Abstract
Objective
We evaluated the procedure of postoperative inhalational sedation with sevoflurane using the Anaesthetic Conserving Device (ACD) with regard to recovery times, feasibility and consumption of anaesthetics in comparison to propofol.
Design and setting
Prospective, randomised, single-blinded, controlled study in a surgical intensive care unit (ICU) of a 1,000-bed academic hospital.
Patients and interventions
A total of 70 patients after elective coronary artery bypass graft surgery either received sevoflurane via ACD (n = 35) or propofol (n = 35) for short-term postoperative sedation in the ICU.
Measurements and main results
The primary endpoint was extubation time from termination of sedation. Recovery times, consumption of anaesthetics, endtidal sevoflurane concentrations, length of ICU and hospital stay, and side effects were documented. Mean recovery times were significantly shorter with sevoflurane than with propofol (extubation time: 22 vs. 151 min; following commands: 7 vs. 42 min). The mean (SD) sevoflurane consumption was 3.2 ± 1.4 mL/h to obtain mean endtidal concentrations of 0.76 vol%. No serious complications occurred during sedation with either sedative drug. The length of ICU stay was comparable in both groups, but hospital length of stay was significantly shorter in the sevoflurane group. Drug costs (in Euro) for sedation per patient were similar in both groups (sevoflurane: 15.1 ± 9.5 €; propofol: 12.5 ± 5.8 €), while sevoflurane sedation costs that included use of the ACD were significantly higher.
Conclusions
Sevoflurane administration via ACD is an effective and safe alternative to propofol to provide postoperative short-term ICU sedation. Recovery from sedation was facilitated with sevoflurane instead of propofol and resulted in shorter extubation and ventilator times.
Descriptor
Neurology/sedation, Sedation and anaesthesia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative and critically ill patients in the intensive care unit (ICU) are sedated to facilitate mechanical ventilation, and to avoid anxiety and stress responses from invasive manipulations and achieve normothermia and cardiovascular stability [1, 2]. No currently available sedative agent possesses the features of an “ideal” sedative for ICU sedation [3]. The most commonly used sedatives in ICU are midazolam and propofol [4], both of which have considerably negative side effects such as withdrawal symptoms and delirium, accumulation and tolerance effects [5, 6].
Volatile anaesthetics form a major part of general anaesthesia during surgical interventions, but have been scarcely used in the ICU due to the technical requirements of low-flow breathing systems and uneconomical volatile anaesthetic consumption in open ICU ventilator circuits. The Anaesthetic Conserving Device (ACD) was approved in 2005 for use in the ICU and represents a gas reflector comparable to low-flow anaesthesia conditions when connected between Y-piece and patient tube [7, 8]. Recently, isoflurane by use of the ACD has been evaluated compared to midazolam in small patient populations [9–11]. Sevoflurane, one of the latest contributions to the family of halogenated inhalative anaesthetics, shows potential advantages over isoflurane for its short duration of action, brief elimination time and rare side effects [12, 13]. In the operating room sevoflurane has been evaluated extensively, but few studies have reported on the use of sevoflurane via ACD in ICU patients [14–16].
The aim of the present randomised, single-blinded, controlled study was to evaluate the feasibility of sevoflurane via ACD in postoperative sedated patients following cardiothoracic surgery compared to a standard intravenous sedation regimen with propofol.
Methods
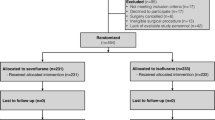
After approval from the ethical and governmental research committee (NCT 00586118) and informed written consent, 70 patients scheduled for elective coronary artery bypass graft (CABG) surgery were enrolled in this study. Inclusion criteria were patients of 18–80 years, 50–120 kg and ASA classification I–III. Exclusion criteria were ASA IV–V patients, severe cardiac impairment (ejection fraction <30%), renal insufficiency (serum creatinine >140 μmol/L) and dialysis, severe respiratory impairment, muscle disease, family history of malignant hyperthermia, central nervous system diseases (Parkinson’s disease, apoplexy with persisting paresis), psychic disorders, hepatic impairment (ALAT and/or ASAT >50 U/L), alcohol or drug abuse, and history of allergy to any of the study agents.
