Abstract
The aim of our study was to determine the validity of cardiac output (CO) measurements taken with the ultrasonic cardiac output monitor (USCOM) by comparing to CO measured by pulmonary arterial catheter (PAC) thermodilution during cardiac catheterization. We enrolled thirty-one children (<18 years) undergoing cardiac catheterization in this double-blinded, prospective, observational study. The median CO measured by USCOM was 4.37 L/min (IQR 3.73, 5.60 L/min) compared to 4.28 L/min (IQR 3.52, 5.26 L/min) by PAC thermodilution. The bias (mean difference) between the two methods was 0.2 L/min, and the 95 % limits of agreement were −1.2 to 1.6 L/min. The mean percentage error of CO between USCOM and PAC thermodilution was 11 %. When excluding a sole outlier, the bias between the two measures decreased to 0.1 L/min (95 % limits of agreement −0.6 to 0.9 L/min), and the percentage error was reduced to 8 %. The median SVRI measured by USCOM was 22.0 Wood Units (IQR 17.0, 26.8 Wood Units) compared to 22.1 Wood Units (IQR 17.6, 27.4 Wood Units) by PAC thermodilution. Bias (mean difference) between the two methods was −0.6 Wood Units, and the 95 % limits of agreement were −8.2 to 6.9 Wood Units. We found that the estimation of CO and by extension SVRI with USCOM is reliable against pulmonary artery catheter thermodilution in children with normal cardiac anatomy. Given the noninvasive nature of USCOM, speed of measurement, and relative ease of use, it may be useful as a bedside tool for pediatric patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiac output (CO) measurement is a cornerstone of advanced hemodynamic monitoring and provides invaluable information for the circulatory management of critically ill patients. Invasive measurement of CO at the bedside with a pulmonary artery catheter (PAC) [14] is feasible and often used for intensive monitoring of larger patients, but PACs are less applicable for children and unsuitable for neonates. During the last decade, noninvasive technologies have become available for the measurement of CO and additional hemodynamic variables. However, most are validated only in adults, and conclusions regarding adult hemodynamic monitoring cannot be extrapolated to pediatric patients [6, 9, 21, 24, 26]. Moreover, clinical estimation of CO, although still frequently practiced, poorly correlates with the true value of CO [13, 27].
The ultrasonic cardiac output monitor (USCOM Pty Ltd, Coffs Harbour, NSW, Australia) was introduced for clinical use in 2001, providing a rapid and noninvasive measure of cardiac function. USCOM uses Doppler ultrasound to measure the velocity of blood flow through the aortic or pulmonary valve. USCOM has been validated in a canine model [8] and in adult patients comparing it to CO PAC thermodilution technique [3, 5, 16, 25]. USCOM has been used clinically in a variety of settings [17, 18, 23]. USCOM has been approved by the FDA for use in children with evidence of good inter-rater reliability and ease of use [11]. In children, there are only two prior studies comparing CO by USCOM to two-dimensional echocardiography [22, 28] and only one comparing USCOM to PAC thermodilution [15]. In these studies, USCOM did not perform well enough to be considered an alternative method to measure CO. This was contrary to our clinical experience, and in turn, we sought to investigate the accuracy of the USCOM in children. The primary objective of this study was to determine the concordance of CO measurement by the USCOM compared to the gold standard PAC thermodilution, in children undergoing cardiac catheterization.
Materials and Methods
The CHLA IRB (CCI #12-00218) approved this study, and written parental consent was obtained for all patients. Pediatric patients undergoing diagnostic cardiac catheterization for the evaluation of cardiac function were prospectively enrolled. Patients with intracardiac or extracardiac shunt, aortic valve disease, or age older than 21 years were excluded. Premedication and induction of anesthesia depended upon the patient’s medical condition and the interventional cardiologist’s preferences.
