Abstract
Purpose
Although chemotherapy and transplantation improve outcome of patients with hematological malignancy, complications of these therapies are responsible for a 20–50% mortality rate that increases when respiratory symptoms evolve into acute lung injury (ALI). The aim of this study is to determine the effectiveness of early continuous positive airway pressure (CPAP) delivered in the ward to prevent occurrence of ALI requiring intensive care unit (ICU) admission for mechanical ventilation.
Methods
Patients with hematological malignancy presenting in the hematological ward with early changes in respiratory variables were randomized to receive oxygen (N = 20) or oxygen plus CPAP (N = 20). Primary outcome variables were need of mechanical ventilation requiring ICU admission, and intubation rate among those patients who required ICU admission.
Results
At randomization, arterial-to-inspiratory O2 ratio in control and CPAP group was 282 ± 41 and 256 ± 52, respectively. Patients who received CPAP had less need of ICU admission for mechanical ventilation (4 versus 16 patients; P = 0.0002). CPAP reduced the relative risk for developing need of ventilatory support to 0.25 (95% confidence interval: 0.10–0.62). Among patients admitted to ICU, intubation rate was lower in the CPAP than in the control group (2 versus 14 patients; P = 0.0001). CPAP reduced the relative risk for intubation to 0.46 (95% confidence interval: 0.27–0.78).
Conclusions
This study suggests that early use of CPAP on the hematological ward in patients with early changes in respiratory variables prevents evolution to acute lung injury requiring mechanical ventilation and ICU admission.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Improved chemotherapeutic agents and transplantation have dramatically improved the outcome of patients with hematological malignancies. Unfortunately, these therapies are associated with complications that are largely responsible for a mortality rate that ranges between 20% and 50% [1]. This rate increases when respiratory symptoms evolve into acute lung injury (ALI) requiring mechanical ventilation and admission to ICU [2, 3].
Although there are early changes in respiratory variables that precede the development of acute lung injury [4], interventions on non-ICU wards are usually limited to administration of supplemental oxygen [5]. One ventilatory approach, which can be used in the non-ICU setting, is continuous positive airway pressure (CPAP). Recent studies have demonstrated the efficacy of CPAP in preventing [6–8] and treating [9] acute hypoxemic respiratory failure without need for tracheal intubation. The key finding of some of these studies is the need to apply CPAP very early in the disease process for optimal efficacy [10].
The present study was designed to examine the hypothesis that application of CPAP in patients with hematological malignancy who exhibit early changes in respiratory variables would prevent evolution of early signs of respiratory impairment to acute lung injury requiring mechanical ventilation and ICU admission.
Methods
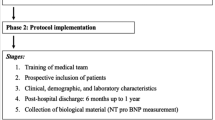
The institutional review board approved the protocol, and written informed consent was obtained from all patients. Patients were recruited from October 2005 to November 2007 (two hematological units of the S. Giovanni Battista-Molinette Hospital).
Patients with hematological malignancy and chemotherapy/bone marrow transplantation induced white cell count <1,000 cells/mm3 and showing for more than 48 h (1) radiological evidence of bilateral pulmonary infiltrates, (2) pulse oxygen saturation (SaO2) <90% while breathing room air, and (3) respiratory rate >25 breaths/min were randomized to control [oxygen through Venturi mask at inspiratory fraction of O2 (FiO2) of 0.5] or CPAP (FiO2 0.5 plus CPAP 10 cmH2O).
We excluded patients who had a diagnosis of pneumonia, infection, and/or sepsis [11]. Evidence of infection was excluded using institutional standard diagnostic workup for suspected infection [pulmonary computed tomography (CT) scan, laboratory tests, blood cultures, and bronchoalveolar lavage]. These were therefore performed in all patients, and data were prospectively collected. Other exclusion criteria were: lack of consent; age <18 or >80 years old; New York Heart Association functional class II–IV, valvular heart disease, history of dilated cardiomyopathy, cardiogenic pulmonary edema, implanted cardiac pacemaker, unstable angina, myocardial infarction, or cardiac surgery within the previous 3 months; systolic arterial pressure <90 mmHg after optimal fluid therapy; history of chronic obstructive pulmonary disease (COPD) or asthma; body mass index >40 kg/m2; presence of facial, neck, or chest wall abnormalities; arterial pH <7.30 with arterial carbon dioxide tension >50 mmHg; diagnosis of sleep or neuromuscular disorders, claustrophobia; Glasgow Coma Scale <12; presence of graft-versus-host disease; life expectancy <12 months.
