Abstract
Purpose
To validate a novel method of ultrasound dilution (COstatus®; Transonic Systems, Ithaca, NY) for measuring cardiac output in paediatric patients after biventricular repair of congenital heart disease.
Methods
Children undergoing biventricular repair of congenital heart disease were prospectively identified. Patients with significant intracardiac shunts were excluded. Postoperative cardiac output was measured by ultrasound dilution (COud) and concurrently calculated by the Fick equation (COrms) using measured oxygen consumption by respiratory mass spectrometry.
Results
Thirty-five patients were studied generating 66 individual data sets. Subjects had a median (interquartile range) age of 147 days (11, 216), weight of 4.98 kg (3.78, 6.90) and body surface area of 0.28 m2 (0.22, 0.34). Of the patients, 66 % had peripheral arterial catheters and 34 % had femoral cannulation; peripheral arterial lines accounted for 6/8 of unsuccessful studies due to inability to generate sufficient flow. The site of the central venous cannula did not impact the feasibility of completing the study. A mean bias of 0.00 L/min [2 standard deviation (SD) ± 0.76 L/min] between COud and COrms was found with a percentage error of 97 %. When comparing cardiac index, bias increased to 0.13 L/min/m2 (2SD ± 2.16 L/min/m2).
Conclusions
Cardiac output by ultrasound dilution showed low bias with wide limits of agreement when compared to measurement derived by the Fick equation. Although measurements through central and peripheral arterial lines were completed with minimal difficulties in the majority of patients, the application of COstatus® in neonates with low body surface area may be limited.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiac output (CO) measurements in paediatrics can be an integral tool in the optimal management of critically ill children [1]. The current gold standard for such measurements consists of the use of respiratory mass spectrometry (RMS) to measure oxygen consumption (VO2), with subsequent calculation of the CO through the standard Fick equation [2]. Indicator dilution (temperature or dye) has been employed through accurate semi-automated commercially available devices [3, 4]. Nevertheless, the widespread use of these systems has been curtailed due to the requirement for a sealed airway (for RMS) or centrally invasive arterial catheters, with associated potential complications and a less than optimal risk–benefit balance.
The COstatus® device (Transonic, Systems, Ithaca, NY) uses ultrasound saline dilution to calculate CO through a modification of the Stuart–Hamilton principle. Similar to all indicator dilution techniques, the COstatus® device can measure CO in individuals with biventricular cardiac physiology in the absence of significant intracardiac shunts. However, in contrast to other systems which require pulmonary arterial or central systemic arterial cannulation for the measurement, the COstatus® device requires peripheral arterial and central venous cannulas. This minimally invasive technique has been validated in several animal and adult models [5–7]. We studied the use of this technology in paediatric patients following biventricular repair of congenital heart disease and validated it against RMS.
Methods
Patients
Following study approval by our institution’s research ethics board, consecutive patients scheduled for repair of congenital heart disease with a resultant biventricular physiology were prospectively recruited. Intraoperative transoesophageal or epicardial echocardiography was used according to routine clinical practice. Individuals with no identifiable significant residual intracardiac shunt (defined as visible tiny shunts measuring <2 mm) who, following transfer to the cardiac critical care unit, had an endotracheal tube (ETT), arterial and venous lines in situ met the criteria for study inclusion. A microcuffed ETT was requested to avoid significant leak and allow for accurate VO2 measurement. Postoperative management was not protocolized for the purpose of the study, but routinely included continuous infusion morphine for analgesia, intermittent administration of benzodiazepine (lorazepam/midazolam) for sedation, and muscle relaxation on an as-needed basis. Inotrope and vasoactive agents were used at the physician’s discretion with overall use measured by the vasopressor–inotrope score [IS = dopamine dose (mcg/kg/min) + dobutamine dose (mcg/kg/min) + 100 × epinephrine dose (mcg/kg/min) + 10 × milrinone dose (mcg/kg/min) + 10,000 × vasopressin dose (U/kg/min) + 100 × norepinephrine dose (mcg/kg/min)] [8].
COstatus®
The COstatus® system creates an extracorporeal closed arterial–venous shunt system using a routine arterial line and central venous catheter. The circuit, with a volume of approximately 5 mL, is primed with heparinized saline. When connected, a roller pump circulates blood through the system, achieving flows of 8–12 mL/min. Warmed saline (37 °C) is then injected into the venous limb with ultrasound velocity measurements of circulating blood continuously monitored through two sensor systems (Fig. 1).