Intraoperative management
All the patients were premedicated orally with flunitrazepam 1–2 mg prior to induction of anaesthesia. A standardised induction protocol was applied using sufentanil (1 μg/kg), pancuronium bromide (0.1 mg/kg) and midazolam (0.07 mg/kg). After tracheal intubation, the lungs of the patients were ventilated with 40% oxygen-air to maintain normocapnia (arterial CO2 35–45 mm Hg). The radial artery was cannulated and a pulmonary artery catheter was placed routinely for measurements of cardiac index (CI), mean pulmonary and arterial pressures (MAP). Anaesthesia was maintained with sufentanil (1.5–2 μg/kg/h), sevoflurane (MAC 0.5–1) before and after cardiopulmonary bypass (CPB), midazolam (0.03–0.07 mg/kg) and pancuronium bromide (0.03 mg/kg). CPB was performed using a non-pulsatile flow heart lung machine; the circuit was primed with 1 L of Ringer’s solution and 0.5 L hydroxyethyl starch. Mild hypothermia (bladder temperature 32–33°C) and a CPB flow rate of 2.4 L/min/m2 were used. At weaning from CPB, dobutamine was given when MAP was <60 mmHg and CI was <2.5 L/min/m2 in spite of sufficient volume infusion (pulmonary capillary wedge pressure 11–14 mmHg). Norepinephrine was administered when systemic vascular resistance was <650 dyn sec/cm5 and MAP was <60 mmHg. Intraoperative volume management, urine output and drug administration, duration of surgery, anaesthesia, aortic cross clamping and CPB were noted.
Patient management in ICU
After surgery, patients were transferred to the ICU and sedation was started according to the randomisation (sealed envelopes) either with sevoflurane via ACD (n = 35) or propofol (n = 35). The single use ACD (SedanaMedical AB, Sundbyberg, Sweden) is a modified heat and moisture exchanger that allows the delivery of volatile anaesthetics, instilled through a syringe perfusion pump, via a miniaturised vaporiser directly into the breathing circuit of ICU ventilators (Fig. 1). The device is connected between the Y-piece of the respiratory circuit and the endotracheal tube. A charcoal membrane integrated within the ACD absorbs volatile anaesthetics during exhalation (to 90%) and then releases it by evaporation into the inspired gas during inspiration. Any exhaled sevoflurane that fails to condense on the filter is released through the expiratory outlet of the ventilator to an active coal scavenging system (Novasorb™, Novamed, Düsseldorf, Germany) to avoid environmental pollution. For the introduction of sevoflurane, a bolus of 1–2 mL was given and an infusion rate of 2–6 mL/h adjusted to obtain endtidal concentrations of 0.5–1 vol%. In the propofol group, intravenous propofol 2% was given initially in a dosage of 2 mg/kg/h with further adjustments to a maximum of 4 mg/kg/h.
Cross-sectional view of the Anaesthetic Conserving Device (ACD). In the inspiration the oxygen comes from the ventilator, passes through the ACD and delivers oxygen enriched with sevoflurane to the patient; in the expiration oxygen flows back to the ventilator, sevoflurane is stored in the charcoal membrane of the ACD and recycled during the next inspiration
Depth of sedation was adjusted to Richmond Agitation Sedation Scale (RASS) values of −4 to −3 [17], and bispectral index spectroscopy (BIS) values of 55–70 [18]. Analgesia during sedation was achieved by piritramide (a morphine derivate) boli 3–7.5 mg, given after a bolus of either sedative agent and increased BIS and RASS values. Inspiratory and expiratory sevoflurane concentrations and syringe pump delivery rates, consumption of propofol and other sedatives and analgesics were documented. All the complications deriving from the new device were documented. Sedation was stopped when patients were normothermic, showed stable haemodynamic (MAP 60–100 mmHg; HR 60–100/min) and respiratory parameters (paO2 > 70 mmHg; FiO2 < 0.4; paCO2 35–45 mmHg; pH 7.3–7.5).