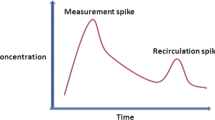
For the catheterization procedure, venous access was obtained, and oxygen saturation and pressure measurements were recorded from the superior vena cava and branch pulmonary artery. A size-appropriate thermodilution catheter was inserted via the right atrium into the right or left pulmonary artery. Thermodilution catheter computation constants were used per the catheter’s recommendations (Arrow Medical Products, Research Triangle Park, NC), and cardiac output was measured using catheterization laboratory software (XPer, Philips Medical Systems, Amsterdam, the Netherlands). CO measurements were obtained by injecting room-temperature sterile saline (10 mL for 6Fr catheters, 5 mL for 5Fr catheters, 3 mL for 4Fr catheters) in triplicate within the space of 5 min. Cardiac output was calculated to precision of 0.01 L/min. All CO PAC thermodilution measurements were taken by one investigator (JDM). After the PAC thermodilution measurements, pulmonary arterial wedge pressure, branch PA pressure, right ventricular pressure, and right atrial pressure were measured before the catheter was removed.
After hemodynamics measurements were taken, coronary angiography and/or endomyocardial biopsy were performed in patients requiring those tests. The vascular access sheaths were then removed, and USCOM measurements were obtained. Anesthesia or analgesia/sedation was maintained until the USCOM measurements were completed.
The CO measurements by USCOM were taken by one experienced physician (FB) blinded to invasive results. Prior to initiating the study, the USCOM operator was trained by an experienced company representative and took numerous USCOM measurements. A minimum of three CO measurements by USCOM were obtained within a period of 5 min. Patient data, including height, weight, and gender, were entered into the USCOM device as well as blood pressure measurements during the procedure. To measure CO by USCOM, Doppler flow curves are obtained using a 3.3-MHz transducer placed in the suprasternal notch to obtain an optimal flow signal at the aortic valve. The Doppler curve is displayed by the device, and the operator adjusts the angle of insonation to return the best Doppler curve. The goals of adjustment were to obtain a flow profile that is well defined at the base, peak, and starting and stopping blood flow [10]. The Doppler curve should be free from interference from the subject talking, and the scale is adjusted as appropriate. Doppler curves are stored for later review, and individual heart beats can be removed for incompleteness or interference. This Doppler curve is measured as the velocity time integral (VTI). As the VTI is a two-dimensional representation of CO, there is no means to confirm the angle of insonation or to measure valve diameter. Typically, the highest, fullest, most complete, and well-defined Doppler curves would indicate the best alignment with the aortic valve, and these are chosen by the operator.
Hemodynamic Calculations
The CO values from both PAC thermodilution and USCOM were divided by body surface area of the patient to produce cardiac index (CI) values. CI values were used in the calculation of systemic vascular resistance index (SVRI). Because not all patients underwent left heart catheterization, noninvasive blood pressure measurements were used for all patients in estimation of SVRI. SVRI (Woods Units) = (Mean Arterial Pressure − Mean right atrial pressure)/Cardiac Index.
The USCOM software uses an algorithm based on the patient’s height to determine the area of the aortic valve providing outflow tract diameter (OTD). The USCOM software calculates stroke volume (SV) from the VTI and OTD and then calculates cardiac output as SV × Heart rate. After the procedure, values of CO were divided by the body surface area to produce CI. SVRI was calculated by the USCOM machine after inputting the mean arterial pressure and mean right atrial pressure obtained during catheterization.
Statistics
Sample size for the study was determined a priori using the Bland formula for repeatability with the assumptions of three measurements per subject and a within-subject standard deviation of 10 %. The minimal sample size required to estimate the width of the 95 % confidence interval within 10 % was 20 individuals. Accepting the potential for a higher within-subject standard deviation, the target enrollment was set at 30.
Mean values of the repeated measurements for both methods were calculated per patient and used for further statistics. Mean standard deviation for all of the triplicate measurements was calculated for both PAC thermodilution and USCOM to identify variation within the measurements. Bland–Altman analysis [1] was performed to compare the mean CO values obtained by USCOM and PAC thermodilution, reporting bias and limits of agreement. Agreement between the measurement values was also assessed with Pearson’s correlation. Outlier analysis was also performed.