All patients in the hospital with hematological malignancy were followed daily for inclusion and exclusion criteria by staff of the hematological wards. Once a patient met entry criteria and informed consent was signed, the patient was randomized via a dedicated website using a computer-generated randomization schedule and the protocol team (senior resident in anesthesia and experienced ICU nurse) was notified. Enrolled patients were continuously monitored with electrocardiogram trace, noninvasive blood pressure, arterial oxygen saturation, and respiratory rate. The protocol team checked included patients at least twice a day and was available around the clock. Senior critical care medical support was available around the clock at the request of the protocol or hematological ward teams. The number of calls and number of therapeutic orders (fluid and catecholamine administration, and device adjustments) and monitoring orders (request for arterial blood gases, chest X-ray, and continuous monitoring of SaO2) were recorded.
After randomization, control or CPAP was applied for 4-day periods consisting of at least 12 consecutive hours per day. At the end of each period, patients underwent a 6-h screening test during which they breathed through a Venturi mask with FiO2 0.3 [8]. If one or more of the following criteria was fulfilled, patients were returned to the assigned treatment for another 4-day period: radiological evidence of pulmonary infiltrates, SaO2 <95%, respiratory rate >25 breaths/min. The treatment protocol was discontinued when the patient met all the following criteria: clear chest X-ray, SaO2 ≥95%, respiratory rate ≤25 breaths/min. CPAP was generated using a flow generator with adjustable FiO2 with a spring-loaded expiratory pressure valve (Whisperflow, Caradyne, Ireland) and applied using a transparent latex-free polyvinylchloride helmet (CaStar, Starmed, Italy) [8].
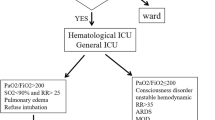
Primary outcomes were evolution of early signs of respiratory impairment to acute lung injury estimated as need of mechanical ventilation requiring ICU admission and, among patients admitted to ICU, number of patients who required endotracheal intubation for invasive ventilation [12–14]. Since the study was not blinded, we attempted to minimize potential biases by: first, having the decision for ICU admission for mechanical ventilation (noninvasive or invasive) based on: SaO2 ≤80% with FiO2 0.5; arterial pH <7.30 with PaCO2 >50 mmHg; or use of accessory muscle or occurrence of paradoxical abdominal or thoracic movements, or initiated on other clinical grounds by a senior hematologist and a senior critical care physician, neither of whom were study investigators. Second, intubation was performed when patients had one of the following: (1) PaO2/FiO2 ≤85;(2) hemodynamic instability defined as systolic blood pressure <70 mmHg or need for inotropic drugs to maintain systolic blood pressure >85 mmHg for 2 h or more, or electrocardiographic evidence of ischemia or significant ventricular arrhythmias; (3) need for sedation for major agitation; (4) metabolic acidosis with pH ≤7.20 (5) Glasgow Coma Scale <9; (6) development of copious tracheal secretions; (7) increase in PaCO2 accompanied by pH ≤7.30; (8) cardiac arrest [8].
Secondary outcome variables were: number of ICU-free days during the 28 days immediately after ICU entry, number of hospital-free days during the 6 months after randomization, and hospital mortality. Incidence of pneumonia and sepsis [11] was assessed post hoc after randomization in the two groups of patients.
Using retrospective review of medical charts and data from a previous study [15] we estimated that 50% of the control subjects would require ICU admission for mechanical ventilation. We hypothesized that use of CPAP would reduce this to 10% based on a previous study in which there was a 90% decrease in intubation rate in postoperative patients treated with CPAP [8]. Using these assumptions, as well as a 5% risk of type I error and 80% power, we estimated that we would require 40 patients.
