Abstract
Purpose
We analyzed the efficacy of a point-of-care ultrasonographic protocol, based on a focused multiorgan examination, for the diagnostic process of symptomatic, non-traumatic hypotensive patients in the emergency department.
Methods
We prospectively enrolled 108 adult patients complaining of non-traumatic symptomatic hypotension of uncertain etiology. Patients received immediate point-of-care ultrasonography to determine cardiac function and right/left ventricle diameter rate, inferior vena cava diameter and collapsibility, pulmonary congestion, consolidations and sliding, abdominal free fluid and aortic aneurysm, and leg vein thrombosis. The organ-oriented diagnoses were combined to formulate an ultrasonographic hypothesis of the cause of hemodynamic instability. The ultrasonographic diagnosis was then compared with a final clinical diagnosis obtained by agreement of three independent expert physicians who performed a retrospective hospital chart review of each case.
Results
Considering the whole population, concordance between the point-of-care ultrasonography diagnosis and the final clinical diagnosis was interpreted as good, with Cohen’s k = 0.710 (95 % CI, 0.614–0.806), p < 0.0001 and raw agreement (Ra) = 0.768. By eliminating the 13 cases where the final clinical diagnosis was not agreed upon (indefinite), the concordance increased to almost perfect, with k = 0.971 (95 % CI, 0.932–1.000), p < 0.0001 and Ra = 0.978.
Conclusions
Emergency diagnostic judgments guided by point-of-care multiorgan ultrasonography in patients presenting with undifferentiated hypotension significantly agreed with a final clinical diagnosis obtained by retrospective chart review. The integration of an ultrasonographic multiorgan protocol in the diagnostic process of undifferentiated hypotension has great potential in guiding the first-line therapeutic approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A differential diagnosis is a systematic procedure that allows physicians to identify a condition where multiple alternatives are possible. In case of medical emergencies, there may not be enough time to perform detailed diagnostic procedures, in which case the main purpose of a differential diagnosis is to eliminate any imminently life-threatening conditions from the possibilities. Point-of-care ultrasonography in the hands of the clinician is a safe, rapid, non-invasive diagnostic technique, suitable for use at the bedside, that can help physicians to solve time-dependent focused clinical puzzles and greatly accelerate the differential diagnostic procedure [1]. The potential use of point-of-care ultrasonography in emergency care is growing rapidly and has been undergoing continuous innovation in recent years. Examples of these innovations are implementation of a focused cardiac and lung ultrasonography evaluation in the procedures for the early diagnosis in extreme emergencies [2]. Particularly lung sonography represents a novelty in the hemodynamic evaluation and monitoring of the critically ill [3, 4].
Undifferentiated hypotension is a common condition in the emergency department (ED), recognized as a strong predictor of in-hospital mortality [5, 6]. A safe and early goal-directed supportive treatment of hypotensive patients depends on identification of possible etiologies and a prompt exclusion of the most severe and rapidly fatal conditions. Point-of-care ultrasonography plays an important role in the diagnostic procedure of undifferentiated hypotension in the emergency setting. Some protocols consisting of goal-directed ultrasonographic evaluations that integrate cardiac, abdominal and venous examinations have already been proposed and validated [7–9]. Some review articles have already introduced the adjunct of a lung evaluation to the multiorgan ultrasonographic diagnostic procedure of undifferentiated hypotension and shock, but this has not been validated by prospective patient studies [10–14].
The purpose of the present study was to validate a rapid focused ultrasonographic protocol that incorporates a bedside stepped examination of the heart, inferior vena cava, lung, abdomen and leg veins as part of a point-of-care examination for an early approach to non-traumatic undifferentiated hypotension in emergency care. The hypothesis of the study is that early diagnostic predictions guided by ultrasonography would significantly agree with retrospective diagnoses performed by chart review by three independent expert clinicians. A secondary objective is to evaluate the number of cases where lung examination, incorporated in a multiorgan ultrasonographic protocol, is decisive in obtaining a definite diagnosis.