To compensate for the relationship between the magnitude of CO measurements and the size of the error, percentage error was calculated, as suggested by Critchley and Critchley [7]. This is especially important for pediatric patients, who have lower absolute CO values compared with adults [7]. The percentage error can be calculated by taking the percentage of the limits of agreement in relation to the mean CO measurement value of the reference technique. The percentage error can be used as a cutoff value for accepting a new technique. A mean percentage error not exceeding 30 % was the target to indicate clinically useful reliability of the USCOM [7].
Results
Thirty-one patients scheduled to undergo cardiac catheterization were approached for consent, and all agreed to participate. Complete data were available on all subjects except SVR measurements obtained from cardiac catheterization for one patient. The patient displayed airway obstruction during the procedure, preventing reliable measurements of central venous pressure. Patient demographics are listed in Table 1. The median age was 12 years, with two children under the age of 2 years.
Twenty-seven patients received procedural sedation with intravenous midazolam and fentanyl. Seven of these patients also received ketamine. Four patients received general anesthesia. At the discretion of the anesthesiologist, two patients received propofol, and two patients received sevoflurane. In the entire cohort, only two patients were endotracheally intubated for the procedure. There did not appear to be any systematic bias with regard to which patients received general anesthesia.
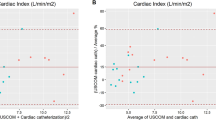
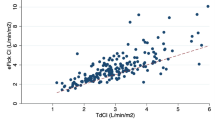
Mean CO measured by PAC thermodilution ranged from 0.81 to 6.85 L/min, median 4.28 L/min (1, 3 IQR 3.52, 5.26 L/min), and mean CO values measured by USCOM ranged from 1 to 7.38 L/min, median 4.37 L/min (1, 3 IQR 3.73, 5.60 L/min). Bias (mean difference) between the two methods was 0.2 L/min, and the 95 % limits of agreement were −1.2 to 1.6 L/min (Fig. 1). Pearson’s correlation between the two techniques had an r = 0.87 (Fig. 2). The mean percentage error of CO between techniques was 11 %. For the three PAC thermodilution injections per patient, there was an average standard deviation (SD) of 0.14 L/min. For the three USCOM measures per patient, there was an average SD of 0.24 L/min. Median SVRI by PAC thermodilution was 22.1 Woods Units (1, 3 IQR 17.6, 27.4) and 22.0 Woods Units (1, 3 IQR 17.0, 26.8) by USCOM. Bias (mean difference) between the two methods was −0.6 Wood Units, and the 95 % limits of agreement were −8.2 to 7.6 Wood Units (Fig. 3). Pearson’s correlation between the two techniques for SVRI had an r = 0.87 (Fig. 4). The mean percentage error of SVRI between techniques was 11 %.
Bland–Altman plot of systemic vascular resistance indexed (SVRI) measured by USCOM as compared to PAC thermodilution. This figure demonstrates the bias between the methods (mean, solid line) and 95 % limits of agreement (dotted lines). All paired values are included in the analysis including one outlier
There was one outlier noted during the USCOM measurements. For this individual patient, the mean CO by PAC thermodilution was 3.81 L/min as compared to 7.38 L/min by USCOM. We feel the significant discordance was secondary to very poor windows and loss of her sedated and comfortable state during that measurement. This patient was studied again at a different occasion, and the mean CO by PAC thermodilution was 4.37 L/min as compared to 5 L/min by USCOM, with a percentage error of 12 %. Excluding this measurement from CO analysis resulted in a mean bias of 0.1 L/min between USCOM and PAC thermodilution with 95 % limits of agreement −0.6 to 0.9 L/min. The Pearson’s correlation increased to r = 0.96, and the mean percentage error decreased to 8 %. Excluding this measurement from SVRI analysis resulted in a mean bias of −0.3 Wood Units with 95 % limits of agreement −7.2 to 6.6 Wood Units. The Pearson’s correlation increased to r = 0.89, and the mean percentage error decreased to 10 %.
