Abstract
Background
Young people with disabilities have poorer mental health than their non-disabled peers. However, people with disabilities are more likely than others to experience financial hardship and low social support, both of which have been linked with poor mental health outcomes. This article explores the extent to which the relatively poor mental health of young people with disabilities is related to the social conditions in which they live.
Methods
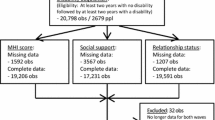
Secondary analysis was performed on Wave 6 (2006) of the survey of Household Income and Labour Dynamics in Australia (HILDA). This nationally representative sample included 3,392 young Australians, aged 15–29, of whom 475 reported having a long-term health condition, impairment or disability.
Results
Young people with disabilities reported poorer mental health than their non-disabled peers. However, this relationship was moderated by both social adversity and social support, with minimal differences in mental health observed between the groups under conditions of high social support and low financial hardship.
Discussion
The results suggest that disability represents a potential adversity that may be exacerbated or ameliorated by the effects of wealth/financial hardship and social support.
Conclusion
It may be possible to improve the mental health of disabled people by addressing their social exclusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The number of young Australians who live with a long-term disabling condition is growing rapidly as a result of a number of factors including increased survival rates for young children with a disability and the increasing incidence of chronic conditions such as diabetes and asthma in adolescence [50, 56]. It is widely accepted that young people with disabling conditions do not have the same health and social outcomes as non-disabled young people [60]. In particular, the mental health of young people with disabling conditions has been found to be worse than that of other young people [23, 45, 68], a particular concern given the high prevalence and serious impact of mental health problems in this age group. In Australia, for example, it is estimated that 14% of children and adolescents and 27% of young adults (18–24) have mental health problems, while mental disorders account for 61% of the non-fatal burden of disease for young Australians [2, 9, 55].
It is increasingly being recognised that the social correlates of disability may play an important part in the relationship between disability and mental health [e.g. 22]. Many studies have shown that people with disabilities are more likely than others to experience financial hardship and inadequate social support [e.g. 28, 36, 68]. For example, in our previous analyses of a national sample of young Australians, those with a chronic health condition, impairment or disability reported receiving less social support, having less social contact with their friends and relatives, being less satisfied with their spare time activities and friendships and feeling less like a part of their local community. They were also more likely to report income poverty, financial strain and hardship [23]. The increased hardship and reduced social support reported by young people with disabilities is particularly problematic given that mental health has been linked with both social support [e.g. 26, 38, 66] and socio-economic status [e.g. 24, 25, 27, 55].
Missing from the literature is an in-depth analysis of how living conditions might influence the established association between disability and mental health amongst adolescents and young adults.
This study explores the relationship between mental health, disability status, social support and financial hardship for young Australians.
Method
Data
We undertook secondary analysis of Wave 6 (2006) of the survey of Household Income and Labour Dynamics in Australia (HILDA). HILDA is a non-refreshed panel survey originating from a national probability sample of approximately 7,500 Australian households in 2001. It is funded by the Australian Government and designed and managed by a group comprising the Melbourne Institute of Applied Economic and Social Research; the Australian Council for Educational Research; and the Australian Institute of Family Studies. HILDA collects information about the employment, economic and subjective wellbeing, health and family dynamics of Australians through interviews with household members of 15 years and older. Full details of HILDA are available in a series of technical reports and annual reports [33, 35, 64].
Measures
Mental health is measured in HILDA using the Mental Health Scale of the SF-36 [63], a self-administered survey designed for people 14 years and older [62]. The Mental Health Scale measures symptoms of depression, anxiety and positive mental health. Participants are asked five questions about how they have been feeling in the past 4 weeks, to which they respond on a 6-point scale from “all of the time” to “none of the time”. This is a widely used, valid and reliable scale that has been shown to be useful in identifying common mental disorders in community and clinical samples [e.g. 14, 53]. We analysed mental health in two ways, using normalised scale scores and a binary indicator of poor mental health. For the latter, a score of below 50 was used to indicate poor mental health, a well-accepted cutoff representing the lowest 9.6% of the Australian population (15 years and over) and the approximate mean score for Australians with depression [1, 19].
