Abstract
Purpose
In critically ill adults, a reduction in the extravascular lung water index (EVLWi) decreases time on mechanical ventilation and improves survival. The purpose of this study is to assess the prognostic value of EVLWi in critically ill children with acute respiratory failure and investigate its relationships with PaO2, PaO2/FiO2 ratio, A-aDO2, oxygenation index (OI), mean airway pressure, cardiac index, pulmonary permeability, and percent fluid overload.
Methods
Twenty-seven children admitted to PICU with acute respiratory failure received volumetric hemodynamic and blood gas monitoring following initial stabilization and every 4 h thereafter, until discharge from PICU or death. All patients are grouped in two categories: nonsurvivors and survivors.
Results
Children with a fatal outcome had higher values of EVLWi on admission to PICU, as well as higher A-aDO2 and OI, and lower PaO2 and PaO2/FIO2 ratio. After 24 h EVLWi decreased significantly only in survivors. As a survival indicator, EVLWi has good sensitivity and good specificity. Changes in EVLWi, OI, and mean airway pressure had a time-dependent influence on survival that proved significant according to the Cox test. Survivors spent fewer hours on mechanical ventilation. We detected a correlation of EVLWi with percent fluid overload and pulmonary permeability.
Conclusions
Like OI and mean airway pressure, EVLWi on admission to PICU is predictive of survival and of time needed on mechanical ventilation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Extravascular lung water index (EVLWi) reflects the amount of fluid in the interstitium and in the alveolar space; a value greater than 12 ml/kg indicates a clinical picture of pulmonary edema [1]. The accepted normal volume of EVLWi is <10 ml/kg [2, 3]. In critically ill children, EVLWi can increase as the result of both changes in pulmonary permeability and generalized fluid and electrolyte imbalance [4].
In adults increased EVLWi is accompanied by reduced survival [5–7]. There is evidence that restriction of fluid intake and maintenance of adequate urine output can improve pulmonary function and shorten the time on mechanical ventilation, with reduction of PICU time. However, no effect was shown on mortality at 60 days [8]. According to other authors [9], a negative fluid balance at day 4 of acute lung injury is indeed associated with significantly lower mortality.
Consequently every effort is made to prevent pulmonary edema by bringing EVLWi back to normal [10, 11]. Pulmonary edema is commonly monitored with chest X-rays and in terms of pulmonary artery occlusion pressure via a pulmonary artery catheter (PAC). Both methods have proved unreliable in the detection of pulmonary edema [12, 13]. In particular modulating therapy based on artery occlusion pressures assessed with PAC has proved inadequate to improve survival or organ function [14]. EVLWi can be directly assessed using thermo-dye dilution [5, 6], but it is a cumbersome technique to use routinely.
At present, routine single indicator EVLWi calculation can be done more easily with the thermodilution method. EVLWi measurements thus obtained are comparable with the thermo-dye dilution technique and with the gravimetric method, the latter being considered the gold standard for EVLWi assessment [15].The thermodilution method for hemodynamic monitoring is particularly appealing for use in pediatrics, as it avoids pulmonary artery catheterization, which carries a significant risk [16]. It must be said that thermodilution also has its drawbacks. Because the thermistor is in the femoral artery, the volume of the aorta adds up to the one of the cardiac chambers, and global end diastolic volume (GEDV) may be overestimated [17]. Mechanical ventilation can affect GEDV, although only when high positive end expiratory pressure exceeds 15 cm of H2O [18].
Thermodilution can also measure GEDV (used as preload index), stroke volume, systemic vascular resistances (SVR), and pulmonary permeability, opening new diagnostic and therapeutic perspectives [1, 19, 20]. Michard [21] has recently reported in adults that measurement of EVLWi helps to quantify pulmonary edema and hence to guide therapy. In adults, Phillips and colleagues [22] consider EVLWi a valid prognostic indicator of acute respiratory distress syndrome associated with sepsis.
Reliable prognostic indicators are important in the management of critically ill children requiring mechanical ventilation. Various indexes of oxygen exchange are used to guide mechanical ventilatory support [23] and are used also as prognostic indicators, although their reliability is not universally accepted [24]. At present there are no studies on EVLWi as prognostic indicator in pediatrics.
The aim of this pilot study on a relatively small pediatric cohort is to explore correlations between EVLWi and prognosis in children on mechanical ventilation for non-cardiac acute respiratory failure. To this end, we have compared EVLWi with the prognostic indexes presently used in pediatrics. Based on the hypothesis that EVLWi correlates with pulmonary permeability, fluid overload, and cardiac index, if a correlation can be demonstrated, a further achievement might be the clarification of which of the factors is more relevant in causing pulmonary edema in critically ill children with acute respiratory failure.