Discussion
Our study validates the accuracy of cardiac output measurements obtained by USCOM as compared to PAC thermodilution in children with normal cardiac anatomy. Measurements of CO with USCOM reliably represent CO obtained via pulmonary artery catheter thermodilution with a mean percentage error of 11 %. It can also give a reliable estimate of SVRI if blood pressure is included, with a mean percentage error of 11 %.
Our study should be reviewed in the context of those that did not find similar results. Studies by Nguyen et al. [22] and Wongsirimetheekul et al. [28] compared CO measured by USCOM to that measured by two-dimensional echocardiography (2D Echo). Again, CO = SV × HR and SV = Outflow tract diameter (OTD) × Velocity Time Integral (VTI). In both of these studies, there was no significant difference in the OTD supplied by the nomogram from the USCOM device as compared to the OTD measured by 2D Echo. The VTI measured by USCOM was significantly greater than that measured by 2D Echo, accounting for the difference in CO measurement. Many, including these authors, have noted that USCOM uses continuous wave Doppler measurements for VTI, whereas 2D Echo uses pulse wave Doppler. USCOM and continuous wave Doppler will identify and measure the highest VTI along the entire path of the measurement. In the case of pulse wave Doppler, the cursor is set to measure the velocity obtained at the aortic valve annulus. In our view, the greatest flaw with these studies was the lack of a gold standard for measuring cardiac output.
With reference to the gold standard of PAC thermodilution, our findings are also counter to those of Knirsch et al. [15] who compared CO measured by USCOM to PAC thermodilution. However, their study population included only patients with congenital heart disease undergoing interventional catheterization. As the authors pointed out “The fact that our study included no patients with normal cardiac anatomy included may be considered as a limitation of this study.” In particular, 15 of their 24 patients were undergoing cardiac catheterization for closure of either an atrial septal defect or ventricular septal defect, though they reportedly took CO measurements after the intervention has been completed. For our study, we chose patients with structurally normal hearts specifically to avoid the issue of intracardiac shunting or the alterations in physiology which might occur immediately after interventional procedures.
Our results do support a number of other studies that show positive benefits for the use of USCOM. USCOM has been shown to have good intra- and inter-observer reliability in children [12] and in neonates [20]. The USCOM device has shown acceptable agreement for CO with 3D transthoracic echo in pregnant women [19]. It can produce good-quality CO tracings in a pediatric urgent care setting [29]. Further, normal ranges for cardiovascular parameters in nonsedated children have been produced [2], and the CO measurements were well tolerated [4] with no greater discomfort than noninvasive blood pressure measurement. Aside from the small number of our patients who had a significantly depressed cardiac output, our results for CO fall within the range reported by Cattermole et al. [2].
It is again worth mentioning that the USCOM uses continuous wave Doppler, the signal of which can be contaminated by turbulence/acceleration within abnormal valves or arteries, as in particular is the case with patients with pulmonary artery stenosis, pulmonary valve stenosis, or coarctation of the aorta as were studied by Knirsch et al. [15]. There is no definitive way to determine what the proper angle of insonation is when obtaining measurements with USCOM. In normal anatomy, one can rely on the aortic valve and ascending aorta to generally contain the fastest blood flow, and therefore, USCOM interrogation along the typical trajectory and optimized for the strongest signal generally yields an aortic valve tracing.
Clinical estimation of CO, although still frequently practiced, correlates poorly with the true value of CO [13, 27]. It is possible that more accurate assessment of CO with this simple and noninvasive technique may improve patient care and help gauge response to therapies. The USCOM may play a role in further clinical investigations, as it is easy to apply, noninvasive, and based on our findings, accurate in pediatric patients with structurally normal hearts.