Recovery profile was evaluated as time from termination of sedation to spontaneous eye opening, hand grip, following commands (looking to left/right side, showing tongue) and extubation, in accordance to previous publications [11, 19]. After extubation, patients were evaluated for personal, time and spatial orientation every 15 min in the first 2 h and thereafter every 30 min. The quality of sleep was documented as follows [20]: recall during loss of consciousness and wake-up in the ICU, dreams classified as pleasant, unpleasant and nightmares, visual or sensory sensations, pain, anxiety or fear, and recall of endotracheal tube during sedation.
Laboratory testing of liver, kidney and cardiac function were evaluated routinely in all patients (such as creatinine, urea; aminotransferases, creatine kinase). All the adverse side effects, such as shivering, postoperative nausea and vomiting, gastrointestinal symptoms, cerebral deterioration (agitation, withdrawal symptoms, inadequate and uncoordinated wake-up, delirium, apoplexia, epilepsia, etc.), haemodynamic instability, arrhythmias, respiratory problems, renal or hepatic failure, from extubation to discharge of hospital were documented. Readmissions to ICU, length of ICU and hospital stay and in-hospital mortality were noted. Costs were calculated separately for sedative and analgesic drugs and average total costs including materials.
Statistical analysis
Data are presented as mean ± SD, median (range) or number, unless otherwise stated. The data have been checked for normal distribution with the Kolmogorov–Smirnov test. The analysis of demographic parameters was tested with the student t test, while other normally distributed data were compared by an analysis of variance (ANOVA) for repeated measures. Continuous, non-normally distributed data were compared using the Wilcoxon Rank Sum test, and incidences were analysed with Fisher’s exact test. Previous published data of the same study centre were used to calculate an a priori power analysis, reporting an extubation time after propofol sedation in visceral surgical patients of 136.2 min [21]. A reduction in extubation time of 40% was seen as clinically relevant. With a power of 80% and a statistical error of α = 0.05 and β = 0.2, a total of 33 patients had been calculated to reach the study aim. Assuming possible drop-outs, the sample size was increased to 35 per study group. A P value of <0.05 was set for describing significance between the two study groups. The null hypothesis was set as no significant difference between sevoflurane and propofol.
Results
Of the 172 initially screened patients, 102 were excluded due to exclusion criteria and violation of the study protocol and a total of 70 patients were finally analysed. Patients in both groups were similar in terms of biometric and perioperative data, duration of surgery, anaesthesia, aortic cross clamping and CPB, and consumption of anaesthetics (Table 1). Duration of ICU sedation was comparable between the sevoflurane (8.1 ± 3.5 h) and the propofol group (8.4 ± 4.2 h), whereas ventilation time was significantly (P < 0.006) shorter following sevoflurane than propofol (9.0 ± 4.0 vs. 12.5 ± 5.8 h). Length of ICU stay was similar in both groups, whereas patients receiving sevoflurane left hospital significantly (P < 0.03) earlier than the propofol group (Table 2).
The median time (25th and 75th percentile) to extubation was significantly shorter (P < 0.001) with sevoflurane [21.5 min (8, 46 min)] when compared to propofol [150.5 min (69, 299 min)] (Fig. 2). Times of recovery from termination of sedation were significantly (P < 0.002) shorter in the sevoflurane group than in the propofol group (Fig. 2). BIS values did not differ significantly from admission to the ICU until 6 h after extubation in both groups (Fig. 3) nor RASS values. Dreams were recalled by six patients in the propofol and five in the sevoflurane group, no nightmares were reported in either group. One patient remembered visual hallucinations after sevoflurane. Adequate orientation was prompt in 19 patients after sevoflurane and 17 after propofol. Except for three patients in the sevoflurane and four in the propofol group that showed signs of delirium, all other patients recovered within 2 h from extubation.
