Abstract
The cannabinoid receptors, CB1 and CB2, are expressed in the heart, but their role under pathological conditions remains controversial. This study examined the effect of CB1 receptor blockade on cardiovascular functions after experimental MI and in experimental metabolic syndrome. MI was induced in Wistar rats by permanent ligation of the left coronary artery. Treatment with the CB1 receptor antagonist rimonabant (10 mg/kg i.p. daily) started 7 days before or 6 h after MI and continued for 6 weeks. Haemodynamic parameters were measured via echocardiography and intracardiac Samba catheter. CB1 blockade improved systolic and diastolic heart function, decreased cardiac collagen and hydroxyproline content and down-regulated TGF-β1. Additionally, rimonabant decreased arterial stiffness, normalised QRS complex duration and reduced brain natriuretic peptide levels in serum. In primary cardiac fibroblasts, rimonabant decreased MMP-9 activity and TGF-β1 expression. Furthermore, rimonabant improved depressed systolic function of spontaneously hypertensive obese rats and reduced weight gain. Blocking of CB1 receptor with rimonabant improves cardiac functions in the early and late stages after MI, decreases arterial stiffness and reduces cardiac remodelling. Rimonabant also has cardioprotective actions in rats characterised by the metabolic syndrome. Inhibition of proteolysis and TGF-β1 expression and reduced collagen content by rimonabant may attenuate destruction of the extracellular matrix and decrease fibrosis after MI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocardial infarction (MI) and heart failure (HF) are among the leading causes of hospitalisation, morbidity and mortality worldwide. Although advances in the therapy improved survival rate after acute coronary ischaemia, the number of patients diagnosed with HF increased during the last decade [1]. Therefore, there is a compelling need to develop novel strategies for the prevention and treatment of coronary heart disease.
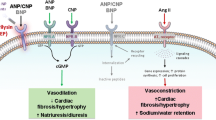
The endocannabinoid system comprises the endocannabinoids (arachidonoylethanolamide and 2-arachidonoylglycerol), two cannabinoid receptors (CB1 and CB2) and the enzymes involved in endocannabinoid synthesis and degradation [2, 3]. In addition to its actions in the control of the central nervous system, the endocannabinoid system may play a pivotal role in cardiovascular regulation [4] and has been linked to obesity and cardiometabolic risk [5].
CB1 and CB2 receptors are seven-transmembrane Gi/o-coupled receptors. By coupling to Gi/o proteins, CB1 receptor regulates the activity of various membrane proteins and signal transduction pathways including ion channels [2].
The mechanisms of the cardiovascular effects of cannabinoids are complex and may involve modulation of autonomic outflow in the central and peripheral nervous systems as well as direct effects on the myocardium and vasculature. It has been confirmed that both endocannabinoids and their receptors are present in the heart [6, 7] and vessels [8, 9]. Signalling through the CB1 receptor elicits hypotension, bradycardia and negative inotropy, whereas CB2 receptor activation exerts positive inotropic effects on the heart [4, 10].
The role of the cannabinoid receptors in the heart under pathological conditions remains controversial. In some experimental models, such as acute ischaemia/reperfusion injury [11] and doxorubicin-induced cardiotoxicity [12], the CB1 receptor blockade with rimonabant has been demonstrated to be cardioprotective. On the other hand, the CB1 receptor antagonist AM-251 promoted left ventricular (LV) remodelling and dilatation after cardiac ischaemia [13].
The selective CB1 receptor antagonist rimonabant, which has been proposed for the treatment of obesity, has also been shown to improve cardiovascular risk factors including serum lipid profiles and to increase circulating levels of adiponectin [5, 14, 15]. Rimonabant also improved vascular function in a mouse atherosclerotic model [16]. No study so far investigated the effect of chronic, long-term CB1 receptor blockade with rimonabant on cardiac function after MI.
In the present study, we investigated whether chronic CB1 receptor inhibition with rimonabant exerts cardioprotective effects in rats with metabolic syndrome. We also hypothesised that CB1 receptor antagonism might produce beneficial effects independent from metabolic changes and investigated its cardiovascular effects in acute (7 days) and chronic (6 weeks) models of myocardial ischaemia. In addition, we studied the potential underlying mechanisms of rimonabant action on the heart by exploring the remodelling processes of post-ischaemic myocardium.