To ascertain the presence of disability, participants in HILDA are asked whether they had “any long-term health condition, impairment or disability that restricts you in your everyday activities and has lasted, or is likely to last, for 6 months or more.” Seventeen examples are provided including: speech, hearing or uncorrected sight problems, learning difficulties, conditions that restrict physical activity and difficulty breathing. Participants then specify which disability or disabilities they have. For this study, we were interested in investigating the mental health of people with physical, sensory or intellectual conditions. Therefore, we excluded from our disability group participants whose only disability was psychiatric as defined by two items: “mental illness which requires supervision” or “nervous or emotional condition which requires treatment”. This meant that people with a psychiatric disability were allocated to the “disability” group only if they also reported a physical, sensory or intellectual impairment, and to the “no disability” group if they did not.
HILDA measures social support using 10 items (see Table 1). Participants were allocated to the high or low social support group based on a median split on a composite measure based on the sum of these items. Given that there is no established cutoff point for this scale, median split was used to avoid the influence of extreme values and because it results in groups of equal sizes in a non-normal distribution.
We defined financial hardship as high if participants reported any one or more of 7 experiences indicating significant financial hardship (see Table 1). Participants answering ‘no’ to all 7 items were allocated to the low financial hardship group.
All analyses were undertaken on data weighted to correct for cross-sectional unit non-response. Weights are included in the HILDA dataset (see http://www.melbourneinstitute.com/hilda/ for details). To explore the interactions between disability, financial hardship, social support and mental health, we completed analyses for males and females separately as research suggests that different patterns may emerge [37, 38].
Results
The wave 6 sample consisted of 3,392 young people (aged 15–29), of whom 475 reported having a physical, sensory or intellectual disability. The weighted prevalence of disability is 13%, which is within the range reported by other population-based surveys [11].
Overall and for both males and females, young people with a disability had significantly lower mental health scores than their non-disabled peers and were much more likely to score below 50 on the Mental Health Scale of the SF-36, indicating poor mental health (see Table 2).
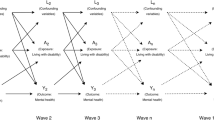
We used linear regression to investigate the association between disability status, financial hardship, social support and normalised SF-36 score and logistic regression to investigate the association between disability status, financial hardship, social support and ‘caseness’ on the SF-36. These analyses involved two stages. In the first stage, we tested for main effects. In the second stage of the analysis, we entered all second- and third-order interaction terms.
In the first stage of the analyses, all main effects were highly statistically significant for all analyses. For men, inclusion of the interaction terms marginally increased the fit of the models (R 2 change +0.024 P < 0.001 for normalised SF-36 score, Nagelkerke pseudo R 2 change +0.018 P = 0.023 for ‘caseness’ on the SF-36). For normalised SF-36 score, all interaction terms were significant (P < 0.01). For mental health ‘caseness’, the three-way interaction term and disability by hardship were significant (P < 0.05), with disability by social support (P = 0.079) and social support by hardship (P = 0.051) approaching significance. For women, inclusion of the interaction terms significantly increased the fit of the model for normalised SF-36 score (R 2 change +0.009, P = 0.002), but not for mental health ‘caseness’ (Nagelkerke pseudo R 2 change +0.009 P = 0.14). All interaction terms were significant in the final model (P < 0.01) for normalised SF-36 score. For mental health caseness, disability by hardship was significant (P < 0.05), with disability by support (P = 0.072), support by hardship (P = 0.074) and the three-way interaction term (P = 0.063) approaching significance.
We used visual plots of cell percentages to explore these interaction effects.
Inspection of cell means for normalised scores (Figs. 1, 2) and cell percentages for low mental health (Figs. 3, 4) indicated the following:
-
1.
Under favourable social conditions (low financial hardship and high social support) there is minimal difference between mental health scores or risk of poor mental health for young people with a disability when compared to non-disabled young people. For women, the residual differences were not statistically significant (mean normalised SF-36 score 0.30 vs. 0.31, t(684) = 0.18, P = 0.86; ‘caseness’ 4.8 vs. 3.4%, OR = 1.46, 95% CI 0.42–5.04, P = 0.47). For men, the residual differences were not statistically significant for normalised SF-36 score (mean 0.36 vs. 0.55, t(77) = 1.85, P = 0.069), but remained significant for mental health ‘caseness’ (5.9 vs. 0.6%, OR = 10.33, 95% CI 2.26–47.22, P = 0.005). To highlight any differences between adolescents (15–19 years old) and young adults (20–29 years old) we explored residual differences by age. Residual differences were not statistically significant for adolescents (mean normalised SF-36 score 0.36 vs. 0.44, t(480) = 0.78, P = 0.44; ‘caseness’ 4.0 vs. 3.2%, OR = 1.24, 95% CI 0.27–5.64, P = 0.68). For young adults, residual differences were not statistically significant for mean normalised SF-36 score (0.31 vs. 0.41, t(91) = 0.96, P = 0.34), but were for mental health ‘caseness’ (5.0 vs. 1.4%, OR = 3.58, 95% CI 1.10–11.69, P = 0.048).