The ultrasound velocity of blood is dependent primarily on the protein and ion concentrations of plasma and typically lies between 1,560 and 1,585 m/s. The determination of CO based on ultrasound velocity employs saline injection (ultrasound 1,533 m/s) for haemodilution as an indicator. CO is then calculated as the product of the volume of isotonic injection and decrease in ultrasound velocity over the integral of ultrasound velocity over time.
Measurements
After achieving steady state conditions, namely, 20 min of haemodynamic stability (stable heart rate blood pressure, no changes to inotropic–vasoactive support), we made three consecutive CO measurements per session, with the mean value (COud) calculated as an average. Individual measurements were made by manual injection of 0.5–1 mL/kg of warmed saline. Following each sample set the COstatus® loop was flushed and remained connected in-line for a maximum of 24 h. Contemporaneous COrms measurements were made with VO2 and arterial/venous blood sampling for comparison. Arterial (CaO2) and venous (CvO2) oxygen content was calculated as \( {\text{C}}_{{{\text{a}}/{\text{v}}}} {\text{O}}_{2} = \left( {1.36 \times {\text{Hemoglobin}}\;{\text{g/dL}} \times {\text{oxygen}}\;{\text{saturation}}} \right) + 0.0003\;{\text{Pa}}/{\text{vO}}_{2} \). Oxygen saturation was measured by the central laboratory by co-oximetry using a ABL800 Flex blood gas analyser (Radiometer, Brønshøj, Denmark). CO was calculated according to the Fick equation [CO = VO2/(CaO2 − CvO2)]. A maximum of three repeat COud measurements were made over a 24-h period or to study termination at time of extubation.
Respiratory mass spectrometry
An Amis 2000 quadrupole RMS (Innovision A/S, Odense, Denmark) was used to measure VO2 consistent with a previously described technique [9, 10]. In summary, with this technique, multiple gases are measured continuously, allowing for the calculation of oxygen consumption by the Argon gas dilution method.
Statistics
Descriptive statistics were generated for baseline characteristics with proportions represented as number (percentage) and continuous data as mean (standard deviation, SD) or median (interquartile range), as appropriate. A cutoff of p < 0.05 was set for statistical significance. A Bland–Altman agreement plot, demonstrating mean bias and 95 % confidence limits of agreement, was calculated for the entire population as well as for individual subpopulations based on arterial catheter type (radial vs. femoral). The CO from RMS and COstatus® were averaged, and the mean bias was calculated as the mean difference between COud and COrms across the range. Percentage error was calculated as the quotient of twice the standard deviation (2SD) of the mean difference of CO by the mean CO of the RMS.
Results
A total of 54 subjects were enrolled, of whom 19 were excluded for the following reasons: extubation in operating room prior to the study period (10 patients), RMS was not available (4 patients), severe leak around ETT invalidated RMS data (1 patient) and presence of a significant residual shunt (1 patient). Also excluded were three subjects who were connected to the COstatus® circuit but in whom flow could not be established; one of these subjects had an external jugular line, while there was no attributable difference in the other two to explain this difficulty. Since CO assessment was not possible, these individuals were excluded from analysis. In total, 35 subjects were included in the analysis.
Baseline characteristics are summarized in Table 1. Approximately one-third (34 %) of subjects had undergone an arterial switch operation for transposition of the great arteries, 20 % had undergone ventricular septal defect repair, 17 % had undergone atrioventricular septal defect (AVSD) repair, and 11 % had repair of tetralogy of Fallot (11 %). Ninety-one percent of measurements were done while the subject was on hemodynamic support, with a median vasopressor–intrope score of 6.6 [interquartile range (IQR) 6.6, 9.9]. Radial arterial catheters were used in 23 patients, and femoral arterial catheters were used in the remainder. The majority of patients (n = 30) had internal jugular cannulation, with femoral (n = 2), subclavian (n = 2) and right atrial (n = 1) venous access employed in the remainder. Repeat sampling data were acquired for 22 patients, totaling 66 data-pairs for analysis. No patient exceeded three data points. Median CO (range) was 0.62 (0.28–2.73) L/min for COrms and 0.57 (0.16–4.60) L/min for COud. When indexed for body surface area, median (range), the cardiac index (CI) for RMS and COstatus® measured at 2.38 (1.24–6.97) L/min/m2 and 2.38 (0.80–7.00) L/min/m2, respectively.
