Abstract
Background
Both individual and familial histories of mental illness are substantial risk factors for suicide in young people.
Aim
To explore suicide risk among adolescents and young adults according to detailed aspects of individual and parental psychiatric admission history.
Methods
A nested case–control study was undertaken using data from Danish population registers to include 4,142 suicide cases and 82,840 matched controls aged 9–35 years. Data were analyzed with conditional logistic regression.
Results
A history of hospitalized psychiatric illness was a strong risk factor for suicide in adolescents and young adults, and the effect of such a history was greater in females than males. The elevated risk peaked in the two periods immediately after admission and discharge for both sexes, and exceeded in females who had multiple admissions and in males who were diagnosed with schizophrenia, affective disorders or substance abuse disorders. At the same time, a parental psychiatric history constituted a substantial risk factor for suicide in young people, in particular, if having a mother admitted for psychiatric illness. The elevated risk associated with parental psychiatric history was greater in females than in males, and tended to be more prominent during the first few years after admission of a parent.
Conclusion
Prevention strategies should aim at improving treatment and care to young people with psychiatric problems and at providing social support and psychological consultation to children with parental psychiatric illness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous studies have consistently documented that both personal and familial psychiatric history are important risk factors for completed suicide among young people [2, 3, 10, 15, 17]. The increased risk associated with a personal history of psychiatry often peaks immediately after a psychiatric admission, and to some extent varies by diagnosis and severity of illness. However, few studies have been able to explore this association in detail by taking into account these aspects simultaneously to examine their relative importance [13, 20]. At the same time, a parental history of psychiatric illness could increase risk for suicide among young offspring either through genetic transmission of vulnerability associated with psychiatric illness, or through its negative influence on family life, e.g., reduced care to the children. Further investigation, addressing the relative influence of maternal and paternal psychiatric history, diagnosis, time since the first contact, etc., in the context of personal own psychiatric status may be able to provide a close clue to this relationship. In the present study based on the entire Danish adolescent and young adult population, we aimed to answer the above mentioned questions to broaden the understanding and comprehension of the association between individual and familial psychiatric history and the risk of suicide among adolescents and young adults.
Materials and methods
Data sources
We obtained data for this study from four national population registers in Denmark. The first was the Danish Civil Register which contains a personal identification number for each individual residing in Denmark as well as links to mother and father at time of birth [14]. This personal identification number is used in all national registers and can be used as a key to retrieve and merge personal data from various registers and to identify links to parents. However, due to the regulations when the civil registration was established in 1968, a certain proportion of people residing in Denmark do not have links to their parents if (1) a person was not living with a parent in 1969, (2) a person itself was a parent in 1969, (3) the parent emigrated from Denmark before 1979 or (4) the person immigrated to Denmark as an adult. These selection mechanisms mean that links to at least a mother is available for almost everybody born in Denmark in 1960 or later, gradually decreasing backwards with birth year. The second register was the Cause-of-Death Register [9], which includes information on cause and date of all deaths in Denmark since 1967. Death of completed suicide was coded as E950–E959 according to the International Classification of diseases eighth revision until 1994, and X60–X84 according to the tenth revision thereafter. The third register was the Danish Psychiatric Central Register which records all dates of admission and discharge as well as diagnoses for all psychiatric inpatients since 1969 [12]. In Denmark hospital treatment is free of charge and there are no private psychiatric hospitals. The last register is the Integrated Database for Labour Market Research (IDA) [5], which contains longitudinal data from 1980 and onwards on socioeconomic and labour market conditions for the entire Danish population. Personal data of a calendar year is complete only for persons who are residing in Denmark on 31 December of the calendar year.
Study design and participants
We adopted a nested case–control design [4] to create a study data set based upon the entire national population in Denmark. At first we obtained all completed suicide victims from 1981 to 1997 from the Cause-of-Death Register, then restricted study cases to persons who were under 35 years old and living in Denmark on 31 December the year prior to the year of suicide. This resulted in the identification of 3,140 male and 1,002 female cases aged 9–35 years. Using a representative sample of the Danish population in the IDA-database, each suicide case was matched with 20 population controls who were identical in terms of age and sex and were alive on the date of case suicide. With this procedure, a total of 62,800 male and 20,040 female controls, matched for 3,140 male and 1,002 female suicide cases, were enrolled into the study.