Methods
Twenty-seven children in acute respiratory failure [25] were enrolled in the study over 24 months. Informed consent was obtained from both parents of each child. The protocol conforms to the guidelines of the Declaration of Helsinki and was approved by the ethical committee of the involved institution [26]. Children with congenital heart diseases or intracardiac shunts, and children with an abnormal coagulation profile contraindicating femoral catheterization were excluded.
Pediatric risk of mortality (PRISM) score [27] was assessed for each child on admission to PICU. Monitoring of volumetric and ventilatory parameters and indexes of oxygen exchange were started as soon as the children were stabilized and mechanical ventilatory support started (see the electronic supplementary material). Regular measurements were performed every 4 h, and additional readings were obtained whenever hemodynamics appeared to worsen. Each volumetric measurement is expressed as the mean value of three consecutive readings. The monitoring ended when the child was weaned from the ventilator or died.
Hemodynamic volumetric monitoring (see the electronic supplementary material) was done with a commercially available device (PiCCO®; Pulsion Medical System, Munich, Germany) [22]. Measurements included cardiac output (CO, l/min) [28], GEDV (ml) [29, 30], EVLW (ml) [1], pulmonary blood volume (PBV, ml) [11], pulmonary permeability as EVLW/PBV ratio [1], and systemic vascular resistance (SVR, dyn s cm−5). All parameters were indexed for body surface area (BSA) (CI = CO/BSA, GEDVi = GEDV/BSA, PBVi = PBV/BSA, SVRi = SVR/BSA) or body weight (EVLWi = EVLW/body weight). Indexes of oxygen exchange include partial pressure of oxygen (PaO2), PaO2/FiO2 ratio (P/F ratio), alveolar arterial oxygen gradient (A-aDO2), and oxygenation index (OI) [30, 31] (see the electronic supplementary material). Patients were grouped as nonsurvivors and survivors to assess the relationship of survival with EVLWi, pediatric PRISMA score, MAP, and indexes of oxygen exchange and to evaluate intra- and intergroup variations. For each patient we also calculated the percent fluid overload (FO%) using the formula: %FA = (total fluid intake − total fluid output) [l]/body weight [kg] × 100.
According to Oland et al. [32], body weights were derived from the clinic charts or obtained from relatives. We entered the lowest weight registered during the month prior to admission. We studied the correlation of EVLWi with FO%, EVLWi/PBVi ratio, and CI.
Data analysis
For statistical analysis we relied on JUMP® 8.0.1 program for Mac by SAS Institute. For all variables the approximation to normal of the distribution of the population was tested by Kolmogorov-Smirnov one-sample test, and statistics for kurtosis and symmetry were assessed. As results were asymmetrically distributed, nonparametric tests were used. Data are expressed as mean ± standard deviation.
We used the Kruskal-Wallis nonparametric one-way analysis of variance to examine the changes in EVLWi in both groups on admission, at 24 and 36 h, and at the end of observation. The null hypothesis was that the groups of the study all came from the same distribution. When the Kruskal-Wallis test was significant, we used the Wilcoxon test to compare the intragroup differences at the four observation times and the Mann-Whitney U test for intergroup variation.
In both survivors and nonsurvivors, to evaluate the variation of the other parameters, we used the Wilcoxon test to estimate the intragroup variation (i.e., admission vs. end of the observation), and the Mann-Whitney U test for intergroup differences (i.e., nonsurvivors vs. survivors). A power test was run to rule out type II error. Variations of parameters from beginning to end of observation were calculated using the formula ∆p = (pex−pen)−100/pen. Sensitivity and specificity for survival were determined by the receiver operating characteristic curve (ROC curve). The time-dependent effect on survival of the explanatory variables was examined with Cox’s proportional hazard method. Existing correlations between parameters considered in the study were tested with Pearson’s r.
Results
Twenty-seven children (15 males and 12 females) with a median age of 72 months (range 6–144 months) admitted to PICU and mechanically ventilated for acute respiratory failure [25] were enrolled in the study over 24 months. Age, sex, survival, diagnosis, time on mechanical ventilation, sets of measurements, and PRISM score for each patient are reported in Table 1.