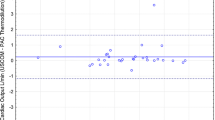
Bland–Altman analysis revealed zero bias between CO measured using RMS and that measured using the COstatus® device; the limits of agreement (LOA) were ±0.76 L/min. Two outliers were noted with a CO of >3 L/min. The first outlier excluded from the study was a 7.5-year-old undergoing primary AVSD repair (study injection of normal saline occurred at room temperature due to a malfunctioning heater); the second patient was excluded due to a large time discrepancy between the collection of arterial and venous gases and timing for COud (making temporal correlation of measurements problematic). On re-evaluation of all subjects with a mean CO of <3 L/min, a mean bias of 0.03 L/min and LOA of ±0.59 L/min were found (Fig. 2). Subjects with peripheral arterial line placement had a mean bias (±LOA) of 0.08 L/min (±0.59) compared to a mean bias of −0.03 (±0.60) with central arterial access. When the CO was indexed to body surface area (denoted as CI), the mean difference was 0.13 L/min/m2 with LOA at ±2.16 L/min/m2 (Fig. 3).
Bland–Altman plot of all individuals with a cardiac output (CO) of <3 L/min showing the comparison of CO as measured by ultrasound dilution (COud) and that measured by RMS (COrms). Bias was 0.03 L/min with limits of agreement of ±0.59 L/min. COCS CO as measured by the COstatus® device, COMS CO as measured by mass spectrometry
Bland–Altman plot showing the comparison of cardiac index (representing subjects with CO of <3.0 L/min) between COstatus® and RMS showing a bias of 0.13 L/min/m2 with limits of agreement of ±2.16 L/min/m2. CICS cardiac index as measured by CoStatus® device; CIMS cardiac index as measured by mass spectroscopy
The percentage error was calculated at 97 % for the entire data set, which decreased to 80 % using the CI data.
Discussion
Cardiac output monitoring has been mainly utilized in the management of critically ill adults for goal-directed therapy [11, 12]. Although useful, the routine measurement of CO in most intensive care units requires the insertion of pulmonary arterial or central arterial catheters. This is an invasive procedure associated with the risk of significant morbidity that has curtailed the use of such catheters in pediatrics. The clinical benefits of these catheters has also been questioned as large studies investigating the use of pulmonary artery catheters demonstrated no significant change in outcome [13]. Furthermore, the use of these measuring devices has also been implicated in increased mortality, morbidity and health expenditures [14], with documented complications including haemorrhage (e.g. haemothorax), line infection, pulmonary embolism/infarction, arrhythmias and various degrees of conduction block [13–15]. All of these factors have led to a significant decrease in the routine use of CO measurement across institutions and an increasing reliance on clinical examination for CO assessments [16]. However, both adult and pediatric studies have shown a poor correlation between a physician’s clinical determination of CO and measured results [17, 18]. This has motivated the development of accurate, minimally invasive measurement technologies which would also be safe and reliable in children.
The ultrasound velocity method allows for direct CO measurement using routine catheters that are already in place in the majority of intensive care patients. This method has been studied in several adult models, including postoperative cardiac patients, and been shown to correlate well with pulmonary arterial catheter measurements [7, 19]. A paediatric animal model has recently been validated in a general post-heart transplant paediatric population [5, 6]. All of these studies have compared the accuracy of ultrasound dilution to other dilution methods.
Our aim was to validate this technology against the CO measurement determined by the RMS/direct Fick method, which is currently the physiological gold standard in CO calculation and based on the accurate measurement of VO2 and use of the Fick equation [2]. When combined with contemporaneous arterial and central venous oxygen content from blood sampling, CO is calculated through the Fick equation. This system requires expensive specialized equipment and expert operational training, making it an impractical option for studying multiple patients in a busy critical care unit for clinical purposes [20, 21]. In our heterogenous group of infants who had undergone surgery for congenital heart disease with biventricular physiology, the CO measured by COud, on average, reflected the CO of the reference standard. However, the poor precision of the measurement by COud was noted, with the SD ranging between 0.3 and 0.38. This represents 40 % of the mean calculated CO. The SD appeared to increase at higher mean CO and CI values, reflecting poorer agreement at higher flows. Subjects with central arterial cannulation had marginally improved bias but no significant difference in agreement between COrms and COud.