All analyses were conducted on an intention-to-treat basis. Values are reported as mean and standard deviation, or median and interquartile range, as appropriate. Continuous variables were compared using unpaired t-test or Wilcoxon rank-sum test, as appropriate. Categorical variables were compared using Fisher’s exact test or chi-square test, when appropriate. The Kaplan–Meier curve was compared by log-rank and Wilcoxon tests. Statistical analysis was performed by using SAS 8.2 software (SAS Institute, Cary, NC). Statistical significance was taken as P < 0.05; all reported P values are two-sided.
Results
Of the 522 patients with hematological malignancy and white cell count <1,000 cells/mm3, 69 patients met criteria for early alteration of respiratory function (13%) and 40 underwent randomization. The remaining 29 patients were not randomized because of: lack of consent (N = 8); history of dilated cardiomyopathy (N = 2); history of chronic obstructive pulmonary disease (N = 3); diagnosis of pneumonia (N = 5), infection (N = 1) or sepsis (N = 3); life expectancy <12 months (N = 7) (Fig. 1). Among the patients not randomized, 14 were admitted to the ICU for noninvasive ventilation.
Baseline characteristics were similar in both groups (Table 1). PaO2/FiO2 ratio at randomization in control and CPAP was 282 ± 41 and 256 ± 52, respectively. White cell count <1,000 cells/mm3 started 10 ± 5 and 11 ± 5 days before enrollment in control and CPAP, respectively. Recovery occurred 8 ± 4 and 8 ± 6 days after study enrollment in control and CPAP, respectively. After randomization, application of O2 or of O2 plus CPAP increased PaO2/FiO2 ratio to 392 ± 15 and 441 ± 10, respectively (P < 0.01). Attending hematologists referred initial respiratory symptoms as associated with chest CT scan showing (1) predominant alveolar infiltrates (ten patients in control and nine patients in CPAP), (2) alveolar and interstitial infiltrates (eight patients in control and ten patients in CPAP), (3) interstitial infiltrates compatible with idiopathic interstitial pneumonia (two patients in control and one in CPAP) [16, 17].
The number of calls to and the number of interventions delivered by the protocol team did not differ between control and CPAP. Orders to adjust fluid administration and the respiratory device were significantly more frequent in CPAP than control (Table 2). Time of treatment was 10.8 ± 6.9 days (16.3 ± 3.8 h per day) in CPAP and 11.4 ± 4.6 days (16.5 ± 2.6 h per day) in control. No patients developed intolerance to the devices.
Figure 2 shows Kaplan–Meier curves of development of acute lung injury requiring ventilatory management and ICU admission: 16 patients in control and 4 patients (20%) in CPAP required ICU admission for ventilatory management (P = 0.0002). CPAP reduced the relative risk for developing acute lung injury requiring ICU admission for ventilatory support to 0.25 (95% confidence interval: 0.10–0.62); the number needed to treat for benefit was 1.7. ICU admission occurred 10 ± 4 days after randomization in the control group and 10 ± 2 after randomization in the CPAP group.
Numbers of patients treated with invasive and noninvasive ventilation at ICU entry and numbers of patients who failed noninvasive ventilation and required intubation are presented in Table 3. Reasons for ICU admission and initiation of mechanical ventilation and for failure of noninvasive ventilation are listed in Table 4. CPAP reduced the relative risk for intubation to 0.14 (95% confidence interval: 0.03–0.54); the number needed to treat for benefit was 1.7.
Figure 3 shows Kaplan–Meier curves of hospital mortality: 5 patients in control and 17 patients in CPAP left the hospital alive (P = 0.0004). Reasons for death in the two groups are listed in Table 4. Reduction of relative risk for death was 0.20 (95% confidence interval: 0.07–0.58), and the number needed to treat was 1.7. Number of ICU- and hospital-free days was higher in CPAP than in control [28 (0–28) and 133 (0–170) days versus 0 (0–28) and 0 (0–151) days, respectively; P = 0.0006].