-
2.
People with lower social support have poorer mental health and greater risk of mental health problems for all groups. This effect is stronger for people with disabilities than for their non-disabled counterparts.
-
3.
Financial hardship is generally associated with lower mental health scores and higher risk of poor mental health; however, there are some unexpected findings. Under conditions of low social support, financial hardship has a particularly strong association with mental health for men with disabilities for whom the risk of poor mental health is around 18% under low hardship and 70% under high hardship conditions. This is apparently not the case for women with disabilities. Normalised mental health scores are similar for high and low hardship groups and the risk of poor mental health is actually lower for those in the high hardship group.
To try to tease out the unexpected finding for women, we investigated the relationship between social support, financial hardship and mental health for disabled and non-disabled women in three age groups (15–19, 20–24 and 25–29). No clear trends were observed by age.
Discussion
Principal findings
The findings are consistent with previous studies that have reported that young people with disabilities have poorer mental health than other young people. The results add to the existing literature in suggesting that between-group differences may be highly contingent on the social and material conditions under which people are living. Under conditions of higher social support and lower financial hardship there are no statistically significant differences between young women with and without disabilities or between men with and without disabilities on normalised mental health scores. There were, however, differences between young men with and without disabilities on “caseness” as indicated by a low mental health score.
Strengths and limitations
The main strengths of the study were the use of: (1) a large nationally representative cohort of Australian young people with a good response rate and (2) a well-validated measure of mental health. The main limitations were: (1) the self-report format for identifying disability, (2) the heterogeneity of disability within the broad group, (3) the cross-sectional nature of the study, and (4) the exclusion of some young people from the sample.
People with disabilities are identified in the HILDA survey using a single-item global disability question (with examples). The self-report format is in common with much previous research in this area. However, the identification of disabled people within generic household surveys is not straightforward and there is no universally accepted method for doing so. Prevalence estimates for disability vary somewhat with the definitions and data collection methods used [8, 11, 46]. HILDA uses the measure of disability identified as most appropriate by the Australian Bureau of Statistics based on the concept of disability as it is defined by the International Classification of Functioning, Disability and Health (ICF) [3].
Disability is a complex concept arising from a model that incorporates health condition, impairment, limitations, restrictions, and personal and environmental factors, which is difficult to capture in a single measure [46]. In this study and elsewhere it represents a very wide grouping which includes a range of conditions which vary widely in their impact and implications. Nevertheless, it is a grouping widely used for development of social policy and human rights and other legislation and thus remains a worthy group for analysis. The results of this study are consistent with the few studies to report on similar issues within specific impairment based groups [e.g. 22]. However, the heterogeneity of the disabled group means that overall results may not necessarily hold for all particular sub-groups whether defined by health condition, impairment, ethnicity or other specific variables.
The cross-sectional nature of the study limits the conclusions that can be drawn. The associations described here are likely to reflect the influence of social support and financial hardship on mental health, based on a considerable literature, including longitudinal studies that identify these factors as determinants of mental health [42, 51, 58, 67]. However, the results may also reflect the influence of mental health on social adversity, as poorer mental health can lead to reduced social networks and financial difficulty. Unmeasured third variables (e.g. family factors) may also have an impact on both social adversity and mental health problems. It is not possible within a cross-sectional study to differentiate the respective contributions of these mechanisms.