Methods
Enrollment
We prospectively enrolled 114 patients from May 2011 to December 2012 in the Emergency Department (ED) of San Luigi Gonzaga University Hospital in Torino, Italy, an urban 400-bed teaching hospital. The ED serves the population of the west part of the town with >48,000 visits per year. Criteria for enrollment included the following: (1) age >18 years and <95 years; (2) systolic blood pressure stably <100 mmHg at presentation, confirmed after at least three measurements during the first evaluation; (3) presence of at least one of the following signs or symptoms of hypoperfusion: unresponsiveness, altered mental status (including unexplained severe anxiety), syncope, respiratory distress, profound asthenia with fatigue and malaise, and severe chest or abdominal pain. Patients were excluded from the study in case of: (1) a usual “low blood pressure” state reported by the patient or recorded in the history; (2) resuscitation maneuvers, with or without the use of defibrillation or ALS medications, before enrollment and invasive ventilation; (3) severe abdominal or thoracic trauma in the 24 h before enrollment; (4) ST elevation myocardial infarction at the electrocardiogram or clear clinical signs of probable non-ST elevation myocardial infarction; (5) a clear cause of shock diagnosed before the ultrasonographic evaluation, mandating prompt life-saving treatment, such as external bleeding, active gastrointestinal bleeding, or drug overdose; (6) onset of signs and symptoms of shock during the hospital stay or in the ED after the initial evaluation. Criteria for inclusion and exclusion were blindly evaluated by at least two independent physicians at presentation, the attending physician and the ultrasonography operator, and only in case of perfect concordance did we proceed with enrollment. Initial arterial blood pressure was measured in the ED triage area or upon arrival in the shock room of the high-acuity section of the ED and then monitored by an automated oscillometric device, Solar 8000M (GE Healthcare, Milwaukee, WI, USA). The study protocol was reviewed and approved by the local Institutional Review Board (no. 182/2012) and the study registered at ClinicalTrials.gov (NCT01572571); it was therefore performed in accordance with ethical standards. A delayed written informed consent for the use of personal data was signed at a time when the patients were deemed competent. Next of kin participated in the informed consent procedure when needed. All patients immediately received standard diagnostic emergent interventions including physical examination, intravenous access for whole blood assays, arterial gas analysis, electrocardiography, continuous cardiac monitoring, supplemental oxygen and supine chest radiography.
Ultrasonography technique
A point-of-care ultrasonographic examination is routinely performed in all unstable patients in our ED. For the purpose of the present study, an independent physician, unaware of all the other diagnostic tests and aware of visible physical signs and symptoms, performed the ultrasonographic evaluation immediately upon arrival. The operator recorded the presence or absence of ultrasonographic findings using an explicit list (Table 1). Then, based on a combination of ultrasonographic signs, the operator chose the diagnosis of the probable condition causing hypotension from a list of nine possible ultrasonographic patterns (Table 2). All goal-directed ultrasonographic studies were performed in two-dimensional grayscale with the patient in a supine to 30° upright position using a Esaote MyLab 40 ultrasound system (Esaote Italia, Milan, Italy). The operator was a board-certified emergency physician with specific competence in emergency ultrasonography, performing about 400 emergency studies per year for no less than 5 years.
The standardized multiorgan ultrasonographic protocol consisted of study of the heart, inferior vena cava, lung, leg veins and abdomen using the views listed below.
Cardiac views
A cardiac phased array 2–4-MHz probe was used for study of the heart through the subcostal, parasternal long axis and the apical four-chamber views. The subcostal four-chamber view was examined for fluid collection within the pericardial sac, right atrium/ventricle (RV) diastolic collapse, left ventricle (LV) impaired function by visual estimation of gross wall contraction and wall thickening, or LV hyperkinesia with impaired filling, RV dilation (RV/LV end diastolic diameter >0.7) and visual estimation of impaired function [15–17]. At least one of the other two cardiac views was used in case of doubtful diagnosis, difficult visualization and confirmation of RV dilation. The parasternal long axis was examined for pericardial effusion, visual estimation of qualitative LV function and signs of RV dilation (RV/LV end diastolic diameter >0.7) [17]. The apical four-chamber view was examined for pericardial effusion, qualitative LV function and signs of RV dilation (RV/LV end diastolic diameter >0.9) [18–20].