Previous studies have used recommendations by Critchley and Critchley that a percentage error of ≤30 % is clinically acceptable when two CO technologies are compared [22]; this has been associated with a mean bias of as high as 0.3 L/min in certain studies. Other studies have shown a lower mean bias, but with SD of up to 0.4 L/min [3, 5]. The clinical effects of such variations cannot be discounted, in particular when dealing with smaller patients. The mean bias in our study was low at 0.03 L/min with a CO of <3 L/min; however, a wide LOA and high percentage error of 97 % brings into question the use of COud for CO measurement in this population. Improved agreement was noted with decreasing mean CO. Analysis of the subjects at the lower spectrum of CO, i.e. those with a CO of <1 L/min, revealed a mean bias of 0.05 L/min with LOA ±0.4 L/min and percentage error of 77 %. Although this seems encouraging, the degree of agreement would hazard the use of COstatus® even in smaller patients.
The agreement for CI was somewhat poorer at 0.13 L/min/m2 with LOA of 2.16 L/min/m2. Indexing CO to body surface area needs to be assessed with caution as it introduces additional opportunities for error without providing increased accuracy. Adapting the measurement to the CI also disproportionately inflates the variance in measurement as all individuals in our study were infants with a body surface areas of <1. Nevertheless, the clinical impact of the poor precision demonstrated by both the CO and CI must be considered.
Although this is not the first study to examine the validity of ultrasound dilution in children, to the best of our knowledge it is the only study to focus on infants. In a recent publication, Crittendon et al. [5] demonstrated that ultrasound dilution performed well against pulmonary artery dilution in children undergoing cardiac catheterization. In their study population comprising children older than 1 year with a minimum weight of approximately 10 kg and central arterial catheterization, a SD of ±0.4 L/min was noted for a range of CO between 1 and 6 L/min. Our results complement their work well in investigating the use of ultrasound dilution in infants, a population not previously studied. In our study, the absolute CO ranged between 0.2 and 2.2 L/min but generally fell below the range studied above. The absolute variance in the mean difference in CO is consistent with that reported from human pediatric and adult studies and animal models with a SD in the range of 0.2–0.5 L/min. However, the same variance at a lower CO represents a higher percentage error, leading to a higher potential clinical impact. The weaker measurement performance in our study may reflect a limitation of COud in smaller individuals or an inherent variance to this technology that does not tighten at lower CO. Potentially this may be overcome with modification to the measurement algorithm when this patient group is being studied.
Infants following cardiopulmonary bypass surgery, with a systemic inflammatory response and inotropic requirement, may also have a unique physiology that contributes to weaker measurement performance that would not have manifested in the relatively healthy subject population used in previous pediatric models [5, 6]. The majority of studied infants were on inotropic support, mainly milrinone, which may have affected measurements. However, a high agreement was noted in COud measurements in corresponding adult patients following cardiac surgery [7]. Lastly, our trial is unique in comparing two completely distinct CO measurement techniques, as all previous studies compared the transpulmonary dilution technique used in COud to other dilution CO measurements. As such, the tighter agreement in previous studies may reflect biases consistent across dilution CO measurements that are not seen in the RMS/direct Fick method. The CO calculation using the Fick equation and measured VO2 value has been generally accepted as the physiological gold standard. Nevertheless, several potential sources of error have been associated with its use in intensive care patients. The accuracy of continuous VO2 measurements in intensive care patients has been questioned particularly in association with increased pulmonary consumption in the presence of lung pathology [23]. Poor agreement between Fick and CO measured by thermodilution, another reference standard, has been identified in numerous intensive care studies [24–26]. Another potential source of systematic error is the use of central venous saturation (CvO2), in contrast to the optimal mixed venous saturation (MvO2) in the Fick calculation. Although a tight correlation is usually observed between the two measurements, CvO2 has been shown to reflect MvO2 poorly in the setting of severe heart failure or shock [27]. It is unclear how large a role this played in this validation study.
To examine the feasibility of COstatus® utilization within the routine care of pediatric postoperative patients, we did not modify or standardize postoperative operative care or catheter selection. The study group represented the wide variation of repairs and case complexity seen in biventricular repairs of congenital heart disease. As mentioned, in only three of the 54 children recruited for study was the COstatus® measurement not completed due to the inability to achieve adequate flows through the circuit; of these individuals, one patient had an external jugular line providing high downstream pressure, and two had decreased arterial flow through 22-gauge radial arterial catheters. Five other study patients had at least one episode during which sufficient flow was not generated through the circuit; four of these patients had a radial arterial line. The inability to generate adequate flows was attributed to elevated circuit resistance, potentially due to mild distal catheter obstruction.