Mean sevoflurane consumption was 3.2 ± 1.4 mL/h, while mean endtidal sevoflurane concentration was initially 0.5 vol% and increased to 1 vol% for adequate sedation levels after 6 h (Fig. 4). The sevoflurane bolus to initiate the inhalative sedation was 1.2 ± 0.5 mL. The mean administration of propofol was 2.4 ± 1.1 mg/kg/h, with an initially lower rate of 1.83 mg/kg/h and an increase to 2.9 mg/kg/h at 6 h postoperatively. Additional sedative agents were given in six of the propofol-treated patients due to paradox arousal and inadequate wake-up. The consumption of piritramide during ICU sedation was comparable between the sevoflurane and the propofol group (7.3 ± 7.2 vs. 7.7 ± 7.1 mg).
Routine laboratory parameters analysed preoperatively, at admission to the ICU and on the 1st postoperative day were similar in both study groups. Adverse events did not differ significantly between the groups (Table 2). Technical problems that originated from the ACD device were observed, such as an increase in carbon dioxide tension (>50 mmHg), false disconnection from the ventilator and sevoflurane loss during suctioning.
Costs for sedative drugs in Euro were 15.07 ± 9.47 € for sevoflurane and 12.51 ± 5.77 € for propofol. Total costs for inhalative sedation including device-related equipment was significantly higher with sevoflurane (65.49 ± 10.52 € per patient) than propofol (13.38 ± 5.91 € per patient).
Discussion
This is the first randomised trial on sevoflurane-based sedation via the Anaesthetic Conserving Device (ACD) compared to a standard intravenous regimen with propofol in elective postoperative cardiac surgery patients in ICU. The main results revealed a similar sedation quality and a significantly shorter emergence from sedation to recovery and extubation with sevoflurane than propofol.
Volatile anaesthetics are potent hypnotics that facilitate fast introduction and awakening and easy titration, and might therefore fulfil the properties of an ideal sedative [12, 22]. Administration of volatile anaesthetics using vaporisers in open non-rebreathing ICU ventilators is not cost-effective and requires a scavenging system to avoid environmental pollution. With the ACD system, a simple application of volatile agents has become feasible in the ICU [23]. The potential advantage is the storage of volatile gas within the ventilator circuit resulting in drug consumptions comparable to low-flow anaesthesia in the operating room [7, 8]. Using BIS and RASS as measures of depth of sedation, postoperative use of sevoflurane via ACD allowed easily titratable depth of sedation comparable to propofol sedation. Endtidal sevoflurane concentrations varied between 0.5 and 1 vol% (0.25–0.5 MAC), administered at a mean hourly delivery rate of 3.2 ± 1.4 mL. Our goal was to randomly assess sevoflurane-based sedation in the immediate postoperative period rather than in a heterogenous patient population suffering from sepsis or respiratory insufficiency, as reported by Soukup et al. [14]. Sevoflurane delivery had to be adjusted in our investigation after 2 h postoperatively and reached levels comparable to those described by Soukup et al. [14] in long-term critically ill patients.
The benefit of early recovery after inhalational ICU sedation has been reported by others [10, 11]. Hanafy et al. [10] evaluated isoflurane sedation in 12 patients following coronary artery bypass grafting and showed significantly shorter wake-up times and earlier mobilisation compared to midazolam. Even in prolonged inhalational sedation, extubation time was found to be significantly shorter with isoflurane than with midazolam [11]. Soukup et al. [14] showed a rapid recovery (mean 13 min) from sevoflurane sedation even after 95 h in 12 of 23 critically ill patients, 2 patients recovered at 50 and 106 min, all other patients were switched to an intravenous sedation concept.
The use of the ACD in the ICU setting revealed only minor problems deriving from false disconnection from the ventilator and suctioning, making inhalative sedation feasible in the ICU setting. We did not observe serious side effects, e.g. arrhythmias, shivering, PONV and delirium during and after sedation with either sedative agent.