Lung views
The same probe used for cardiac study or, alternatively, a curvilinear 2–5-MHz probe was used for intercostal lung views (oblique scans). Fundamental ultrasonographic signs were considered multiple B-lines, subpleural consolidations, air bronchograms and lung sliding. The standardized eight anterior-lateral area examination was used [21]. Absence of multiple B-lines with regular sliding is the “A pattern,” which is a sign of normally aerated or hyperinflated lungs and rules out pulmonary edema and pneumothorax. Multiple B lines on at least two scans per side represent the “B pattern,” a sign of diffuse interstitial syndrome. This condition indicates cardiogenic pulmonary congestion or, alternatively, lesional edema in ARDS, pulmonary fibrosis and interstitial pneumonia [22]. Detection of multiple B lines limited to less than two scans per side or limited to one side is the “A/B pattern,” a sign of focal interstitial syndrome. This condition indicates focal interstitial involvement around isolated pulmonary consolidations, such as pneumonia, infarction and contusion [3]. Pulmonary consolidations with air bronchograms indicate consolidative processes of the lung, very often due to pneumonia [23, 24]. The examination was also extended to the dorsal areas to visualize possible posterior consolidations. Respiratory lung sliding was also checked, and its absence with the absence of B-lines, lung pulsation and images of consolidation was considered a sign of tension pneumothorax [25]. For brevity, in the text and tables this set of signs is indicated “no sliding.” Diagnostic criteria corresponded to the recommendations of the recent consensus conference on lung ultrasound [21].
Inferior vena cava views
The subcostal view was used for long axis visualization of the proximal inferior vena cava (IVC) to measure maximum diameter, estimate the percent of respiratory collapsibility (caval index) and visualization of intraluminal thrombosis. The same probe used for cardiac views or, alternatively, a curvilinear 2–5-MHz probe was used. All measurements were made no less than 2 cm caudal from the junction of the right atrium [26]. The pattern considered significant for central venous pressure (CVP) >10 mmHg coincided with diameter >2 cm and absent or reduced (<40 %) collapsibility, while low CVP (<5 mm Hg) was diagnosed with diameter <2 cm and total or enhanced collapsibility (>50 %) [27, 28]. All the intermediate conditions were considered not diagnostic. A third condition interpreted as a sign of acute overload was visualization of spontaneous echo contrast (sludge) or solid echogenic thrombi [29].
Abdominal views
Free fluids were estimated by a curvilinear 2–5-MHz probe as detection of anechoic free spaces in the traditional peritoneal pouch [30]. The anterior-posterior diameter of the abdominal aorta was measured in the short axis view, and a measurement >30 mm was considered a sign of dilation [31].
Leg vein views
The common femoral and popliteal leg veins were examined for collapsibility in the short axis using a linear 7–12-MHz probe. Absence of collapsibility was considered diagnostic for intraluminal thrombosis [32]. In case of a negative examination but strong suspicion of thrombosis, the bilateral venous waveform was analyzed by color Doppler to check for asymmetry indicating proximal obstruction [29].
Each ultrasonographic examination was performed by following a systematic and standardized sequence: heart, inferior vena cava, lungs, abdomen and legs veins. If the cause of hypotension was obvious at any point of the ultrasonographic evaluation, the examination was concluded. The physician in charge of the patients’ care was always aware of the ultrasound findings obtained during our first line examination and used the information for the immediate diagnostic and treatment decision making.
Retrospective clinical evaluation
The aim of retrospective clinical evaluation was to establish a final clinical diagnosis using a predefined, structured method of chart review. Three expert board-certified clinicians (FM, emergency physician; PR, cardiologist; CL, radiologist) examined all relevant clinical documentation of cases, including laboratory data, imaging procedures, consultative calls, post-mortem evaluation and other data recorded during the hospital stay. The auditors were blinded to the results of the initial ultrasonographic evaluation, and their chart review consisted of three separate steps. Initially, inclusion criteria of each single case were re-discussed. Cases where the enrollment criteria were not considered fully followed were excluded from a further clinical evaluation. Then, each auditor independently formulated a personal clinical diagnosis of the initial cause of undifferentiated hypotension by choosing from a list of eight possible diagnoses. These clinical diagnoses corresponded to the ultrasonographic categories listed in Table 2, with the exception of the distributive/hypovolemic. They represent widely accepted definitions for the diagnosis of non-traumatic hypotensive state, as published in specialty textbooks [33, 34]. Cases where the clinical documentation was considered not complete or insufficient were described as indefinite. Finally, the committee of auditors, in a plenary meeting, discussed the cases where the three independent personal diagnoses were not concordant. When the plenary discussion did not create full consensus, the contradiction was resolved by the majority. Cases without agreement of at least two of the three auditors were described as indefinite.