Pneumonia occurred in 13 patients of the control and 5 patients of the CPAP group (P = 0.025), while sepsis was observed in 13 patients of the control group and 2 patients of the CPAP group (P = 0.001).
Discussion
The present study demonstrates that early treatment of early respiratory symptoms with noninvasive CPAP may prevent evolution to acute lung injury requiring ventilatory support and ICU admission of immunosuppressed patients with hematological malignancy who do not have a diagnosis of pneumonia, infection, and/or sepsis. These data should provide the preliminary evidence required to motivate a confirmatory multicenter study.
It is important to review the weaknesses of the study before discussing its implications. First, the study was unblinded. We attempted to limit potential bias by having an explicit set of objective criteria for admission to the ICU; for ethical reasons, patients could be admitted to the ICU even if they did not meet these criteria, if the attending physician deemed it necessary. Only two (one in each group) patients admitted to the ICU did not fulfill these criteria, while all patients fulfilling these criteria were admitted to the ICU. Most importantly, however, if patients in the CPAP group were systematically being kept from the ICU, one would expect that clinical outcome in the CPAP group might be worse than in the control group. In fact, mortality was significantly lower in the CPAP group, strongly suggesting that the decrease in admissions to the ICU in the CPAP group was due to a beneficial clinical effect rather than due to the unblinded nature of the intervention. Second, as part of both interventions we used a protocol team (senior resident and an experienced ICU nurse). Although evidence for the effectiveness of a critical care outreach team is controversial [18], one possibility was that the CPAP group received closer medical monitoring than the control group, and that this was the reason for the improved outcome. This seems unlikely; a recent study found that a medical emergency team similar to the one implemented in our study had no impact on patient outcome [18]. However, post hoc analysis of the trial showed that a high rate of interventions performed by the critical care outreach team was associated with better outcome [19]. In the present study, the number of calls and orders given by the protocol team did not differ between control and CPAP (Table 2), suggesting that the CPAP group did not receive increased medical attention. Third, we studied a relatively small number of patients. Obtaining a statistically significant decrease in mortality with such a small number of patients (and events) implies a powerful treatment effect, or suggests the play of chance. Fourth, interventions tested in a single clinical site may not be automatically exported to a broader population, since large effect sizes may not be replicated in multicenter effectiveness trials [20]. Fifth, results of the present study could be attributed to a late ICU admission policy rather than to efficacy of CPAP in preventing evolution of ALI. Although deterioration of oxygenation requiring ventilatory support is not the only reason for ICU admission, analysis of the SAPS 3 database (13,322 patients enrolled at ICU admission) [21] and of the Mechanical Ventilation International Study Group (15,757 patients enrolled at ICU admission) [22] shows that the PaO2/FiO2 ratio on ICU admission was 261 ± 137 (P.G. Metnitz, pers. comm.) and 197 ± 115 (A. Esteban, pers. commun.), respectively. In our study, on initial respiratory symptoms, treatment with O2 administration led to PaO2/FiO2 ratio of 398 ± 15 while administration of O2 plus CPAP led to PaO2/FiO2 ratio of 441 ± 10 (Table 1). Under these circumstances, patients included in the present study could be treated in ward and not in ICU, provided that appropriate monitoring and clinical support from the ICU was provided to medical personnel of the ward.
Chemotherapy and transplantation markedly improved the outcome of patients with hematological malignancy [3]. However, the associated immunosuppression limits the efficacy of these therapies [1]. Pulmonary complications, described in about half of patients with neutropenia [13], are thought to worsen clinical outcome in about 20% of patients [23]. These complications may evolve into ALI and require transfer to ICU for mechanical ventilation [24]. Although use of noninvasive mechanical ventilation [25] and earlier recognition of chemotherapy toxicity [26] have remarkably advanced quality of patient care, the number of ICU beds remains limited, and questions related to the ethics of admitting such patients to the ICU are still raised [27].