Although attractive from a pharmacological profile, total costs were higher in the sevoflurane-treated patients due to the costs of the device itself. Sevoflurane showed favourable recovery properties in our postoperative cardiac surgery patients compared to propofol and less paradox arousals needing less nurse care. These differences might be even pronounced and important for the readiness of ICU discharge after prolonged sedation. Thus, inhalative sedation might be considered as an alternative to conventional propofol sedation in the future as propofol underlies formal restrictions and recommendations for the fear of a propofol-infusion-syndrome [1, 24]. In prolonged sedation, ICU patients often need different sedative substances including benzodiazepines, α2-agonists and ketamine. Volatile anaesthetics could be administered as single-use sedative and therefore bear the advantage of a low risk of accumulation and delayed recovery [11, 14].
Limitations
A sevoflurane-based sedation regime could be easily integrated in daily ICU work and provide a good quality of sedation at low end-tidal concentrations. The present randomised study was focussed on short-term postoperative sedation in a specific ICU population. Complications emerging from either the ACD or the prolonged use of sevoflurane in other ICU populations have not been evaluated. A postulated concern has been connected with sevoflurane exposure and the formation of inorganic fluorides, although no renal impairment in terms of polyuria and renal failure has been observed so far [25]. Sevoflurane exposure in our study was comparable to prolonged intraoperative use of sevoflurane and no kidney dysfunction was observed. Renal function secondary to prolonged use of sevoflurane for ICU sedation may need further investigation.
We noted that sevoflurane sedated patients were discharged earlier from hospital. A postulated bias might be that differences are based on logistic procedures, and are not due to sedation regimens. We tried to reduce bias in considering prolonged stays over week-ends in this analysis, furthermore anaesthesiologists were not involved in the discharge of the patients from hospital. Our patient population was small and the favourable reduction in hospital stay, which was not our primary outcome parameter, needs further confirmation in larger studies.
The use of volatile anaesthetics in the ICU has not been approved according to current drug-approval-laws. The “off-label” use of inhalational drugs in the ICU lies within the experience and responsibility of medical professionals.
Conclusions
Sevoflurane sedation using the Anaesthetic Conserving Device appears to be a valid and safe alternative to the commonly used intravenous propofol-based regimen. Sevoflurane provided a comparable sedation quality to propofol at low end-tidal concentrations of 0.5–1.0 Vol%. Patients showed a faster and more predictable return of recovery after sevoflurane, and shorter times of mechanical ventilation and hospital stay.
References
Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM, Crippen DW, Fuchs BD, Kelleher RM, Marik PE, Nasraway SA Jr, Murray MJ, Peruzzi WT, Lumb PD (2002) Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 30:119–141
Weinert CR, Sprenkle M (2008) Post-ICU consequences of patient wakefulness and sedative exposure during mechanical ventilation. Intensive Care Med 34:82–90
Martin J, Bäsell K, Bürkle H, Hommel J, Huth G, Kessler P, Kretz F, Putensen C, Quintel M, Tonner P, Tryba M, Scholz J, Schüttler J, Wappler F, Spies C (2005) Analgesia and sedation in ICU—S2-guidelines of DGAI. Anaesthesiologie und Intensivmedizin 46:S1–S20
Martin J, Franck M, Fischer M, Spies C (2006) Sedation and analgesia in German intensive care units: how is it done in reality? Results of a patient-based survey of analgesia and sedation. Intensive Care Med 32:1137–1142
Shafer A (1998) Complications of sedation with midazolam in the intensive care unit and a comparison with other sedative regimens. Crit Care Med 26:947–956