The HILDA survey is conducted on a nationally representative sample of households obtained through multistage sampling (census collection districts, dwellings, households). While about 92% of Australians live in private dwellings [6], findings cannot be generalised to specific populations that are not sampled, including homeless people or those living in institutions. People living in remote and sparsely populated areas were also excluded from the sample and this reduced the reference population by about 80,000 altogether [65] or around 0.5%. While indigenous people are more likely than other Australians to live in remote areas [7], they are well represented generally as the overall proportion of indigenous young Australians (15–29) participating in HILDA is a little higher than national estimates [5] (4.1 and 3.2% respectively). Even within households, some groups of people with disabilities were excluded from this analysis. The SF-36 is part of the self-completion section of HILDA, which involves a written questionnaire. HILDA interviewers are instructed not to issue this questionnaire to people who are unable to complete it themselves. This would therefore exclude people who cannot read or write. Further, the SF-36 has not been adequately tested to ensure its validity or reliability with people with intellectual disabilities, who make up 7.9% of the disabled sample.
Meaning of principal findings
These findings support other studies that have demonstrated that financial hardship and social support are primary mechanisms which link socially disadvantaged groups, such as single mothers, to poorer mental health [19] and that the impact of health conditions and disabilities can be exacerbated or ameliorated by socio-economic, demographic and family factors [21, 23, 31, 68].
The findings are also consistent with frameworks arising from the study of resilience [41, 58], which suggest that coping may be disrupted by combinations of stressors, with the presence of one stressor making people more vulnerable to the effects of other stressors. Smith et al. [58], in a longitudinal study of over 12,000 people found that wealth measured prior to the onset of a disability protected participants’ well-being from some of the negative effects of a new disability, though even less wealthy participants had recovered some of their well-being by 2 years. They postulated that financial resources helped participants deal with the practical demands of an illness or disability and could also act as a psychological buffer against the decline in well-being. Wight et al. [66] found from a representative sample of 18,417 adolescents that, while high perceived social support was protective against poor mental health, this effect was reduced in areas of socio-economic disadvantage when compared to wealthier areas. The reserve capacity model proposed by Gallo and Matthews [27] conceptualises the existence of a resource bank consisting of tangible, personal and social resources that people use when coping with negative life events or circumstances. They propose that people who live in worse socio-economic situations have lower ‘reserve capacity’ in this resource bank because they are exposed to more situations in which they must use their resources and because their circumstances prevent them from developing and replenishing these resources. These circumstances include lack of material resources to cope with any negative events, neighbourhoods characterised by deficient community resources and high rates of crime and violence, and high risk of several other factors such as marital breakdown and substance abuse that reduce social support.
Having a disability had a greater association with risk of poor mental health for men than for women (OR = 4.25 vs. 1.75). This is consistent with research amongst children and adolescents that has suggested that the emotional impact of having a disabling condition is greater for males than females [49]. This may be linked to the traditional construction of masculinity through bodily performance, independence and physical dominance, all of which can be threatened by disability [18].
The finding that for women with disabilities and low social support, the addition of another adversity—financial hardship—is actually associated with lower risk of mental ill-health is difficult to explain, especially given the strong opposite relationship between financial hardship and mental ill-health for men in a similar situation. This finding should be treated with caution as the numbers are quite small for the low social support groups (N = 40). Further research is needed to ascertain whether it is replicated rather than anomalous and, if so, the meanings and mechanisms behind it.
Previous research on the mental health of young people with disabling conditions has primarily explored the extent to which young people with particular conditions experience worse mental health than the general population. Many studies examining the relationship between disability and mental health for young people have focused on specific conditions. In these studies, the measurement of mental health and outcomes has varied. For example, while one study found that young people with sickle cell disease had higher levels of depression and lower self-esteem [57], others reported no difference in body image, self-esteem or mental health (on the SF-36) when compared to a control group [15, 44]. For other conditions findings are less controversial. For example, it is well established that children and adolescents with intellectual disabilities are considerably more vulnerable to mental health problems than other young people and that elevated levels of psychopathology persist into young adulthood [20, 32, 39]. Research comparing psychological outcomes across conditions [e.g. 59, 61] typically results in differential outcomes for each condition. However, when young people with a wide variety of long-term conditions are considered as a population group the evidence overall points to higher risk for negative mental health outcomes such as low emotional wellbeing, poor body image and suicide [23, 45, 48, 68]. Exploration of factors influencing this relationship has usually been limited to condition-related factors (such as severity), individual characteristics (such as intelligence) and family factors (such as cohesiveness) [17]. The current research demonstrates the importance of wider social and economic factors influencing the impact of disability on mental health.