Of the 522 patients with hematological malignancy and neutropenia enrolled in our study period, 69 patients (13%) developed early alterations of respiratory function. These data are consistent with previous studies [28, 29]. Infusion of large volumes of fluid combined with cardiac and renal dysfunction caused by previous chemotherapy, bilateral lung consolidation caused by commonly used cytotoxic drugs, and the diffuse alveolar damage with interstitial mononuclear cell infiltrate that frequently occur after bone marrow transplant [16, 17] may explain why attending hematologists reported initial respiratory symptoms as associated with (1) alveolar infiltrates (ten patients in control and nine patients in CPAP), (2) alveolar and interstitial infiltrates (eight patients in control and ten patients in CPAP), and (3) interstitial infiltrates compatible with idiopathic interstitial pneumonia (two patients in control and one in CPAP).
Conventional treatment of hypoxemia in the hematological ward consists of increasing the fractional concentration of inspired oxygen [12, 25]. CPAP, by maintaining positive pressure at the airway opening throughout the ventilatory cycle, helps to prevent alveolar collapse, and reduces intrapulmonary shunt [30]. CPAP was used for 16.3 ± 3.8 h per day for 10.8 ± 6.9 days with no episodes of intolerance. These results may reflect the use of CPAP through a helmet rather than through a face or nasal mask [31]. Recent studies have demonstrated that intolerance to ventilatory treatment, skin necrosis, gastric distension, and eye irritation were less common with helmet than with face-mask [32]. These underlying mechanisms may therefore explain the efficacy of CPAP in preventing evolution of initial respiratory symptoms to ALI [8, 9]. Moreover, previous studies showed that clearance of pulmonary densities by early use of CPAP might prevent occurrence of pneumonia and sepsis [8, 33, 34].
Our study is different from a number of other studies [35, 36] in that it did not include patients with recognized respiratory or systemic infections; rather it focused on patients who did not have a diagnosis of infection, but who had very early respiratory signs and symptoms. However, our definition of infection may be limited since we adapted the classic definition of sepsis and pneumonia to the situation of the hematologic patient with white cell count <1,000 cells/mm3. In terms of early intervention, our study is similar to the early use of CPAP in the out-of-hospital setting to treat acute cardiogenic pulmonary edema, which significantly reduced incidence of tracheal intubation and in-hospital mortality [7]; and the application of noninvasive ventilation, which is much more effective when applied early in patients with acute lung injury [37].
The efficacy of CPAP later in clinical course is controversial. Hilbert and coworkers found that CPAP was effective in preventing 25% of intubations in patients with hematological malignancy and neutropenia; their cohort included patients with infectious pulmonary diagnoses [35]. However, Delclaux and coworkers found that CPAP did not reduce intubation rate in patients with severe hypoxemic respiratory failure, most of whom had pneumonia (60%) [36].
In conclusion, this study demonstrates that early use of CPAP in the hematological ward in immunosuppressed patients with hematological malignancy, but without a secure diagnosis of infection, may prevent evolution of respiratory symptoms to acute lung injury requiring ventilatory support and ICU admission. Early use of CPAP appears to be a practical, simple, and inexpensive method to prevent worsening of respiratory complications in patients undergoing aggressive chemotherapy and intense immunosuppression.