Material and methods
Ethics statement
All animal experiments were conducted with approval by the ethics commission of the regulatory authorities of the city of Berlin, Germany, the “Landesamt für Gesundheit und Soziales” (registration number G 0307/06) and complied with national and European guidelines for animal experiments (EU RL 2010/63/EU).
Animals
Male normotensive Wistar rats (6 weeks old; weight, 200 to 220 g; Harlan Winkelmann, Borchen, Germany) and male obese spontaneously hypertensive Koletsky rats (SHROB; weight, 300 to 320 g; Charles River Laboratories, Sulzfeld, Germany) were kept in a specific pathogen-free barrier under standardised conditions with respect to temperature and humidity and were housed on a 12-h light/12-h dark cycle in groups of five animals with food and water ad libitum.
Experimental protocol
Male Wistar rats were randomly assigned to the following groups: rimonabant pre-treatment—treatment started 7 days before MI and was continued until end of the protocol; rimonabant treatment—treatment started 3 h after MI induction and continued until end of the protocol; and two vehicle groups accordingly.
MI was induced in Wistar rats as previously established [17]. Briefly, under anaesthesia with ketamine/xylazine (80/10 mg/kg i.p.) and intubation, a left lateral thoracotomy was performed and a suture was tightened around the proximal left anterior descending coronary artery. Sham-operated rats underwent the same surgical procedure with the exception of coronary ligature. Assignment of animals to the respective treatment groups was performed by an investigator who was strictly blinded to the outcome of MI operation. Thorough inclusion and exclusion criteria, based on functional evaluation 24 h after MI, were applied to clearly narrow groups with equal infarct size for further intervention and monitoring. Animals with severe impairment of ejection fraction (EF ≤ 35 %) were excluded (vehicle group: one animal in each 1- and 6-week study; rimonabant pre-treatment and treatment groups 6-week study: one and three animals, respectively). Additionally, animals with EF > 73 % after MI were also excluded. Together in the 1- and 6-week studies, seven animals from the vehicle group and four animals in each rimonabant pre-treatment and treatment group were excluded. The final number of animals per group was 7–12 at the time of euthanasia.
Rimonabant (Sanofi Aventis GmbH, Frankfurt, Germany) was administered 10 mg/kg/day i.p., a dose which was assessed in preliminary experiments (treatment with rimonabant in a dose of 10 mg/kg/day i.p., but not 3 mg/kg/day for 14 days lead to significant weight loss in SHROB rats and improved systolic cardiac function).
Additionally, the acute effect of rimonabant (10 mg/kg, in 0.5 ml NaCl, i.a. in the arteria femoralis) on LV pressure was examined in sham-operated and vehicle-treated animals with MI under 1.5–2 % isoflurane.
To investigate the effect of CB1 receptor blockade on cardiac function in the rats with metabolic syndrome, spontaneously hypertensive obese rats (SHROB, Koletsky rats) were treated with rimonabant or vehicle for 2 weeks (10 mg/kg/day, i.p.). Cardiac function was evaluated using echocardiography. Lean age-matched Wistar rats were used as controls.
Locomotor activity
Animals were housed individually, and spontaneous movements were recorded by an infrared monitoring system (Supermex, Muromachi, Tokyo, Japan) before MI and 4 weeks after MI, over a 24-h period.
Transthoracic Doppler echocardiography
Transthoracic Doppler echocardiography (M-mode and Doppler measurements) was performed 1, 3 and 6 weeks after MI under 1.5–2 % isoflurane anaesthesia. Images were obtained by using a high-resolution imaging system Vevo 770 (VisualSonics Inc., Toronto, Canada).
Haemodynamic parameters
Haemodynamic assessment was performed at the end of the study, using a fibre-optic pressure transducer Samba catheter (Samba Sensors, Västra Frölunda, Sweden) and Chart 5 software for analysis. After anaesthesia with isoflurane (2 %), the catheter was inserted into the right carotid artery in the normal-breathing animal. After blood pressure (BP) recording in the ascending aorta, the catheter was advanced into the LV and the pressure time indices (dP/dt min and dP/dt max) were recorded.
Pulse wave analysis
Pulse wave analysis (PWA) was performed as shown in Supplemental Fig. 1. Diastolic pressure (Pd), pressure of the inflection point (Pi) and systolic pressure (Ps) were determined and averaged on the central aortic pressure waveforms from at least 20 cardiac cycles.