Implications
Because this analysis is based on cross-sectional data it cannot be concluded that the relatively poor mental health of young people with disabilities can be attributed to social and material disadvantage. However, in the context of a considerable literature that demonstrates a temporal sequence in a variety of different populations it suggests that social support and financial hardship may play a part in determining the consequences of disability for mental health [42, 51, 58, 67]. This highlights the importance of social and fiscal policies that reduce the odds that young people with disabilities will be exposed to social exclusion.
First, there exists abundant evidence that exposure to poverty during childhood can have a detrimental effect on health, well-being and the incidence of disability during childhood and across the lifecourse [e.g. 40, 52, 69]. As such, social policies aimed at reducing income inequality could be expected to have an impact on both reducing the incidence and prevalence of disability and reducing the association between poverty and disability.
Second, the association between poverty and disability is exacerbated by the exclusion of people with disabilities from the labour market [28, 29]. Compared to other working-age Australians, people with disabilities have a lower labour force participation rate (53 compared to 81%) and a higher unemployment rate (8.6 compared to 5.0%) [4]. Unemployment contributes to financial hardship, social network contraction and psychological distress [16, 47] with evidence that the psychological impact of workforce exclusion due to sickness or disability is greater for younger people than older adults [25]. It is therefore important to ensure that policies facilitate employment for young people with disabilities and also for their carers, whose loss of earnings also contribute to poverty [29]. As precarious employment, such as casual work, is associated with poor mental health outcomes policy needs to be particularly directed to ensuring stable and flexible employment [69]. Although the Australian Disability Discrimination Act 1992 makes it unlawful for employers to discriminate on the grounds of disability and requires them to make “workplace accommodations” for workers with disabilities who can perform the essential activities of the job, there is evidence that improvements in this area since the introduction of the act have been slow [30]. For example, the gap in participation and unemployment rates between people with and without disabilities did not narrow in the 10 years to 2003 [10], or, for young people, between 2001 and 2006 [23].
Third, social protection needs to be made available for those who are unable to work or unable to provide for themselves sufficiently through work. Countries with the most comprehensive and generous social protection systems, like the Nordic countries, have the lowest overall rates of poverty and the lowest rates of relative poverty for ‘at risk’ groups such as single parents and the elderly [69]. The Commission on Social Determinants of Health has recommended that governments increase the generosity of their social protection systems towards a level that is sufficient for people with disabilities and other vulnerable groups to live “flourishing” lives and participate in their communities. Yet research suggests that, in Australia, income support payment rates for people with a disability have failed to take account of the considerable extra costs associated with disability, resulting in people with disabilities facing high rates of poverty and hardship [54].
Finally, social policies will also need to address other key dimensions of the social exclusion experienced by people with disabilities, including exclusion from political engagement and civic participation and exclusion from social interaction and support [13]. These are likely to involve broad-based policies that address such issues as: public attitudes and stigma associated with disability, disability discrimination, the physical accessibility of community resources and the accessibility of information. Such policies need to address the heterogeneity of disabling conditions and the complexity associated with ensuring meaningful inclusion for all disability types.
Future research
Longitudinal research examining the diverse pathways of young people with disabilities both into and out of financial hardship, social exclusion and mental health problems will help to unravel why some young people with disabilities are more resilient and others are more vulnerable to poor mental health. Patterns may vary according to the health conditions or impairments associated with disability as well as contextual factors. Such research will also help to identify issues that are particular to this age group. These issues may not be apparent in research using adult samples as the prevalence of disabling conditions is skewed towards older age groups. For example, an Irish longitudinal study of adults found that although people who had an illness or disability throughout the entire 7-year study had lower levels of social participation than others, the onset of disability was only associated with significantly reduced participation when it severely hampered the individual. Becoming non-disabled did not have a significant impact on social participation [28]. This may suggest that transitions into and out of disability during adulthood might have less social impact than being disabled as an adolescent or young adult as social networks are better established and disability is more common among older people. The authors are currently undertaking a longitudinal examination of HILDA data in relation to young people with disabilities which will address these issues.
There are a number of factors which may influence the mental health and financial and social situations of young people with disabilities that were not within the scope of this broad analysis. These include diagnostic category, recency of diagnosis, household structure, marital and parental status and disability severity or need for assistance. These features, unlike social support and financial hardship, are not a target for government policy but future study of their influence may provide information on specific groups who are most in need of intervention to prevent social exclusion.