References
Offidani M, Corvatta L, Malerba L, Marconi M, Bichisecchi E, Cecchini S, Manso E, Principi T, Gasparini S, Leoni P (2004) Risk assessment of patients with hematologic malignancies who develop fever accompanied by pulmonary infiltrates: a historical cohort study. Cancer 101:567–577
Rubenfeld GD, Crawford SW (1996) Withdrawing life support from mechanically ventilated recipients of bone marrow transplants: a case for evidence-based guidelines. Ann Intern Med 125:625–633
Thomas X (2009) Chemotherapy of acute leukemia in adults. Expert Opin Pharmacother 10:221–237
Hillman KM, Bristow PJ, Chey T, Daffurn K, Jacques T, Norman SL, Bishop GF, Simmons G (2002) Duration of life-threatening antecedents prior to intensive care admission. Intensive Care Med 28:1629–1634
McQuillan P, Pilkington S, Allan A, Taylor B, Short A, Morgan G, Nielsen M, Barrett D, Smith G, Collins CH (1998) Confidential inquiry into quality of care before admission to intensive care. BMJ 316:1853–1858
Principi T, Pantanetti S, Catani F, Elisei D, Gabbanelli V, Pelaia P, Leoni P (2004) Noninvasive continuous positive airway pressure delivered by helmet in hematological malignancy patients with hypoxemic acute respiratory failure. Intensive Care Med 30:147–150
Plaisance P, Pirracchio R, Berton C, Vicaut E, Payen D (2007) A randomized study of out-of-hospital continuous positive airway pressure for acute cardiogenic pulmonary oedema: physiological and clinical effects. Eur Heart J 28:2895–2901
Squadrone V, Coha M, Cerutti E, Schellino MM, Biolino P, Occella P, Belloni G, Vilianis G, Fiore G, Cavallo F, Ranieri VM (2005) Continuous positive airway pressure for treatment of postoperative hypoxemia: a randomized controlled trial. JAMA 293:589–595
Bersten AD, Holt AW, Vedig AE, Skowronski GA, Baggoley CJ (1991) Treatment of severe cardiogenic pulmonary edema with continuous positive airway pressure delivered by face mask. N Engl J Med 325:1825–1830
Ferreyra G, Long Y, Ranieri VM (2009) Respiratory complications after major surgery. Curr Opin Crit Care 15:342–348
(1992) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Gruson D, Hilbert G, Portel L, Boiron JM, Bebear CM, Vargas F, Bebear C, Reiffers J, Gbikpi-Benissan G, Cardinaud JP (1999) Severe respiratory failure requiring ICU admission in bone marrow transplant recipients. Eur Respir J 13:883–887
Karlin L, Darmon M, Thiery G, Ciroldi M, de Miranda S, Lefebvre A, Schlemmer B, Azoulay E (2005) Respiratory status deterioration during G-CSF-induced neutropenia recovery. Bone Marrow Transplant 36:245–250
Peigne V, Rusinova K, Karlin L, Darmon M, Fermand JP, Schlemmer B, Azoulay E (2009) Continued survival gains in recent years among critically ill myeloma patients. Intensive Care Med 35:512–518
Gruson D, Vargas F, Hilbert G, Bui N, Maillot T, Mayet T, Pillet O, Chene G, Gbikpi-Benissan G (2004) Predictive factors of intensive care unit admission in patients with haematological malignancies and pneumonia. Intensive Care Med 30:965–971
Worthy SA, Flint JD, Muller NL (1997) Pulmonary complications after bone marrow trans plantation: high-resolution CT and pathologic findings. Radiographics 17:1359–1371
Khurshid I, Anderson LC (2002) Non-infectious pulmonary complications after bone marrow transplantation. Postgrad Med J 78:257–262
Winters BD, Pham J, Pronovost PJ (2006) Rapid response teams–walk, don’t run. JAMA 296:1645–1647
Chen J, Bellomo R, Flabouris A, Hillman K, Finfer S (2009) The relationship between early emergency team calls and serious adverse events. Crit Care Med 37:148–153
Bellomo R, Warrillow SJ, Reade MC (2009) Why we should be wary of single-center trials. Crit Care Med 37:3114–3119
Metnitz PG, Metnitz B, Moreno RP, Bauer P, Del Sorbo L, Hoermann C, de Carvalho SA, Ranieri VM (2009) Epidemiology of mechanical ventilation: analysis of the SAPS 3 database. Intensive Care Med 35:816–825
Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart TE, Benito S, Epstein SK, Apezteguia C, Nightingale P, Arroliga AC, Tobin MJ (2002) Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 287:345–355
Kress JP, Christenson J, Pohlman AS, Linkin DR, Hall JB (1999) Outcomes of critically ill cancer patients in a university hospital setting. Am J Resp Crit Care 160:1957–1961
Pene F, Aubron C, Azoulay E, Blot F, Thiery G, Raynard B, Schlemmer B, Nitenberg G, Buzyn A, Arnaud P, Socie G, Mira JP (2006) Outcome of critically ill allogeneic hematopoietic stem-cell transplantation recipients: a reappraisal of indications for organ failure supports. J Clin Oncol 24:643–649
Hilbert G, Gruson D, Vargas F, Valentino R, Gbikpi-Benissan G, Dupon M, Reiffers J, Cardinaud JP (2001) Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med 344:481–487
Adam AK, Soubani AO (2008) Outcome and prognostic factors of lung cancer patients admitted to the medical intensive care unit. Eur Respir J 31:47–53
Garrouste-Orgeas M, Montuclard L, Timsit JF, Reignier J, Desmettre T, Karoubi P, Moreau D, Montesino L, Duguet A, Boussat S, Ede C, Monseau Y, Paule T, Misset B, Carlet J (2005) Predictors of intensive care unit refusal in French intensive care units: a multiple-center study. Crit Care Med 33:750–755
Jackson SR, Tweeddale MG, Barnett MJ, Spinelli JJ, Sutherland HJ, Reece DE, Klingemann HG, Nantel SH, Fung HC, Toze CL, Phillips GL, Shepherd JD (1998) Admission of bone marrow transplant recipients to the intensive care unit: outcome, survival and prognostic factors. Bone Marrow Transplant 21:697–704
Ho VT, Weller E, Lee SJ, Alyea EP, Antin JH, Soiffer RJ (2001) Prognostic factors for early severe pulmonary complications after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 7:223–229
Azoulay E (2009) Pulmonary infiltrates in patients with malignancies: why and how neutropenia influences clinical reasoning. Eur Respir J 33:6–8
Mehta S, Hill NS (2001) Noninvasive ventilation. Am J Respir Crit Care Med 163:540–577
Antonelli M, Pennisi MA, Pelosi P, Gregoretti C, Squadrone V, Rocco M, Cecchini L, Chiumello D, Severgnini P, Proietti R, Navalesi P, Conti G (2004) Noninvasive positive pressure ventilation using a helmet in patients with acute exacerbation of chronic obstructive pulmonary disease: a feasibility study. Anesthesiology 100:16–24
Antonelli M, Conti G, Bufi M, Costa MG, Lappa A, Rocco M, Gasparetto A, Meduri GU (2000) Noninvasive ventilation for treatment of acute respiratory failure in patients undergoing solid organ transplantation: a randomized trial. JAMA 283:235–241
Duggan M, Kavanagh BP (2005) Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology 102:838–854
Hilbert G, Gruson D, Vargas F, Valentino R, Chene G, Boiron JM, Pigneux A, Reiffers J, Gbikpi-Benissan G, Cardinaud JP (2000) Noninvasive continuous positive airway pressure in neutropenic patients with acute respiratory failure requiring intensive care unit admission. Crit Care Med 28:3185–3190
Delclaux C, L’Her E, Alberti C, Mancebo J, Abroug F, Conti G, Guerin C, Schortgen F, Lefort Y, Antonelli M, Lepage E, Lemaire F, Brochard L (2000) Treatment of acute hypoxemic nonhypercapnic respiratory insufficiency with continuous positive airway pressure delivered by a face mask: a randomized controlled trial. JAMA 284:2352–2360
Adda M, Coquet I, Darmon M, Thiery G, Schlemmer B, Azoulay E (2008) Predictors of noninvasive ventilation failure in patients with hematologic malignancy and acute respiratory failure. Crit Care Med 36:2766–2772
Acknowledgments
This article was supported by Regione Piemonte (CEP AN RAN 07) and Ministero dell’Università (PRIN RANI 07)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Squadrone, V., Massaia, M., Bruno, B. et al. Early CPAP prevents evolution of acute lung injury in patients with hematologic malignancy. Intensive Care Med 36, 1666–1674 (2010). https://doi.org/10.1007/s00134-010-1934-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1934-1