Six (22%) of the 27 children in the study died in the PICU (nonsurvivors); 21 (78%) survived and could be extubated (survivors). Of the six deceased, only one had EVLWi = 10 ml/kg; five out of six had EVLWi >10 ml/kg.
On admission to PICU
PRISM score was significantly higher in nonsurvivors than survivors: 31.17 ± 10.85 vs. 12.38 ± 6.68, p < 0.0011, power 0.99.
In the intergroup comparison, EVLWi, A-aDO2, OI, and MAP were found to be significantly higher in nonsurvivors; PaO2 and PaO2/FiO2 ratio were significantly reduced. Pulmonary permeability (EVLWi/PBVi), GEDVVi, SVi, and SVRi were not different (Tables 2, 3).
As shown in Tables 2 and 3, the intergroup observation showed that in nonsurvivors, we found significantly higher levels of EVLWi, A-aDO2, OI, and MAP, and significantly reduced values of PaO2 and PaO2/FiO2 ratio. Pulmonary permeability (EVLWi/PBVi), GEDVi, SVi, and SVRi were not different.
The receiver operating characteristic curve test (ROC test) identifies good sensitivity and specificity for all parameters with an area under the curve (AUC) that was always significant: PRISM score AUC = 0.94, OI AUC = 0.92, MAP AUC = 0.92, PaO2/FiO2 ratio AUC = 0.85, EVLWi AUC = 0.81, A-aDO2 AUC = 0.80, PaO2 AUC = 0.79, and EVLWi/PBVi ratio AUC = 0.78 (see Figs. E1 and E2 in the electronic supplementary material).
At end of observation
At the end of the study the intergroup observation showed significantly elevated A-aDO2, OI, EVLWi, MAP, and EVLWi/PBVi in nonsurvivors and reduced PaO2 and PaO2/FiO2 ratio (Tables 2, 3).
During stay in PICU
Nonsurvivors were mechanically ventilated for a greater number of hours (nonsurvivors vs. survivors: 9,467 ± 4,327 vs. 6,247 ± 4,397 h, p < 0.0408, power = 0.60). Between entry and exit from the study (Tables 2, 3), in nonsurvivors there was a significant increase in OI and MAP, while in survivors we observed a significant reduction in OI and EVLWi. All other parameters were unchanged or their changes did not attain statistical significance (Table 2). In survivors, EVLWi was already reduced significantly at 24 h, and the levels remained stable throughout the stay in PICU (Table 2). In contrast, in nonsurvivors EVLWi remained constantly elevated (Table 2). Moreover in survivors, EVLWi was lower at 24 and 36 h when compared with the nonsurvivors (Table 2). With Cox’s proportional hazard method we were able to prove a significant time-dependent influence on survival only for changes (∆) in OI, EVLWi, and MAP (∆OI: χ2 = 6.87, prob > χ2 0.0088, p < 0.0077; ∆EVLWi: χ2 = 5.02, prob > χ2 0.0251, p < 0.0079; ∆MAP: χ2 = 13.11, prob > χ2 0.0003, p < 0.00091). No significant changes in CI could be observed either intra- or intergroup (Table 3). Percent fluid overload was significantly higher in nonsurvivors than in survivors (4.59 ± 2.12 vs. 1.06 ± 0.64, p < 0.0003, power test = 1.0).
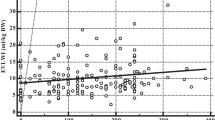
Finally the correlation between EVLWi and FO% attained statistical significance (EVLWi = 5.09 + 4.86 × FO%; r 2 = 0.63, p < 0.0001) as did that between EVLWi and EVLWi/PBVi (EVLWi = 0.88 + 9.69 × EVLWi/PBVi; r 2 = 0.53, p < 0.0001). In contrast, correlation between EVLWi and CI was not statistically significant.
Discussion
Mortality of the pediatric patients in our study was 9% (1 patient) among those with an EVLWi ≤10 ml/kg (11 patients) at admission to PICU and 31% (five patients) among those with EVLWi >10 ml/kg (16 patients). The incidence of mortality is consistent with that reported by other authors in critically ill children with acute respiratory failure and is lower than the average mortality for the same condition in adults [31, 33, 34]. Martin et al. [2], Sakka et al. [7], and Berkowitz et al. [35] report that in adult patients mortality increases with increasing volumes of EVLW. In particular Martin and colleagues [2] report better survival (100 vs. 36%) at 28 days in patients with severe sepsis and ARDS, when EVLWi could be maintained <10 ml/kg. In 373 critically ill patients, Sakka and colleagues [7] found that the mortality rate was approximately 65% in patients with EVLWi >15 ml/kg, whereas it was approximately 33% in patients with EVLWi <10 ml/kg. Berkowitz et al. [35] report that mortality exceeds 60% when EVLWi is >10 ml/kg. In our study, similar to the findings reported in adult populations, the children who did not survive their acute respiratory failure had had EVLWi volumes significantly elevated throughout the entire PICU stay (Table 2).