The most important benefit offered by this technology is the ability to run CO measurements with peripheral arterial catheters that are the standard of care in many institutions. Although 75 % of patients who did not achieve adequate flows had radial arterial lines, this represented fewer than 15 % of all patients with arterial lines. Two patients were even successfully studied with a 24-gauge radial arterial line. All patients with difficulty achieving adequate arterial flows had a body surface area of <0.25 m2. The site of the arterial cannula position had very little effect on the performance of the COstatus® measurement. When used with central arterial cannulas, COud tended to overestimate the CO by a mean of 30 mL/min/m2; in comparison, the CO was marginally underestimated by 80 mL/min/m2 by COud when peripheral arterial lines were used. These differences are not clinically significant.
This study has certain inherent limitations. Recruitment was predominantly limited to younger and smaller patients by virtue of their ongoing postoperative ventilatory requirement. Additional investigation is required to validate COStatus® technology for larger children who are do not fall below the previously validated adult size [7, 28]. Secondly, this study was limited to individuals with biventricular physiology without significant shunts. CO monitoring in children with a single ventricle is still limited to calculated values based on the Fick equation and VO2 measurement. Further studies investigating the role of this technology in the wider setting of congenital heart disease surgery are warranted.
Conclusion
Based on our results, we conclude that the ultrasound dilution measurement of CO using the COstatus® device in infants shows a poor agreement with CO determined by measured oxygen consumption and the Fick equation. This wide range in agreement level, which persisted even when data were transformed from CO to CI, may reflect a limitation of this transpulmonary dilution technique in individuals with low body surface area and may restrict its applicability in neonates following bypass surgery. Technically, the COud measurements were completed with little difficulty in patients with central arterial lines. Difficulty in achieving adequate flows was noted in a minority of subjects with peripheral arterial lines. There were no patient-related complications during the trial.
References
Wernovsky G, Wypij D, Jonas RA, Mayer JE Jr, Hanley FL, Hickey PR, Walsh AZ, Chang AC, Castaneda AR, Newburger JW et al (1995) Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants. A comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 92:2226–2235
Boyd AD, Tremblay RE, Spencer FC, Bahnson HT (1959) Estimation of cardiac output soon after intracardiac surgery with cardiopulmonary bypass. Ann Surg 150:613–626
Linton RA, Jonas MM, Tibby SM, Murdoch IA, O’Brien TK, Linton NW, Band DM (2000) Cardiac output measured by lithium dilution and transpulmonary thermodilution in patients in a paediatric intensive care unit. Intensive Care Med 26:1507–1511
Fakler U, Pauli C, Balling G, Lorenz HP, Eicken A, Hennig M, Hess J (2007) Cardiac index monitoring by pulse contour analysis and thermodilution after pediatric cardiac surgery. J Thorac Cardiovasc Surg 133:224–228
Crittendon I 3rd, Dreyer WJ, Decker JA, Kim JJ (2012) Ultrasound dilution: an accurate means of determining cardiac output in children*. Pediatr Crit Care Med 13:42–46
Darling E, Thuramalla N, Searles B (2011) Validation of cardiac output measurement by ultrasound dilution technique with pulmonary artery thermodilution in a pediatric animal model. Pediatr Cardiol 32:585–589
Eremenko AA, Safarov PN (2010) Flow-regulated extracorporeal arteriovenous tubing loop for cardiac output measurements by ultrasound velocity dilution: validation in post-cardiac surgery intensive care unit patients. ASAIO J 56:522–526
Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG, Charpie JR, Hirsch JC (2010) Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 11:234–238
Shekerdemian LS, Shore DF, Lincoln C, Bush A, Redington AN (1996) Negative-pressure ventilation improves cardiac output after right heart surgery. Circulation 94:II49–II55
Davies NJ, Denison DM (1979) The measurement of metabolic gas exchange and minute volume by mass spectrometry alone. Respir Physiol 36:261–267