Variables
Based on data from source registers, we added explanatory variables containing information on cases, controls, and their parents. From the Danish Psychiatric Central Register, we recorded personal data on three aspects of the person’s and the parents’ psychiatric history. The first variable was time since admission to or discharge from a psychiatric hospital in detailed categories according to time elapsed from a psychiatric hospitalization. We chose to use the information of the latest hospitalization for cases and controls and the first hospitalization for parents. The second explanatory variable was the total number of psychiatric admissions for study subjects and parents. The third variable was the person’s main diagnosis at the latest hospitalization and parent’s main diagnosis at the first hospitalization. We categorized the diagnoses into four major groups; schizophrenia spectrum disorder (ICD-8 codes 295, 297, 298.29, 298.39, 298.89, 298.99, 299.05, 299.09, 301.09, 301.29 and 301.83 and ICD-10 codes F20, F21, F23, F24, F25, F28, F29, F60.0 and F60.1), affective disorders (ICD-8 codes 296, 298.09, 298.19, 300.49 and 301.19 and ICD-10 codes F30, F31, F32, F33, F34, F38 and F39), substance abuse disorders (ICD-8 codes 303 and 304 and ICD-10 codes F10.2, F10.3, F10.4 and Flx.2) and other psychiatric disorders. For the purpose of adjustment, variables identifying the socio-economic status the year prior to the year of suicide were extracted from the IDA database, i.e., person’s marital status, income and place of residence. Since some cases did not have a link to a father or mother, we also included a variable indicating the availability of links to parents in the analyses.
Statistical analysis
We constructed contingency tables for the main study variables and computed the conditional odds ratios (and 95% confidence intervals) of suicide using conditional logistic regression with the PhReg procedure available in SAS version 8 [8]. Because we sampled controls from individuals at risk for suicide at the time, i.e., risk set sampling, the estimated odds ratios in this study can be interpreted as risk ratios. We additionally examined interactions between study variables using the likelihood test.
Results
The cases of this study included 3,140 males aged 9–35 years and 1,002 females aged 14–35 years who committed suicide in Denmark during the period 1981 to 1997. Among these cases, 1,214 (38.7%) males and 572 (57.1%) females had a history of hospitalized psychiatric illness, with schizophrenia being the most common psychiatric diagnosis. At the same time, 514 (16.4%) males and 177 (17.7%) females had at least one parent with a history of admission to a psychiatric hospital, while 47 males and 19 females even had both parents with such a history.
Suicide and individual’s own psychiatric history
Our analyses indicated that a personal history of psychiatric hospitalization was a strong risk factor for completed suicide in adolescents and young adults in Denmark (Table 1). Its strong effect remained after controlling for personal socioeconomic status [adjusted odds ratio: 13.5 (12.2–15.0) for males and 38.9 (32.2–47.1) for females], and the increased risk associated with such a history was significantly greater for females than for males (sex interaction test: χ2 = 111.2, P-value < 0.0001).
When exploring this association in details (Table 1), we noted that, for both males and females, the risk for suicide peaked immediately after admission to or discharge from a psychiatric hospital, and then gradually decreased with the time thereafter, and that the risk increased progressively with numbers of psychiatric admissions. Compared with other disorders, the increased risk was significantly higher if diagnosed with schizophrenia spectrum disorders, affective disorders or substance abuse disorders in both sexes, and with personality or adjustment disorders in males.
When including these variables into the model simultaneously and adjusting the data for personal marital status, income, place of residence as well as parental psychiatric history, the estimated risks associated with personal psychiatric factors were either reduced or eliminated due to strong interactions between these variables. Still, the two sharp peaks of high suicide risk in the periods right after admission and discharge remained prominent in both sexes. At the same time, the excess risk associated with multiple admissions remained significant only in females, while the substantial risk associated with affective disorders, substance abuse disorders remained significantly high only in male subjects.