There are several limitations to our study. Most of the eligible patients were receiving routine post-cardiac transplant catheterizations. For this reason, we had only a few patients with very low or high cardiac output. Greater experience will be needed before we know this device’s applicability to the physiologic stresses present in children in the intensive care unit. Also, we were not able to make simultaneous assessments of CO by PAC thermodilution and USCOM due to issues of sterility during the procedure, patient safety, and blinding of the investigators. Although we attempted to keep patients at steady state, it is possible that anesthetic conditions could have changed in the interval between the two measurements, thus changing cardiac output. We attempted to keep the time interval as brief as possible and to limit stimulation of the patients.
The USCOM has its own limitations. USCOM uses continuous wave Doppler without 2D Echo to guide placement of the beam, VTIs may be larger than measured in other circumstances. During measurements, the aortic root is explored, and a number of signals from other vessels are identified. The dominant signal is from the aortic valve. However, it is possible to insonate the wrong vessel or the wrong region because of lack of experience. Thus, a learning curve is anticipated with the USCOM. Because USCOM calculates cardiac output by using one Doppler flow profile and the inter-peak distance, irregularity of heart rate will result in beat-to-beat variation in cardiac output estimates.
Despite these limitations, to our knowledge this is the first study in children with structurally normal hearts validating CO and by extension SVRI measurements by USCOM against PAC thermodilution. USCOM is a reliable tool to assess hemodynamic status in pediatric patients with no intracardiac shunts. The learning curve for skill acquisition is very short. Further studies are needed to validate its usefulness in neonates, patients with congenital heart defects, and in pediatric patients with both high and low cardiac outputs as in shock states.
References
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Cattermole GN, Leung PY, Mak PS, Chan SS, Graham CA, Rainer TH (2010) The normal ranges of cardiovascular parameters in children measured using the Ultrasonic Cardiac Output Monitor. Crit Care Med 38(9):1875–1881
Chan JS, Segara D, Nair P (2006) Measurement of cardiac output with a non-invasive continuous wave Doppler device versus the pulmonary artery catheter: a comparative study. Crit Care Resusc 8(4):309–314
Chan S, Cattermole GN, Leung M, Ho G, Graham C, Rainer T (2013) Children’s discomfort during noninvasive cardiac output monitoring by suprasternal ultrasonographic transducer [online]. Hong Kong J Emerg Med 20(1):3–8
Chand R, Mehta Y, Trehan N (2006) Cardiac output estimation with a new Doppler device after off-pump coronary artery bypass surgery. J Cardiothorac Vasc Anesth 20(3):315–319
Chaney JC, Derdak S (2002) Minimally invasive hemodynamic monitoring for the intensivist: current and emerging technology. Crit Care Med 30(10):2338–2345
Critchley LA, Critchley JA (1999) A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 15(2):85–91
Critchley LA, Peng ZY, Fok BS, Lee A, Phillips RA (2005) Testing the reliability of a new ultrasonic cardiac output monitor, the USCOM, by using aortic flowprobes in anesthetized dogs. Anesth Analg 100(3):748–753
de Waal EE, Wappler F, Buhre WF (2009) Cardiac output monitoring. Curr Opin Anaesthesiol 22(1):71–77
Dey I, Sprivulis P (2005) Emergency physicians can reliably assess emergency department patient cardiac output using the USCOM continuous wave Doppler cardiac output monitor. Emerg Med Australas 17(3):193–199
Dhanani S, Barrowman NJ, Ward RE, Murto KT (2011) Intra- and inter-observer reliability using a noninvasive ultrasound cardiac output monitor in healthy anesthetized children. Paediatr Anaesth 21(8):858–864