Conclusion
People with disabilities must cope, not only with physical symptoms and functional limitations, but also “the negative and often punitive societal and social responses” to disability which can have a negative impact on the individual’s social world and self-image [12, p. 206]. Many appear to cope well with these difficulties, demonstrating similar mental health to non-disabled people under advantageous social circumstances. However, young people with disabilities are more likely than their peers to live under conditions that are detrimental to their mental health including financial hardship and low social support [23]. These stressors may deplete their resources to below the level at which effective coping can occur, resulting in reduced mental health and a higher risk of mental health problems.
Our findings offer the possibility that the higher reported risk of poor mental health outcomes amongst young people with disabilities may be modifiable, not inevitable as generally portrayed. This is consistent with approaches to social policy that focus on the environment of people with disabilities, addressing issues such as financial hardship and social support to improve well-being [23].
References
Australian Bureau of Statistics (1997) SF-36 population norms: Australia. ABS, Canberra
Australian Bureau of Statistics (1998) Mental health and wellbeing: profile of adults, Australia, 1997. ABS, Canberra
Australian Bureau of Statistics (2003) Information paper: disability, ageing and carers, Australia: user guide 2003. ABS, Canberra
Australian Bureau of Statistics (2005) Australian social trends 2005. ABS, Canberra
Australian Bureau of Statistics (2007) 20680-indigenous status by age—Australia. ABS, Canberra
Australian Bureau of Statistics (2007) Basic community profile 2006 census community profile series. ABS, Canberra
Australian Bureau of Statistics (2008) Australian social trends 2008: population distribution. ABS, Canberra
Australian Institute of Health, Welfare (2003) Disability prevalence and trends. AIHW, Canberra
Australian Institute of Health, Welfare (2007) Young Australians: their health and wellbeing 2007. AIHW, Canberra
Australian Institute of Health, Welfare (2008) Disability in Australia: trends in prevalence education employment and community living. AIHW, Canberra
Bajekal M, Harries T, Breman R, Woodfield K (2004) Review of disability estimates and definitions. National Centre for Social Research, London
Bethune-Davies P, McWilliam C, Bermen H (2006) Living with the health and social inequities of a disability: a critical feminist study. Health Care Women Int 27:204–222
Burchardt T, Le Grand J, Piachaud D (2002) Degrees of exclusion: developing a dynamic, multidimensional measure. In: Hills J, Le Grand J, Piachaud D (eds) Understanding social exclusion. Oxford University Press, Oxford, pp 30–43
Butterworth P, Crosier T (2004) The validity of the SF-36 in an Australian national household survey: demonstrating the applicability of the Household Income and Labour Dynamics in Australia (HILDA) Survey to examination of health inequalities. BMC Public Health, pp 1–11
Cepeda ML, Allen FH, Cepeda NJ, Yang Y-M (2000) Physical growth, sexual maturation, body image and sickle cell disease. J Natl Med Assoc 92:10–14
Claussen B (1999) Alcohol disorders and re-employment in a 5-year follow-up of long-term unemployed. Addiction 94:133–138
Committee on Children with Disabilities and Committee on Psychosocial Aspects of Child and Family Health (1993) Psychosocial risks of chronic health conditions in childhood and adolescence. Pediatrics 92:876–877
Connell RW (1995) Masculinities. Allen and Unwin, Sydney
Crosier T, Butterworth P, Rodgers B (2007) Mental health problems among single and partnered mothers: the role of financial hardship and social support. Social Psychiatry Psychiatr Epidemiol 42:6–13
Einfeld SL, Piccinin AM, Mackinnon A et al (2006) Psychopathology in young people with intellectual disability. JAMA 296:1981–1989
Emerson E, Hatton C (2007) The contribution of socio-economic position to the health inequalities faced by children and adolescents with intellectual disabilities in Britain. Am J Ment Retard 112:140–150
Emerson E, Hatton C (2007) Mental health of children and adolescents with intellectual disabilities in Britain. Br J Psychiatry 191:493–499