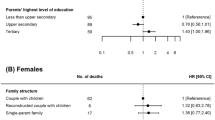
Suicide and parental psychiatric history
This study demonstrated that having a parent with a history of admission to a psychiatric hospital was a strong predictor for suicide in offspring adolescents and young adults (Table 1). Although our analyses suggested a significant interaction between individual psychiatric history and parental psychiatric history (χ2 = 31.5, P < 0.001), the increased risk associated with psychiatric history of a mother [adjusted odds ratio: 1.5 (1.3–1.8) for males and 1.8 (1.4–2.4) for females] or a father [adjusted odds ratio: 1.2 (1.0–1.4) for males and 1.4 (1.0–2.0) for females] remained highly significant after adjusting for case’s socioeconomic status and own psychiatric history. At the same time, the effect of parental psychiatric history was slightly stronger in female offspring than in male offspring (sex interaction test of overall influence of parental psychiatric history: χ2 = 6.7, P = 0.035).
Including detailed information regarding parent’s psychiatric contact, i.e., time elapsed from the first admission, diagnosis of disorders and number of total admissions into the analyses, the results (Table 2) showed that, for both sexes, the increased risk appeared more pronounced the shorter the time between parent’s first psychiatric admission and the case suicide, and it existed continuously even after a parent had had a such history for more than 10 years. At the same time, multiple psychiatric admissions of a father and/or a mother substantially increased the risk for suicide in both female and male offspring. In terms of psychiatric diagnosis in parents, schizophrenia tended to have an additional effect, however, the excess risk was statistically significant only for female offspring having a mother diagnosed with schizophrenia.
These estimates changed substantially after further adjustment for person’s own socioeconomic status and psychiatric history. Thus, for both sexes, the increased risk for suicide remained significant only if a mother was admitted for the first time to a psychiatric hospital within the past 3 years; additionally for female offspring this elevated risk of suicide continued until 4–10 years after the first psychiatric admission of a mother. At the same time, the elevated risks associated with paternal psychiatric discharge, multiple admissions, and psychiatric diagnosis, were rendered non-significant in either sex.
When introducing a variable that combined psychiatric history of both father and mother into the model, the results showed that the risk of suicide was elevated if the father had been admitted to a psychiatric hospital [odds ratio: 1.7 (CI 1.4–2.0) for males and 2.1 (CI 1.5–2.8) for females], and increased additionally if the mother had been admitted [odds ratio: 2.3 (CI 2.0–2.6) for males and 3.0 (CI 2.4–3.7) for females], and peaked if both parents had been admitted [odds ratio: 3.1 (CI 2.3–4.2) for males and 3.9 (CI 2.4–6.4) for females]. After adjustment for person’s socioeconomic status and psychiatric history, these estimates were slightly attenuated but generally resembled the pattern of the crude analyses.
Discussion
This comprehensive study based on data from Danish longitudinal registers demonstrates that a history of hospitalized psychiatric illness was a strong risk factor for suicide in adolescents and young adults, and the effect of such a history was greater in females than males. The elevated risk peaked in the two periods immediately after admission and discharge for both sexes, and exceeded for females who had multiple admission and for males who were diagnosed with schizophrenia, affective disorders or substance abuse disorders. The study also shows that a parental psychiatric history constituted a substantial risk factor for suicide in young people, in particular, if having a mother admitted for psychiatric illness. The elevated risk associated with parental psychiatric history was greater in female subjects than males, and it tended to be more prominent during the first a few years after admission of a parent.