The concept that a positive fluid balance is partly responsible for a bad prognosis in the presence of pulmonary edema has been validated by Mitchell et al. [6]. These authors support a strategy based on a negative fluid balance as tolerated by the patient in terms of hemodynamics. Another recent study reports that a cumulative negative fluid balance on day 4 was associated independently with a lower hospital mortality and more ventilator- and ICU-free days [9]. Also in children with acute renal failure and hemodynamic instability, fluid overload has been shown to favor mortality [36]. In critically ill children, reduction of fluid overload with continuous venovenous hemofiltration (CVVH) improves survival [37], fluid balance, and caloric intake and allows for a parallel reduction in the use of diuretics. In our study, percent fluid overload was higher in nonsurvivors than in survivors, confirming these observations. Presently, however, it is difficult to define the pathophysiologic mechanisms linking pulmonary damage and hyperhydration [38].
In our study EVLWi had decreased significantly in survivors already at 24 h and remained constant thereafter until discharge (Table 2). With the Cox test we could also prove that time-related changes (∆) in EVLWi, MAP, and OI significantly influenced survival. This is consistent with Kuzkov and colleagues’ study [30] showing that changes in EVLWi at day 3 are predictors of outcome. The significance of EVLWi for the outcome of adult critical patients has been addressed in a number of studies. Matthay et al. [39] and Ware et al. [40] stress that reabsorption of pulmonary edema, the latter defined as fluid accumulation in the pulmonary extravascular space, can be impaired in acute lung injury and ARDS. Kuzkov et al. [30] report that pulmonary permeability and EVLWi increase significantly in septic patients with acute lung injury who do not survive.
The assumption that increased EVLWi can result at least in part from more severe damage to the pulmonary parenchyma is also supported by our findings. In nonsurvivors, we found lower levels of PaO2/FiO2 ratio, and higher levels of OI and pulmonary permeability both at entry and exit from the study (Table 3). The intragroup analysis showed only a significant reduction in the levels of OI in the survivors and a significant increase in the nonsurvivors, but no significant changes in PaO2/FiO2 ratio and pulmonary permeability between the two groups (Table 3). Further support is offered by the significant correlation that we observed between elevation of EVLWi and increased FO% and pulmonary permeability, resulting in more time on mechanical ventilation and higher mortality rate as already reported by others in adult patients [5–7]. According to our findings, the correlation between EVLWi and patient outcome is significant. However, the underlying pathophysiology remains undetermined. As recently reported also by other authors, it is not clear if the increase in extravascular fluid in the lungs is strictly dependent on excess amounts of extravascular fluids, is the consequence of increased lung permeability, or both [10, 38]. Therefore, EVLWi qualifies as a reliable prognostic index, but its usefulness as a guide to proper fluid therapy can only be speculative. At present, optimization of EVLWi with an appropriate therapy is an extremely difficult task. On the one hand excessive administration of fluids can increase pulmonary edema and mortality [41], on the other hand, excessive fluid restriction can cause hypovolemia and reduction of preload and peripheral organ perfusion [42]. As suggested by Foland et al., hemofiltration applied earlier and more decisively might improve volume parameters.
The number of observations in our study is relatively small, so that the study itself should be considered a pilot one. However, the analysis of the data collected on critically ill children admitted to PICU with acute respiratory failure points to a good concordance of EVLWi with all indexes of oxygen exchange. Also sensitivity and specificity appear to be good. In conclusion, eventual confirmation of our findings, obtained from a much wider multicenter study, might suggest routine assessment of EVLWi with the thermodilution method as a reliable prognostic index in critically ill children with acute respiratory failure. Speculations on the potential role of EVLWi assessment in guiding an appropriate fluid replacement therapy should be withheld until the pathophysiological mechanisms of pulmonary edema are better understood.