Dhanani S, Barrowman NJ, Ward RE, Murto KT (2011) Intra- and inter-observer reliability using a noninvasive ultrasound cardiac output monitor in healthy anesthetized children. Paediatr Anaesth 21(8):858–864
Egan JR, Festa M, Cole AD, Nunn GR, Gillis J, Winlaw DS (2005) Clinical assessment of cardiac performance in infants and children following cardiac surgery. Intensive Care Med 31(4):568–573
Ganz W, Donoso R, Marcus HS, Forrester JS, Swan HJ (1971) A new technique for measurement of cardiac output by thermodilution in man. Am J Cardiol 27(4):392–396
Knirsch W, Kretschmar O, Tomaske M, Stutz K, Nagdyman N, Balmer C, Schmitz A, Bettex D, Berger F, Bauersfeld U, Weiss M (2008) Cardiac output measurement in children: comparison of the ultrasound cardiac output monitor with thermodilution cardiac output measurement. Intensive Care Med 34(6):1060–1064
Knobloch K, Lichtenberg A, Winterhalter M, Rossner D, Pichlmaier M, Phillips R (2005) Non-invasive cardiac output determination by two-dimensional independent Doppler during and after cardiac surgery. Ann Thorac Surg 80(4):1479–1483
Knobloch K, Hubrich V, Rohmann P, Lupkemann M, Gerich T, Krettek C, Phillips R (2006) Feasibility of preclinical cardiac output and systemic vascular resistance in HEMS in thoracic pain—the ultrasonic cardiac output monitor. Air Med J 25(6):270–275
Knobloch K, Hoeltke V, Jakob E, Vogt PM, Phillips R (2008) Non-invasive ultrasonic cardiac output monitoring in exercise testing. Int J Cardiol 126(3):445–447
McNamara H, Barclay P, Sharma V (2014) Accuracy and precision of the ultrasound cardiac output monitor (USCOM 1A) in pregnancy: comparison with three-dimensional transthoracic echocardiography. Br J Anaesth 113(4):669–676
Meyer S, Todd D, Shadboldt B (2009) Assessment of portable continuous wave Doppler ultrasound (ultrasonic cardiac output monitor) for cardiac output measurements in neonates. J Paediatr Child Health 45(7–8):464–468
Morgan P, Al-Subaie N, Rhodes A (2008) Minimally invasive cardiac output monitoring. Curr Opin Crit Care 14(3):322–326
Nguyen HB, Banta DP, Stewart G, Kim T, Bansal R, Anholm J, Wittlake WA, Corbett SW (2010) Cardiac index measurements by transcutaneous Doppler ultrasound and transthoracic echocardiography in adult and pediatric emergency patients. J Clin Monit Comput 24(3):237–247
Siu CW, Tse HF, Lee K, Chan HW, Chen WH, Yung C, Lee S, Lau CP (2007) Cardiac resynchronization therapy optimization by ultrasonic cardiac output monitoring (USCOM) device. Pacing Clin Electrophysiol 30(1):50–55
Skowno JJ, Broadhead M (2008) Cardiac output measurement in pediatric anesthesia. Paediatr Anaesth 18(11):1019–1028
Tan HL, Pinder M, Parsons R, Roberts B, van Heerden PV (2005) Clinical evaluation of USCOM ultrasonic cardiac output monitor in cardiac surgical patients in intensive care unit. Br J Anaesth 94(3):287–291
Tibby SM, Murdoch IA (2003) Monitoring cardiac function in intensive care. Arch Dis Child 88(1):46–52
Tibby SM, Hatherill M, Marsh MJ, Murdoch IA (1997) Clinicians’ abilities to estimate cardiac index in ventilated children and infants. Arch Dis Child 77(6):516–518
Wongsirimetheekul T, Khositseth A, Lertbunrian R (2014) Non-invasive cardiac output assessment in critically ill paediatric patients. Acta Cardiol 69(2):167–173
Zorko DJ, Choong K, Gilleland J, Agar B, Baker S, Brennan C, Pullenayegum E (2013) Urgent ultrasound guided hemodynamic assessments by a pediatric medical emergency team: a pilot study. PLoS ONE 8(6):e66951
Acknowledgments
USCOM Limited provided the USCOM-1A device used in the study but had no role in the study design, analysis, or review of the manuscript. No financial support was used for this study. The investigators independently conducted the research study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Beltramo, F., Menteer, J., Razavi, A. et al. Validation of an Ultrasound Cardiac Output Monitor as a Bedside Tool for Pediatric Patients. Pediatr Cardiol 37, 177–183 (2016). https://doi.org/10.1007/s00246-015-1261-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1261-y