Emerson E, Honey A, Madden R, Llewellyn G (2009) The well-being of Australian adolescents and young adults with self-reported long-term health conditions, impairments or disabilities: 2001 and 2006. Aust J Soc Issues 44:39–53
Fagg J, Curtis S, Stansfeld SA, Congdon P (2006) Psychological distress among adolescents, and its relationship to individual, family and area characteristics in East London. Soc Sci Med 63:636–648
Fone D, Dunstan F, Williams G, Lloyd K, Palmer S (2007) Places, people and mental health: a multilevel analysis of economic inactivity. Soc Sci Med 64:633–645
Fuhrer R, Stansfeld SA, Chemali J, Shipley MJ (1999) Gender, social relations and mental health: prospective findings from an occupational cohort (Whitehall II study). Soc Sci Med 48:77–87
Gallo LC, Matthews KA (2003) Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull 129:10–51
Gannon B, Nolan B (2006) The dynamics of disability and social inclusion in Ireland. The Economic and Social Research Institute, Dublin
Gannon B, Nolan B (2007) The impact of disability transitions on social inclusion. Soc Sci Med 64:1425–1437
Goggin G, Newell C (2005) Disability in Australia: exposing a social apartheid. UNSW Press, Sydney
Gortmaker SL, Perrin JM, Weitzman M, Homer CJ, Sobol AM (1993) An unexpected success story: transition to adulthood in youth with chronic physical health conditions. J Res Adolesc 3:317–336
Gray KM, Mohr C (2004) Mental health problems in children and adolescents with intellectual disability. Curr Opin Psychiatry 17:365–370
Headey B, Warren D (2008) Families, incomes and jobs, volume 3: a statistical report on waves 1 to 5 of the HILDA survey. Melbourne Institute of Applied Economic and Social Research, Melbourne
Henderson S, Duncan-Jones P, McAuley H, Ritchie K (1978) The patient’s primary group. Br J Psychiatry 132:74–86
HILDA (2006) HILDA survey annual report 2006. Melbourne Institute of Applied Economic and Social Research, University of Melbourne, Melbourne
Jenkins S, Rigg J (2004) Disability and disadvantage: selection, onset and duration effects. J Soc Policy 33:479–501
Kerr DC, Preuss LJ, King CA (2006) Suicidal adolescents’ social support from family and peers: gender-specific associations with psychopathology. J Abnorm Child Psychol 34:103–114
Klineberg E, Clark C, Bhui KS, Haines MM, Viner RM, Head J et al (2006) Social support, ethnicity and mental health in adolescents. Soc Psychiatry Psychiatr Epidemiol 41:755–760
Kolaitis G (2008) Young people with intellectual disabilities and mental health needs. Curr Opin Psychiatry 21:469–473
Kuh D, Power C, Blane D, Bartley M (2004) Socioeconomic pathways between childhood and adult health. In: Kuh D, Ben-Shlomo Y (eds) A life course approach to chronic disease epidemiology. Oxford University Press, Oxford, pp 371–398
Luthar SS (2003) Resilience and vulnerability: adaptation in the context of childhood adversities. Cambridge University Press, Cambridge
Marmot M, Wilkinson RG (eds) (2006) Social determinants of health, 2nd edn. Oxford University Press, Oxford
Marshall ML, Barnett RC (1993) Work family strains and gains among two-earner couples. J Community Psychol 21:64–78
McClish D, Penberthy L, Bovbjerg V, Roberts J, Aisiku I, Levenson J, Roseff S, Smith W (2005) Health related quality of life in sickle cell patients: the PiSCES project. Health Qual Life Outcomes 3:50
Miauton L, Narring F, Michaud PA (2003) Chronic illness, life style and emotional health in adolescence: results of a cross-sectional survey on the health of 15–20-year-olds in Switzerland. Eur J Pediatr 162:682–689
Mont D (2007) Measuring disability prevalence. Social protection discussion papers. World Bank, Washington
Morrell S, Taylor R, Quine S, Kerr C, Western J (1994) A cohort study of unemployment as a cause of psychological disturbance in Australian youth. Soc Sci Med 38:1553–1564
Neumark-Sztainer D, Story M, Resnick MD, Garwick A, Blum RW (1995) Body dissatisfaction and unhealthy weight-control practices among adolescents with and without chronic illness: a population-based study. Arch Pediatr Adolesc Med 149:1330–1335
Patterson J, Blum RW (1996) Risk and resilience among children and youth with disabilities. Arch Pediatr Adolesc Med 150:692–698
Perrin JM (2002) Health services research for children with disabilities. Milbank Q 80:303–324
Perry MJ (1996) The relationship between social class and mental disorder. J Prim Prev 17:17–30