References
Monnet X, Anguel N, Osman D, Hamzaoui O, Richard C, Teboul JL (2007) Assessing pulmonary permeability by transpulmonary thermodilution allows differentiation of hydrostatic pulmonary edema from ALI/ARDS. Intensive Care Med 33:1125–1132
Martin GS, Eaton S, Mealer M, Moss M (2005) Extravascular lung water in patients with severe sepsis: a prospective cohort study. Crit Care 9:R74–R82
Groenneveld AB, Verheij J (2006) Extravascular lung water to blood volume ratios as measures of permeability in sepsis-induced ALI/ARDS. Intensive Care Med 32:1315–1321
Sibbald WJ, Short AK, Warshawski FJ, Cunningham DG, Cheung H (1985) Thermal dye measurements of extravascular lung water in critically ill patients: intravascular Starling forces and extravascular lung water in the adult respiratory distress syndrome. Chest 87:585–592
Eisenberg PR, Hansbrough JR, Anderson D, Schuster DP (1987) A prospective study of lung water measurements during patient management in an intensive care unit. Am Rev Respir Dis 136:662–668
Mitchell JP, Schuller D, Calandrino FS, Schuster DP (1992) Improved outcome based on fluid management in critically ill patients requiring pulmonary artery catheterization. Am Rev Respir Dis 145:990–998
Sakka SG, Klein M, Reinhart K, Meier-Hellmann A (2002) Prognostic value of extravascular lung water in critically ill patients. Chest 122:2080–2086
The National Heart, Lung and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trial Network (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Rosenberg AL, Dechert RE, Park PK, Bartlett RH, NHI NHLBI ARDS Network (2009) Association of cumulative fluid balance on outcome in acute lung injury: a retrospective review of the ARDSnet Tidal Volume Study cohort. J Intensive Care Med 24:35–46
Rivers EP (2006) Fluid management strategies in acute lung injury—liberal, conservative, or both? N Engl J Med 354:2598–2600
Sakka SG, Rühl CC, Pfeiffer UJ, Beale R, McLuckie A, Reinhart K, Meier-Hellmann A (2000) Assessment of cardiac preload and extravascular lung water by single transpulmonary thermodilution. Intensive Care Med 26:180–187
Halperin BD, Feeley TW, Mihm FG, Chiles C, Guthaner DF, Blank NE (1985) Evaluation of the portable chest roentgenogram for quantitating extravascular lung water in critically ill adults. Chest 88:649–652
Takayama Y, Iwasaka T, Sugiura T, Sumimoto T, Takeuchi M, Tsuji H, Takashima H, Taniguchi H, Inada M (1991) Increased extravascular lung water in patients with low pulmonary artery occlusion pressure after acute myocardial infarction. Crit Care Med 19:21–25
Robin ED (1985) The cult of Swan-Ganz catheter: overuse and abuse of pulmonary flow catheter. Ann Intern Med 103:445–449
Katzenelson R, Perel A, Berkenstadt H, Preisman S, Kogan S, Sternik L, Segal E (2004) Accuracy of transpulmonary thermodilution versus gravimetric measurement of extravascular lung water. Crit Care Med 32:1550–1554
Pauli C, Falker U, Genz T, Hennig M, Lorenz HP, Hess J (2002) Cardiac output determination in children: equivalence of the transpulmonary thermodilution method to the direct Fick principle. Intensive Care Med 28:947–952
Brivet FG, Jacobs F, Colin P (2004) Calculated global end-diastolic volume does not correspond to the largest heart blood volume: a bias for cardiac function index? Inensive Care Med 30:2133–2134
Kubitz JC, Annecke T, Kemming GI, Forkl S, Kronas N, Goetz AE, Reuter DA (2006) The influence of positive end-expiratory pressure on stroke volume variation and central blood volume during open and closed chest conditions. Eur J Cardiothorac Surg 30:90–95
Fernandez-Mondejar E, Guerrero-Lopez F, Colmenero M (2007) How important is the measurement of extravascular lung water? Curr Opin Crit Care 13:79–83
Cecchetti C, Lubrano R, Cristaldi S, Stoppa F, Barbieri MA, Elli M, Masciangelo R, Perrotta D, Travasso E, Raggi C, Marano M, Pirozzi N (2008) Relationship between global end-diastolic volume and cardiac output in critically ill infants and children. Crit Care Med 36:928–932
Michard F (2007) Bedside assessment of extravascular lung water by dilution methods: temptations and pitfalls. Crit Care Med 35:1186–1192
