impact on irradiation and medical cost. Anaesth Crit Care Pain Med 34:41–44
Laursen CB, Sloth E, Lassen AT, Christensen Rd, Lambrechtsen J, Madsen PH, Henriksen DP, Davidsen JR, Rasmussen F (2014) Point-of-care ultrasonography in patients admitted with respiratory symptoms: a single-blind, randomised controlled trial. Lancet Respir Med 2:638–646
Georgopoulos D, Xirouchaki N, Volpicelli G (2014) Lung ultrasound in the intensive care unit: let’s move forward. Intensive Care Med 40:1592–1594
Hansen MA, Juhl-Olsen P, Thorn S, Frederiksen CA, Sloth E (2014) Ultrasonography-guided radial artery catheterization is superior compared with the traditional palpation technique: a prospective, randomized, blinded, crossover study. Acta Anaesthesiol Scand 58:446–452
ARISE Investigators, ANZICS Clinical Trials Group, Peake SL, Delaney A, Bailey M, Bellomo R, Cameron PA, Cooper DJ, Higgins AM, Holdgate A, Howe BD, Webb SA, Williams P (2014) Goal-directed resuscitation for patients with early septic shock. N Engl J Med 371:1496–1506
Investigators ProCESS, Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, Pike F, Terndrup T, Wang HE, Hou PC, LoVecchio F, Filbin MR, Shapiro NI, Angus DC (2014) A randomized trial of protocol-based care for early septic shock. N Engl J Med 370:1683–1693
Expert Round Table on Echocardiography in ICU (2014) International consensus statement on training standards for advanced critical care echocardiography. Intensive Care Med 40:654–666
Acknowledgments
Author contributions: Drs Zieleskiewicz and Leone had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Arbelot, Chaumoitre, Cholley, Constantin, Jaber, Lakhal, Leone, Martin, Perbet, Zieleskiewicz.
Acquisition, analysis or interpretation of data: Arbelot, Bouhemad, Demory, M. Muller, L. Muller, Cholley, Duperret, Hammad, Langeron, Mahjoub, Maury, Meaudre, Michel, Nafati, Quintard, Bertrand, Guervilly, Jaber, Riu, Perbet.
Drafting of the manuscript: Lakhal, Meresse, De Backer, Leone, Allaouchiche, Zieleskiewicz, L Muller, Ichai, Lefrant.
Statistical analysis: Antonini, Leone, Meresse, Vigne, Zieleskiewicz.
Study supervision: Martin, Leone, De Backer, Chaumoitre.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: In the intensive care unit, the prevalence of point-of-care ultrasound was 55 %. Ultrasound was utilized for diagnostic assessment in 87 % of cases and procedural guidance in 13 % of cases; its use impacted diagnostic and therapeutic strategies in 84 and 69 % of cases. Transthoracic echocardiography and lung ultrasound were routinely performed by intensivists. In contrast, ultrasound guidance for central venous line and arterial catheter placement remains unsatisfactory.
For the CAR’Echo and AzuRea Collaborative Networks
c/o M. Leone, Département d’anesthésie et de réanimation, Hôpital Nord, Marseille, France.
Members of the CAR’Echo and AzuRea Collaborative Networks are listed in the Acknowledgments.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Members of the CAR’Echo and AzuRea Collaborative Networks
Members of the CAR’Echo and AzuRea Collaborative Networks
Table 4 presents a list of members of the CAR’Echo and AzuRea Collaborative Networks.
Rights and permissions
About this article
Cite this article
Zieleskiewicz, L., Muller, L., Lakhal, K. et al. Point-of-care ultrasound in intensive care units: assessment of 1073 procedures in a multicentric, prospective, observational study. Intensive Care Med 41, 1638–1647 (2015). https://doi.org/10.1007/s00134-015-3952-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-3952-5