The primary strengths of our study are the use of population controls, inclusion of socioeconomic data, and risk set samples with an unbiased estimate of the incidence rate ratio in a cohort design. At the same time, all residents in Denmark have equal access to psychiatric hospitals with treatment free of charge. The decision on hospitalization of a patient is completely based upon the psychiatric evaluation from psychiatrists. Individual data on each admission have been recorded and computerized in the Danish Psychiatric Central Register since 1969 and are not targeted for any specific research purpose. These advantages enable us to obtain precise and cumulative information about individual history of psychiatric hospitalisation, and our data are not subject to differences in access to psychiatric care by socioeconomic status. On the other hand, we are not able to control the influence of psychiatric illness not leading to hospitalization because such data were not available in the register before the year 1995. Also, our data may represent a severe spectrum of psychiatric disorders that require hospital treatment. In addition, the coverage period of our data back to 1969 might not be long enough to catch the lifetime history of psychiatry; however, this limitation may apply to the history of the parents only since our study cases are young of age. Nevertheless, we believe, this large population-based study provides substantial knowledge about suicide risk in relation to personal and familial history of psychiatry, which may assist health professionals making strategies to reduce suicides in this high-risk population.
This study confirms the finding in the literature that a psychiatric history is a significant risk factor for suicide among adolescents and young people [1–3, 10, 15, 17], but provides further insights that the risk peaks at time periods shortly after admission and discharge, and that the risk exceeds for individuals with multiple admissions or with a diagnosis of schizophrenia, affective disorders or substance abuse disorders. The test for sex interaction moreover documents that a psychiatric history has a significantly stronger impact on increasing risk for suicide among females than does it among males. These findings highlight the importance of special care and social attention towards young people with psychiatric illness, especially female patients and in the specific time-periods immediately after admission or discharge.
Our observation that as many as 57.1% young females and 38.7% young males who killed themselves had actually been admitted to a psychiatric hospital for treatment is remarkable. These numbers would be much higher if including individuals who had contacted psychologists, general practitioners or psychiatric wards for outpatients because of psychiatric problems. Such information does not only indicate how vulnerable young people with psychiatric problems are to suicide, but also suggests important possibilities to prevent tragedies if psychiatrists, psychologists and GPs are well-trained for suicide prevention.
Moreover, in line with the literature documenting a familial psychiatric history as a risk factor for suicide in young people [2, 15], this study pinpoints that a parental, especially a maternal, psychiatric history significantly increases the risk of suicide in offspring even after controlling for own psychiatric history and socioeconomic status, and that the increased risk is slightly greater in female than male offspring. At the same time, this study, to our awareness, is the first that has taken variables of time since parental first psychiatric admission, diagnosis of the admission and the total number of admission into account simultaneously to estimate their relative importance.
Our finding that 16.4% male and 17.7% female cases had a parental psychiatric history is likely an underestimation because since it was only possible to include information recorded after the year 1968 on parents with psychiatric illness that led to hospitalization, and we were unable to get parental information for individuals whose links to parents were not recorded in the register. This may explain why our number is lower than the numbers collected through psychological autopsy in other studies [7, 11, 13, 15].
Our results establish that the more recent the first psychiatric admission of a parent the higher risk of suicide would be, suggesting that the influence of parental psychiatric history on young offspring suicide is likely on an emotional level rather than a genetic level. This is further supported by our finding that maternal psychiatric history denoted a more substantial risk factor for suicide than paternal psychiatric history, because the mother usually represents the primary carer within a family, so if the mother was mentally ill, it might affect the nursing of the children more than if the father was mentally ill. This explanation is moreover supported by the fact that the subjects in this study are young and subsequently have a relatively strong attachment to and need for their parents. In line herewith, few studies have demonstrated that inadequate parental care, low parental involvement and low emotional support from the parents can act as risk factors for suicide in young people [6, 18]. Although genetic components may play a role [16, 19], we believe, the association between risk of suicide and psychiatric history of a parent, especially maternal psychiatric history, to a large extent is attributed to by a decrease in parental care, both mentally and physically.
We believe that this large population-based study sheds new light on how individual and familial psychiatric histories influence suicide risk in adolescents and young adults and hence has some important clinical implications. Previous studies have emphasised the importance of targeting prevention strategies at mentally ill people as early as possible. The results of this study vindicate that strategy, and in addition the results also highlight the importance of offering psychological counselling to families with parental mental illness. The counselling could be in the form of providing the family with coping strategies in order to prevent later psychological repercussions such as feelings of neglect in the children, and to deal with stress naturally occurring in such situations.