Statistical evaluation
Continuous data are presented as mean ± SD. The ultrasonographic diagnoses were compared with the respective final clinical diagnoses by employing the Cohen k inter-rater coefficient of agreement [35]. Values assumed by the coefficient in the different types of analyses performed are reported with the 95 % confidence intervals, the p value for the significance and the corresponding raw-agreement index. We followed the six categories of interpretation of the k coefficient values [36]. For statistical hypothesis tests, p < 0.05 was considered significant. The sample size was estimated to detect an accuracy of our protocol >90 %, requiring an enrollment of approximately 40 patients. However, the sample necessary for using the kappa method is at least 90 cases. Anticipating an approximately 10 % rate of exclusion, we planned a sample size of >100 patients.
Results
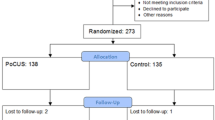
Of the 114 patients enrolled, 6 were excluded: 1 patient had a significant difference in the measured arterial pressure between the two arms, documentation of another 2 patients was considered incomplete by the review board, and for the remaining 3 patients, history records revealed they were chronically hypotensive. Thus, the study sample size was 108 patients, 66 men and 42 women, with an average age of 71.5 ± 13.5 years and a systolic blood pressure at presentation of 84 ± 11.0 mmHg. Seven patients died during hospital stay, and three of them were autopsied. The average time needed for a complete ultrasonographic evaluation was 4.9 ± 1.3 min. The final charted hospital diagnoses of the 108 cases are reported in Table 3. The final clinical diagnoses based on chart assessment by the three auditors and the ultrasonographic diagnoses obtained in the 108 patients are shown in Table 4. In the study period, there were no cases of tension pneumothorax.
Eighteen out of 67 patients with hypovolemic or distributive ultrasonographic diagnoses did not show signs of hyperkinetic LV, but showed the A pattern at lung ultrasonography. One out of the 15 cases with a cardiogenic diagnosis at ultrasonography did not show a hypokinetic LV, but showed pulmonary B pattern. Three out of eight patients with an ultrasonographic diagnosis of pulmonary embolism did not show signs of inferior vena cava congestion, but showed pulmonary A pattern. Lung ultrasonography was also decisive to finalize the diagnosis of a mixed pattern in three out of eight cases. Overall, incorporation of a lung examination in our multiorgan ultrasonographic protocol was decisive for a definite diagnosis in 24 cases (22 %).
Lung ultrasonography detected signs of pulmonary consolidation in 30 patients, in 18 cases also showing an air bronchogram. Of these, 25 had a definite diagnosis of distributive hypotension and 3 mixed, with distributive as one of the two components.
We performed three analyses: analysis 1 consisted of comparing the ultrasonographic diagnoses with the final clinical diagnoses for all 108 cases. The ultrasonographic hypovolemic/distributive pattern was considered concordant to the final clinical diagnosis when this latter was hypovolemic, distributive or mixed distributive/hypovolemic. Analysis 2 was similar to the first, but in case of a mixed clinical diagnosis with a combination of two categories, the ultrasonographic diagnosis was considered concordant when it was the same for at least one of the two. For analysis 3 we used the same criteria as for 2, but excluded cases with an indefinite final clinical diagnosis (n = 13) and indefinite ultrasonographic pattern (n = 7). There were 16 cases overall, because 4 were indefinite for both the ultrasonographic operator and the committee of auditors. Thus, analysis 3 was possible on 92 patients. Data from analysis 1, 2 and 3 are shown in Table 5.
Discussion
Goal-directed ultrasonography is an excellent diagnostic methodology to evaluate the etiology of undifferentiated hypotension at bedside. Basic focused ultrasonographic study of single organs can provide important information on functional changes. Combining single ultrasonographic analyses in a rapid multiorgan protocol improves the accuracy of the diagnostic process in case of challenging clinical situations, such as undifferentiated hypotension, sepsis and cardiac arrest. This potential was already introduced in some review articles and case series [2, 8, 9, 12, 14, 37], but the efficacy was also demonstrated by prospective studies [7, 38]. On the basis of the recommendations of the main experts on point-of-care lung ultrasound [21], we added a pulmonary evaluation to a multiorgan ultrasonographic protocol based on rapid cardiac, vein and abdominal examinations of undifferentiated hypotension in the emergency department [7].