Ouimet S, Kavanagh BP, Gottfried SB, Skrobik Y (2007) Incidence, risk factors and consequences of ICU delirium. Intensive Care Med 33:66–73
Tempia A, Olivei MC, Calza E, Lambert H, Scotti L, Orlando E, Livigni S, Guglielmotti E (2003) The anesthetic conserving device compared with conventional circle system used under different flow conditions for inhaled anesthesia. Anesth Analg 96:1056–1061
Enlund M, Lambert H, Wiklund L (2002) The sevoflurane saving capacity of a new anaesthetic agent conserving device compared with a low flow circle system. Acta Anaesthesiol Scand 46:506–511
Berton J, Sargentini C, Nguyen JL, Belii A, Beydon L (2007) AnaConDa reflection filter: bench and patient evaluation of safety and volatile anesthetic conservation. Anesth Analg 104:130–134
Hanafy M (2005) Clinical evaluation of inhalation sedation following coronary artery bypass grafting. Br J Anaesth 21:237–242
Sackey PV, Martling CR, Granath F, Radell PJ (2004) Prolonged isoflurane sedation of intensive care unit patients with the Anesthetic Conserving Device. Crit Care Med 32:2241–2246
Behne M, Wilke HJ, Harder S (1999) Clinical pharmacokinetics of sevoflurane. Clin Pharmacokinet 36:13–26
Patel SS, Goa KL (1996) Sevoflurane. A review of its pharmacodynamic and pharmacokinetic properties and its clinical use in general anaesthesia. Drugs 51:658–700
Soukup J, Schärff K, Kubosch K, Rudzki M, Zielonka M, Radke J (2007) Sedation concepts with volatile anesthetics in intensive care: technical application and current experiences. Intensiv und Notfallbehandlung 32:29–36
Röhm KD, Wolf M, Boldt J, Schöllhorn T, Schellhaass A, Piper SN (2008) Short-term sevoflurane sedation using the anaesthetic conserving device AnaConDa after cardiac surgery: feasibility, recovery and clinical issues. Crit Care 12(Suppl 2):P270
Belda JF, Soro M, Badenes R, Meiser A, Garcia ML, Aguilar G, Marti FJ (2008) The predictive performance of a pharmacokinetic model for manually adjusted infusion of liquid sevofluorane for use with the Anesthetic-Conserving Device (AnaConDa): a clinical study. Anesth Analg 106:1207–1214
Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, Francis J, Speroff T, Gautam S, Margolin R, Sessler CN, Dittus RS, Bernard GR (2003) Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 289:2983–2991
Johansen JW, Sebel PS (2000) Development and clinical application of electroencephalographic bispectrum monitoring. Anesthesiology 93:1336–1344
Röhm KD, Riechmann J, Boldt J, Schöllhorn T, Piper SN (2007) Do patients profit from physostigmine in recovery from desflurane anaesthesia? Acta Anaesthesiol Scand 51:278–283
Rundshagen I, Schnabel K, Wegner C, am Esch S (2002) Incidence of recall, nightmares, and hallucinations during analgosedation in intensive care. Intensive Care Med 28:38–43
Piper SN, Kumle B, Maleck WH, Suttner SW, Fent MT, Boldt J (2001) Effects of postoperative sedation with propofol and midazolam on pancreatic function assessed by pancreatitis-associated protein. Anaesthesia 56:836–840
Campagna JA, Miller KW, Forman SA (2003) Mechanisms of actions of inhaled anesthetics. N Engl J Med 348:2110–2124
Enlund M, Wiklund L, Lambert H (2001) A new device to reduce the consumption of a halogenated anaesthetic agent. Anaesthesia 56:429–432
Vasile B, Rasulo F, Candiani A, Latronico N (2003) The pathophysiology of propofol infusion syndrome: a simple name for a complex syndrome. Intensive Care Med 29:1417–1425
Bito H, Atsumi K, Katoh T, Ohmura M (1999) Effects of sevoflurane anesthesia on plasma inorganic fluoride concentrations during and after cardiac surgery. J Anesth 13:156–160
Acknowledgments
The present study was an investigator-initiated trial granted by the hospital and department sources of the Klinikum Ludwigshafen, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Röhm, K.D., Wolf, M.W., Schöllhorn, T. et al. Short-term sevoflurane sedation using the Anaesthetic Conserving Device after cardiothoracic surgery. Intensive Care Med 34, 1683–1689 (2008). https://doi.org/10.1007/s00134-008-1157-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1157-x