Pickett KE, Wilkinson RG (2007) Child wellbeing and income inequality in rich societies: ecological cross sectional study. BMJ 335:1080–1086
Sanson-Fisher RW, Perkins JJ (1998) Adaptation and validation of the SF-36 Health Survey for use in Australia. J Clin Epidemiol 51:961–967
Saunders P (2006) The costs of disability and the incidence of poverty. Social Policy Research Centre, University of NSW, Sydney
Sawyer MG, Arney FM, Baghurst PA, Clark JJ, Graetz BW, Kosky RJ, Nurcombe B, Patton GC, Prior MR, Raphael B, Rey J, Whaites LC, Zubrick SR (2000) Mental health of young people in Australia: child and adolescent component of the National Survey of Mental Health and Well-being. Commonwealth Department of Health and Aged Care, Canberra
Sawyer SM, Drew S, Yeo MS, Britto MT (2007) Adolescents with a chronic condition: challenges living, challenges treating. Lancet 369:1481–1489
Seigel W, Golden N, Gough J, Lashley M, Sacker I (1990) Depression, self-esteem, and life events in adolescents with chronic illness. J Adolesc Health Care 11:501–504
Smith DM, Langa KM, Kabeto MU, Ubel PA (2005) Health, wealth, and happiness: financial resources buffer subjective well-being after the onset of a disability. Psychol Sci 16:663–666
Stam H, Hartman EE, Deurloo JA, Groothoff J, Grootenhuis MA (2006) Young adult patients with a history of pediatric disease: impact on course of life and transition into adulthood. J Adolesc Health 39:4–13
Stewart D, Antle BJ, Healy H, Law M, Young NL (2007) Best practice guidelines for transition to adulthood for youth with disabilities in Ontario: an evidence-based approach. CanChild Centre for Childhood Disability Research, Ontario
Varni J, Limbers C, Burwinkle T (2007) Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL™ 4.0 Generic Core Scales. Health Qual Life Outcomes 5:43
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36) I. Conceptual framework and item selection. Med Care 30:473–483
Ware JE, Snow KK, Kosinski M, Gandek B (2000) SF-36 Health Survey: manual and interpretation guide. QualityMetric Inc., Lincoln
Watson N (ed) (2008) HILDA user manual: Release 6. Melbourne Institute of Applied Economic and Social Research, University of Melbourne, Melbourne
Watson N, Wooden M (2002) The Household, Income and Labour Dynamics in Australia (HILDA) survey: wave 1 survey methodology. HILDA project technical paper series. University of Melbourne, Melbourne
Wight RG, Botticello AL, Aneshensel CS (2006) Socioeconomic context, social support, and adolescent mental health: a multilevel investigation. J Youth Adolesc 35:115–126
Wilkinson RG (2005) The impact of inequality. The New Press, New York
Wolman C, Resnick MD, Harris LJ, Blum RW (1994) Emotional well-being among adolescents with and without chronic conditions. J Adolesc Health 15:199–204
World Health Organisation (2008) Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. World Health Organization, Geneva
Acknowledgments
This research was the outcome of the collaboration “Achieving Better Health Outcomes for Youth with Chronic Health Conditions: A Pan Disciplinary Approach”. The collaboration was seed-funded by the Australian Research Alliance for Children and Youth, whose support we greatly appreciate. We would also like to thank the other collaborators for their participation and contributions. This paper uses unit record data from the Household, Income and Labour Dynamics in Australia (HILDA) Survey. The HILDA Project was initiated and is funded by the Australian Government Department of Families, Housing, Community Services and Indigenous Affairs (FaHCSIA) and is managed by the Melbourne Institute of Applied Economic and Social Research (Melbourne Institute). The findings and views reported in this paper, however, are those of the author and should not be attributed to either FaHCSIA or the Melbourne Institute.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Honey, A., Emerson, E. & Llewellyn, G. The mental health of young people with disabilities: impact of social conditions. Soc Psychiat Epidemiol 46, 1–10 (2011). https://doi.org/10.1007/s00127-009-0161-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-009-0161-y




 ) Disability: low social support, (
) Disability: low social support, ( ) disability: high social support, (
) disability: high social support, ( ) no disability: low social support, (
) no disability: low social support, ( ) no disability: high social support
) no disability: high social support