Our protocol was effective in guiding a safe first approach to undifferentiated hypotension in the emergency department, at least in good agreement with a detailed diagnostic evaluation performed by a retrospective chart review. Ultrasonographic examination of the lung may add some crucial information in a multiorgan protocol in hypotensive states. In our study, lung examination was decisive for the definite diagnosis in 24 patients. Lung ultrasonography may indicate not only the hemodynamic effects of the condition on the pulmonary circulation, such pulmonary edema from cardiogenic shock, but also the presence of primitive pulmonary diseases causing hemodynamic instability, such as pneumonia in sepsis.
The main goal of an early diagnostic ultrasonographic study of undifferentiated hypotension cannot be the final diagnosis. Rather, point-of-care ultrasonography should be targeted at ruling out any immediate life-threatening condition and identifying the most likely cause of hemodynamic instability at that precise moment. For this reason, the committee of clinical auditors had to formulate the hypothesis on the main cause of the condition at presentation, which did not necessarily coincide with the final charted hospital diagnosis. The need to separate the initial condition from the evolution of the disease was sometimes made complicated by the acquisition of the many data of the whole clinical documentation. These difficulties may explain some of the few discrepancies found between the initial ultrasonographic hypothesis and the final clinical diagnoses.
The therapeutic interventions of undifferentiated hypotension at presentation can vary largely from the massive administration of fluids with amine support in case of hypovolemic and distributive causes, to fibrinolysis or invasive procedures in case of obstructive causes, to the pharmacological and procedural treatment of the cardiogenic cause. Not only a missing diagnosis can be highly dangerous at an early phase, as when cardiac tamponade or pneumothorax are misdiagnosed, but also an erroneous therapeutic approach can be deleterious. For instance, massive fluid administration in case of cardiogenic hypotension with impaired global function of the left ventricle may rapidly precipitate the clinical condition. The use of point-of-care ultrasonography may allow immediate classification of the clinical condition into one of the pathophysiological categories or, at least, a prompt exclusion of an immediate life-threatening condition. Further studies are needed to verify whether a multiorgan point-of-care ultrasonographic approach has a significant impact on the life expectancy of patients presenting with undifferentiated hypotension.
A limitation of our study is that we simplified our statistical analysis by arbitrarily corresponding the mixed hypotensive/distributive ultrasonographic pattern to either the hypovolemic or distributive final clinical diagnoses. We based our ultrasonographic differentiation between hypovolemic and distributive on the presence of a pulmonary consolidation with air bronchograms, which may represent a site of infection. While ultrasonographic signs of lung consolidation allowed a correct distributive diagnosis in most cases, this criterion has many limitations mainly because we may have a distributive condition without a pulmonary infection. However, this differentiation is theoretical since hypovolemic and distributive causes of undifferentiated hypotension need the same first-line therapeutic interventions to sustain the hemodynamics. Clinically, a correct differentiation of these two categories is not always possible. The progressive aging of the general population leads to an ever-increasing presence of elderly patients in our EDs. These patients represent a diagnostic challenge because very often they have multiple pathologies. Simplification of the diagnostic methodology is mandatory to meet the complexity and variability of daily practice in our crowded EDs.
Another limitation is that our protocol does not incorporate pleural effusion, although lung ultrasonography has great potential in the diagnosis of this condition. However, anechoic pleural fluid can never be assigned with certainty to a cardiogenic pattern because the transudate cannot be differentiated from the exudate using lung ultrasonography [21].
This study does not take into consideration training aspects for critical care ultrasonography. The expertise and skill of the ultrasonographic operator are crucial for the maintenance of sufficient levels of diagnostic accuracy in critical care and should always be considered in the data analysis [39].
Conclusion
This study demonstrates that point-of-care ultrasonographic diagnoses obtained in the emergency department agree with a post hoc clinical analysis of the etiology of symptomatic undifferentiated hypotension. An ultrasonographic protocol that includes lung examination may simplify the diagnostic process by reducing the viable diagnoses of hypotensive states and may allow immediate diagnosis of life-threatening conditions that can be reversed by prompt therapeutic interventions. Our data encourage the incorporation of ultrasonography into routine emergency evaluation of undifferentiated hypotension to guide early interventions. Whether or not this approach influences the outcome of hypotensive patients and associated management costs and how to incorporate point-of-care ultrasonography in the diagnostic workup remain to be elucidated by further research.