Phillips CR, Chesnutt MS, Smith SM (2008) Extravascular lung water in sepsis-associated acute respiratory distress syndrome: indexing with predicted body weight improves correlation with severity of illness and survival. Crit Care Med 36:69–73
El-Khatib MF, Jamaleggine GW (2004) A new oxygenation index for reflecting intrapulmonary shunting in patients undergoing open-heart surgery. Chest 125:592–596
Rodriguez Martinez CE, Guzman MC, Castillo JM, Sossa MP, Ojeda P (2006) Evaluation of clinical criteria for the acute respiratory distress syndrome in pediatric patients. Pediatr Crit Care Med 7:335–339
Ralston M, Hazinski MF, Zaritsky AL, Schexnayder SM, Kleiman ME (2006) PALS provider manual. American Heart Association, Dallas
World Medical Association (2000) Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 284:3043–3045
Pollak MM, Ruttiman UE, Geston PR (1998) Pediatric risk of mortality (PRISM) score. Crit Care Med 16:1110–1116
Francis DB, Hu KC (1977) An algorithm for the automated determination of cardiac output by the Stewart-Hamilton method. IEEE Trans Biomed Eng 24:482–484
Meier P, Zierler KL (1954) On the theory of the indicator-dilution method for measurement of blood flow and volume. J Appl Physiol 6:731–734
Kuzkov VV, Kirov MY, Sovershaev MA, Kuklin VN, Suburov EV, Waerhaug K, Bjertnaes LJ (2006) Extravascular lung water determined with single transpulmonary thermodilution correlates with the severity of sepsis-induced acute lung injury. Crit Care Med 34:1647–1653
Trachsel D, McCrindle BW, Nakagawa S, Bohn D (2005) Oxygenation index predicts outcome in children with acute hypoxemic respiratory failure. Am J Respir Crit Care Med 172:206–211
Foland JA, Fortenberry JD, Warshaw BL, Pettignano R, Merritt RK, Heard ML, Rogers K, Reid C, Tanner AJ, Easley KA (2004) Fluid overload before continuous hemofiltration and survival in critically ill children: a retrospective analysis. Crit Care Med 32:1771–1776
Kneyber MC, Brouwers GA, Caris JA, Chedamni S, Plötz FB (2008) Acute respiratory distress syndrome: is it under recognized in the pediatric intensive care unit? Intensive Care Med 34:751–754
Dahlem P, van Aalderen WM, Hamaker ME, Dijkgraaf MG, Bos AP (2003) Incidence and short-term outcome of acute lung injury in mechanically ventilated children. Eur Respir J 22:980–985
Berkowitz DM, Pajman AD, Eaton S, Moss M, Martin GS (2008) Acute characterization of extravascular lung water in acute respiratory distress syndrome. Crit Care Med 36:1803–1809
Sutherland SM, Zappitelli M, Alexander SR, Chua AN, Brophy PD, Bunchman TE, Hackbarth R, Somers MJ, Baum M, Symons JM, Flores FX, Benfield M, Askenazi D, Chand D, Fortenberry JD, Mahan JD, McBryde K, Blowey D, Goldstein SL (2010) Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kid Dis 55:316–325
Hoover NG, Heard M, Reid C, Wagoner S, Rogers K, Foland J, Paden ML, Fortenberry JD (2008) Enhanced fluid management with continuous venovenous hemofiltration in pediatric respiratory failure patients receiving extracorporeal membrane oxygenation support. Intensive Care Med 34:2241–2247
Groeneveld ABJ, Polderman KH (2005) Acute lung injury, overhydration or both? Critical Care 9:136–137
Matthay MA, Robriquet L, Fang X (2005) Alveolar epithelium. Role in lung fluid balance and acute lung injury. Proc Am Thorac Soc 2:206–213
Ware LB, Matthay MA (2001) Alveolar fluid clearance is impaired in the majority of patients with acute lung injury and the acute respiratory distress syndrome. Am J Respir Crit Care Med 163:1376–1383
Goldstein SL, Somers MJ, Baum MA, Symons JM, Brophy PD, Blowey D, Bunchman TE, Baker C, Mottes T, McAfee N, Barnett J, Morrison G, Rogers K, Fortenberry JD (2005) Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int 67:653–658
Metha RI, Pascual MT, Soroko S, Chertow GM (2002) Diuretics mortality and nonrecovery of renal function in acute renal failure. JAMA 288:2547–2553
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lubrano, R., Cecchetti, C., Elli, M. et al. Prognostic value of extravascular lung water index in critically ill children with acute respiratory failure. Intensive Care Med 37, 124–131 (2011). https://doi.org/10.1007/s00134-010-2047-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-2047-6