Richard C, Warszawski J, Anguel N, Deye N, Combes A, Barnoud D, Boulain T, Lefort Y, Fartoukh M, Baud F, Boyer A, Brochard L, Teboul JL (2003) Early use of the pulmonary artery catheter and outcomes in patients with shock and acute respiratory distress syndrome: a randomized controlled trial. JAMA 290:2713–2720
Harvey S, Harrison DA, Singer M, Ashcroft J, Jones CM, Elbourne D, Brampton W, Williams D, Young D, Rowan K (2005) Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): a randomised controlled trial. Lancet 366:472–477
Shah MR, Hasselblad V, Stevenson LW, Binanay C, O’Connor CM, Sopko G, Califf RM (2005) Impact of the pulmonary artery catheter in critically ill patients: meta-analysis of randomized clinical trials. JAMA 294:1664–1670
Connors AF Jr, Speroff T, Dawson NV, Thomas C, Harrell FE Jr, Wagner D, Desbiens N, Goldman L, Wu AW, Califf RM, Fulkerson WJ Jr, Vidaillet H, Broste S, Bellamy P, Lynn J, Knaus WA (1996) The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT Investigators. JAMA 276:889–897
Sandham JD, Hull RD, Brant RF, Knox L, Pineo GF, Doig CJ, Laporta DP, Viner S, Passerini L, Devitt H, Kirby A, Jacka M (2003) A randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients. N Engl J Med 348:5–14
Wiener RS, Welch HG (2007) Trends in the use of the pulmonary artery catheter in the United States, 1993–2004. JAMA 298:423–429
Tibby SM, Hatherill M, Marsh MJ, Murdoch IA (1997) Clinicians’ abilities to estimate cardiac index in ventilated children and infants. Arch Dis Child 77:516–518
Eisenberg PR, Jaffe AS, Schuster DP (1984) Clinical evaluation compared to pulmonary artery catheterization in the hemodynamic assessment of critically ill patients. Crit Care Med 12:549–553
Galstyan G, Bychinin M, Alexanyan M, Gorodetsky V (2010) Comparison of cardiac output and blood volumes in intrathoracic compartments measured by ultrasound dilution and transpulmonary thermodilution methods. Intensive Care Med 36:2140–2144
Li J, Bush A, Schulze-Neick I, Penny DJ, Redington AN, Shekerdemian LS (2003) Measured versus estimated oxygen consumption in ventilated patients with congenital heart disease: the validity of predictive equations. Crit Care Med 31:1235–1240
Li J, Zhang G, Holtby HM, McCrindle BW, Cai S, Humpl T, Caldarone CA, Williams WG, Redington AN, Van Arsdell GS (2006) Inclusion of oxygen consumption improves the accuracy of arterial and venous oxygen saturation interpretation after the Norwood procedure. J Thorac Cardiovasc Surg 131:1099–1107
Critchley LA, Critchley JA (1999) A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 15:85–91
Light RB (1988) Intrapulmonary oxygen consumption in experimental pneumococcal pneumonia. J Appl Physiol 64:2490–2495
Axler O, Tousignant C, Thompson CR, Dall’ava-Santucci J, Phang PT, Russell JA, Walley KR (1996) Comparison of transesophageal echocardiographic, Fick, and thermodilution cardiac output in critically ill patients. J Crit Care 11:109–116
Sherman MS, Kosinski R, Paz HL, Campbell D (1997) Measuring cardiac output in critically Ill patients: disagreement between thermodilution-, calculated-, expired gas-, and oxygen consumption-based methods. Cardiology 88:19–25
Gonzalez J, Delafosse C, Fartoukh M, Capderou A, Straus C, Zelter M, Derenne JP, Similowski T (2003) Comparison of bedside measurement of cardiac output with the thermodilution method and the Fick method in mechanically ventilated patients. Crit Care 7:171–178
Scheinman MM, Brown MA, Rapaport E (1969) Critical assessment of use of central venous oxygen saturation as a mirror of mixed venous oxygen in severely ill cardiac patients. Circulation 40:165–172
Tsutsui M, Matsuoka N, Ikeda T, Sanjo Y, Kazama T (2009) Comparison of a new cardiac output ultrasound dilution method with thermodilution technique in adult patients under general anesthesia. J Cardiothorac Vasc Anesth 23:835–840
Acknowledgements
We would like to acknowledge Transonic Systems (Ithaca, NY) supplying the COstatus® equipment and study disposables.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Floh, A.A., La Rotta, G., Wermelt, J.Z. et al. Validation of a new method based on ultrasound velocity dilution to measure cardiac output in paediatric patients. Intensive Care Med 39, 926–933 (2013). https://doi.org/10.1007/s00134-013-2848-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2848-5