References
Agerbo E, Nordentoft M, Mortensen PB (2002) Familial, psychiatric, and socioeconomic risk factors for suicide in young people: nested case–control study. BMJ 325(7355):74
Beautrais AL (2003) Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am J Psychiatry 160(6):1093–1099
Brent DA (1995) Risk factors for adolescent suicide and suicidal behavior: mental and substance abuse disorders, family environmental factors, and life stress. Suicide Life Threat Behav 25(suppl 52–63):52–63
Clayton D, Hills M (1993) Statistical models in epidemiology. Oxford University Press, Oxford
Danmarks S (1991) IDA—en integreret database for arbejdsmarkedsforskning. Danmarks Statistiks trykkeri, København
Flouri E (2005) Psychological and sociological aspects of parenting and their relation to suicidal behavior. Arch Suicide Res 9(4):373–383
Houston K, Hawton K, Shepperd R (2001) Suicide in young people aged 15–24: a psychological autopsy study. J Affect Disord 63(1–3):159–170
SAS Institute Inc. (1999) The PHREG Procedure. SAS/STAT user’s guide, version 8. SAS Institute Inc., Cary, pp 2569–2657
Juel K, Helweg-Larsen K (1999) The Danish registers of causes of death. Dan Med Bull 46(4):354–357
Koplin B, Agathen J (2002) Suicidality in children and adolescents: a review. Curr Opin Pediatr 14(6):713–717
Mittendorfer-Rutz E, Rasmussen F, Wasserman D (2008) Familial clustering of suicidal behaviour and psychopathology in young suicide attempters. A register-based nested case control study. Soc Psychiatry Psychiatr Epidemiol 43(1):28–36
Munk-Jorgensen P, Mortensen PB (1997) The Danish psychiatric central register. Dan Med Bull 44(1):82–84
Murphy GE (1998) Why women are less likely than men to commit suicide. Compr Psychiatry 39(4):165–175
Pedersen CB, Gotzsche H, Moller JO, Mortensen PB (2006) The Danish Civil Registration System. A cohort of eight million persons. Dan Med Bull 53(4):441–449
Portzky G, Audenaert K, van Heeringen K (2005) Suicide among adolescents. A psychological autopsy study of psychiatric, psychosocial and personality-related risk factors. Soc Psychiatry Psychiatr Epidemiol 40(11):922–930
Qin P (2003) The relationship of suicide risk to family history of suicide and psychiatric disorders. Psychiatr Times 20(13):62–63
Qin P, Agerbo E, Mortensen PB (2002) Suicide risk in relation to family history of completed suicide and psychiatric disorders: a nested case–control study based on longitudinal registers. Lancet 360(9340):1126–1130
Reigstad B, Jorgensen K, Sund AM, Wichstrom L (2006) Adolescents referred to specialty mental health care from local services and adolescents who remain in local treatment: what differs? Soc Psychiatry Psychiatr Epidemiol 41(4):323–331
Roy A, Nielsen D, Rylander G, Sarchiapone M (2000) The genetics of suicidual behaviour. In: Hawton K, van Heeringen K (eds) The international handbook of suicide and attempted suicide. Wiley, Chichester, pp 209–221
Shiang J (1998) Does culture make a difference? Racial/ethnic patterns of completed suicide in San Francisco, CA 1987–1996 and clinical applications (in process citation). Suicide Life Threat Behav 28(4):338–354
Acknowledgments
This study was initiated during Miss Kirstina Stenager’s internship. Miss Stenager participated in study design, data analysis and interpretation, and prepared the first draft of the manuscript. Associate Professor Ping Qin supervised the study, made the final analysis of the data and finalized the manuscript. The authors thank Preben Bo Mortensen for his support.
Financial disclosure and conflict of interest.
There is no conflict of interest for this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stenager, K., Qin, P. Individual and parental psychiatric history and risk for suicide among adolescents and young adults in Denmark. Soc Psychiat Epidemiol 43, 920–926 (2008). https://doi.org/10.1007/s00127-008-0385-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0385-2