References
Moore CL, Copel JA (2011) Point-of-care ultrasonography. N Engl J Med 364:749–757
Volpicelli G (2011) Usefulness of emergency ultrasound in nontraumatic cardiac arrest. Am J Emerg Med 29:216–223
Volpicelli G (2013) Lung sonography. J Ultrasound Med 32:165–171
Lichtenstein DA (2007) Ultrasound in the management of thoracic disease. Crit Care Med 35:S250–S261
Jones AE, Aborn LS, Kline JA (2004) Severity of emergency department hypotension predicts adverse hospital outcome. Shock 22:410–414
Jones AE, Yiannibas V, Johnson C, Kline JA (2006) Emergency department hypotension predicts sudden unexpected in-hospital mortality: a prospective cohort study. Chest 130:941–946
Jones AE, Tayal VS, Sullivan DM, Kline JA (2004) Randomized, controlled trial of immediate versus delayed goal-directed ultrasound to identify the cause of nontraumatic hypotension in emergency department patients. Crit Care Med 32:1703–1708
Atkinson PR, McAuley DJ, Kendall RJ, Abeyakoon O, Reid CG, Connolly J, Lewis D (2009) Abdominal and Cardiac Evaluation with Sonography in Shock (ACES): an approach by emergency physicians for the use of ultrasound in patients with undifferentiated hypotension. Emerg Med J 26:87–91
Rose JS, Bair AE, Mandavia D, Kinser DJ (2001) The UHP ultrasound protocol: a novel ultrasound approach to the empiric evaluation of the undifferentiated hypotensive patient. Am J Emerg Med 19:299–302
Perera P, Mailhot T, Riley D, Mandavia D (2010) The RUSH exam: Rapid Ultrasound in SHock in the evaluation of the critically lll. Emerg Med Clin North Am 28:29–56
Lanctot J, Valois M, Beaulieu Y (2011) EGLS: Echo-guided life support. An algorithmic approach to undifferentiated shock. Crit Ultrasound J 3:123–129
Copetti R, Copetti P, Reissig A (2012) Clinical integrated ultrasound of the thorax including causes of shock in nontraumatic critically ill patients. A practical approach. Ultrasound Med Biol 38:349–359
Lichtenstein D, Karakitsos D (2012) Integrating lung ultrasound in the hemodynamic evaluation of acute circulatory failure (the fluid administration limited by lung sonography protocol). J Crit Care 27(533):e511–e519
Seif D, Perera P, Mailhot T, Riley D, Mandavia D (2012) Bedside ultrasound in resuscitation and the rapid ultrasound in shock protocol. Crit Care Res Pract 2012:503254
Moore CL, Rose GA, Tayal VS, Sullivan DM, Arrowood JA, Kline JA (2002) Determination of left ventricular function by emergency physician echocardiography of hypotensive patients. Acad Emerg Med 9:186–193
Randazzo MR, Snoey ER, Levitt MA, Binder K (2003) Accuracy of emergency physician assessment of left ventricular ejection fraction and central venous pressure using echocardiography. Acad Emerg Med 10:973–977
Becattini C, Agnelli G, Vedovati MC, Pruszczyk P, Casazza F, Grifoni S, Salvi A, Bianchi M, Douma R, Konstantinides S, Lankeit M, Duranti M (2011) Multidetector computed tomography for acute pulmonary embolism: diagnosis and risk stratification in a single test. Eur Heart J 32:1657–1663
Steering C (2012) Single-bolus tenecteplase plus heparin compared with heparin alone for normotensive patients with acute pulmonary embolism who have evidence of right ventricular dysfunction and myocardial injury: rationale and design of the Pulmonary Embolism Thrombolysis (PEITHO) trial. Am Heart J 163(33–38):e31
Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, Jenkins JS, Kline JA, Michaels AD, Thistlethwaite P, Vedantham S, White RJ, Zierler BK (2011) Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation 123:1788–1830
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713; (quiz 786–688)
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, Melniker L, Gargani L, Noble VE, Via G, Dean A, Tsung JW, Soldati G, Copetti R, Bouhemad B, Reissig A, Agricola E, Rouby JJ, Arbelot C, Liteplo A, Sargsyan A, Silva F, Hoppmann R, Breitkreutz R, Seibel A, Neri L, Storti E, Petrovic T, International Liaison Committee on Lung Ultrasound for International Consensus Conference on Lung Ultrasound (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38:577–591
Volpicelli G, Mussa A, Garofalo G, Cardinale L, Casoli G, Perotto F, Fava C, Frascisco M (2006) Bedside lung ultrasound in the assessment of alveolar-interstitial syndrome. Am J Emerg Med 24:689–696
Lichtenstein D, Meziere G, Seitz J (2009) The dynamic air bronchogram. A lung ultrasound sign of alveolar consolidation ruling out atelectasis. Chest 135:1421–1425
Lichtenstein DA, Lascols N, Meziere G, Gepner A (2004) Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med 30:276–281
Volpicelli G (2011) Sonographic diagnosis of pneumothorax. Intensive Care Med 37:224–232
Wallace DJ, Allison M, Stone MB (2010) Inferior vena cava percentage collapse during respiration is affected by the sampling location: an ultrasound study in healthy volunteers. Acad Emerg Med 17:96–99
Brennan JM, Blair JE, Goonewardena S, Ronan A, Shah D, Vasaiwala S, Kirkpatrick JN, Spencer KT (2007) Reappraisal of the use of inferior vena cava for estimating right atrial pressure. J Am Soc Echocardiogr 20:857–861
Kircher BJ, Himelman RB, Schiller NB (1990) Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol 66:493–496
Volpicelli G, Mussa A, Frascisco MF (2012) Sonographic diagnosis of pulmonary embolism with cardiac arrest without major dilation of the right ventricle or direct sign of lower limb venous thrombosis. J Clin Ultrasound 40:529–533
Scalea TM, Rodriguez A, Chiu WC, Brenneman FD, Fallon WF Jr, Kato K, McKenney MG, Nerlich ML, Ochsner MG, Yoshii H (1999) Focused Assessment with Sonography for Trauma (FAST): results from an international consensus conference. J Trauma 46:466–472
Hendrickson RG, Dean AJ, Costantino TG (2001) A novel use of ultrasound in pulseless electrical activity: the diagnosis of an acute abdominal aortic aneurysm rupture. J Emerg Med 21:141–144
Siragusa S, Anastasio R, Porta C, Falaschi F, Pirrelli S, Palmieri P, Gamba G, Granzow K, Malato A, Minardi V, Tatoni P, Bressan MA, Mariani G (2004) Deferment of objective assessment of deep vein thrombosis and pulmonary embolism without increased risk of thrombosis: a practical approach based on the pretest clinical model, D-dimer testing, and the use of low-molecular-weight heparins. Arch Intern Med 164:2477–2482
Loscalzo J, Harrison TR (2013) Harrison’s pulmonary and critical care medicine. McGraw-Hill Medical, New York
Tintinalli JE, Stapczynski JS (2011) Tintinalli’s emergency medicine: a comprehensive study guide. McGraw-Hill, New York
Berry CC (1992) The kappa statistic. JAMA 268:2513–2514
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37:360–363
Hernandez C, Shuler K, Hannan H, Sonyika C, Likourezos A, Marshall J (2008) C.A.U.S.E.: Cardiac arrest ultra-sound exam–a better approach to managing patients in primary non-arrhythmogenic cardiac arrest. Resuscitation 76:198–206
Haydar SA, Moore ET, Higgins GL 3rd, Irish CB, Owens WB, Strout TD (2012) Effect of bedside ultrasonography on the certainty of physician clinical decision making for septic patients in the emergency department. Ann Emerg Med 60(346–358):e344
Expert Round Table on Ultrasound in ICU (2011) International expert statement on training standards for critical care ultrasonography. Intensive Care Med 37:1077–1083
Acknowledgments
The authors thank all the staff of our emergency department who worked with enthusiasm in the study.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial registry: ClinicalTrials.gov; No.: NCT01572571; URL: http://www.clinicaltrials.gov
Rights and permissions
About this article
Cite this article
Volpicelli, G., Lamorte, A., Tullio, M. et al. Point-of-care multiorgan ultrasonography for the evaluation of undifferentiated hypotension in the emergency department. Intensive Care Med 39, 1290–1298 (2013). https://doi.org/10.1007/s00134-013-2919-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2919-7