Electrocardiogram
A three-lead electrocardiogram (ECG; ADIstruments, Chart 5 software, Spechbach, Germany) was recorded in all animals at the end of the study under isoflurane (2 %) and analysed using the eMOUSE software (Mouse Specifics, Quincy, MA, USA). Duration of the QRS complex was analysed in at least four cardiac cycles.
Enzyme-linked immunosorbent assay
Brain natriuretic peptide (BNP) levels were determined in rat serum collected 6 weeks after MI using a commercially available enzyme-linked immunosorbent assay kit (Assaypro, St. Charles, MO, USA) according to the manufacturer’s protocol.
mRNA analysis
Total RNA from LV tissue was isolated by TRIzol reagent (Invitrogen). qRT-PCR was performed with MX3005p QPCR System (Stratagene) using SYBR green reaction mix and different primers (Supplemental material). All samples were measured in triplicate and expression values were normalised to 18S rRNA. Data analysis was done using the MxPro™ ET QPCR software (Stratagene) and ∆∆Ct method.
Western blotting
Protocols and antibodies are specified in the Supplementary material.
Histology
Paraffin-embedded heart samples were sectioned at 5 μm. Fibrosis was visualised by Sirius Red stain, according to standard protocols.
Hydroxyproline content in the heart and aorta
Amount of collagen in the thoracic aorta and cardiac septum was analysed by quantification of the tissue hydroxyproline content using the modified method based on alkaline hydrolysis as previously described [18].
Cell culture experiments
Primary rat cardiac fibroblasts were isolated as described previously [19]. Cells were cultured in Dulbecco’s modified Eagle’s medium containing sodium pyruvate, d-glucose (4.5 g/L) and 10 % foetal bovine serum and supplemented with 2 ng/ml IL-1β (Sigma) to induce the secretion of matrix metalloproteinases (MMPs). Incubation was preformed with or without co-incubation with rimonabant (1, 0.75, 0.5 and 0.25 μM). Activities of MMP-2 and MMP-9 were analysed with gelatine zymography as previously described [20].
Statistical analysis
Results were expressed as the mean ± SEM. Multiple comparisons were analysed with one-way analysis of variance (ANOVA) followed by the Bonferroni post hoc test. Two-group comparisons were analysed by the two-tailed Student unpaired t test for independent samples. Differences were considered statistically significant at the value of p < 0.05.
Results
CB1 receptor blockade improves cardiac function in rats with metabolic syndrome
To investigate the effect of CB1 receptor blockade on cardiac function in rats with metabolic syndrome, spontaneously hypertensive obese rats (SHROB, Koletsky rats) were treated with rimonabant or vehicle for 2 weeks. Age-matched lean Wistar rats served as controls. Vehicle-treated SHROB rats had depressed systolic LV function, as evidenced by reduced EF and fractional shortening (FS), compared with lean Wistar rats (p < 0.05) (Table 1). Rimonabant significantly reduced weight gain (p < 0.01) and improved systolic cardiac function in SHROB rats, raising FS and EF by 5.7 and 7.5 %, respectively, compared with the vehicle-treated group. Heart rate and BP were not influenced by rimonabant administration and changes in LV diameters between groups were not significant (Supplemental Table 1).
CB1 receptor blockade enhances heart inotropy
An acute effect of rimonabant administration (10 mg/kg, i.a.) on cardiac function was studied in Wistar rats 6 weeks post MI. As shown in Fig. 1a, maximal peak rate of developed LV pressure (dP/dt max) immediately increased after rimonabant injection and remained significantly higher 10 min after administration compared with vehicle. This response was constant over a 40-min period (not shown). Minimal peak rate of developed LV pressure (dP/dt min) decreased slightly (Fig. 1b). In sham rats, CB1 receptor blockade did not modify dP/dt max or dP/dt min (Fig. 1a, b).
Effect of intra-arterial rimonabant administration on a maximal peak rate of LV pressure and b minimal peak rate of LV pressure in sham rats (open circles) and 6 weeks after MI (solid circles). Injection of NaCl in the same volume served as a control (open upward triangles). c Representative LV pressure traces directly after NaCl/rimonabant administration. *p < 0.05 vs. basal value (time point 0); one-way ANOVA
Basal parameters 6 weeks after myocardial infarction
Mortality was only evident within the first 24 h after MI. The mortality rate was 32 %. Treatment with rimonabant did not influence this early mortality. Furthermore, no animal died during the further course of the study.
The dynamics of the most important physiological parameters which were studied 6 weeks after MI in Wistar rats are presented in Table 2. Significantly lower weight gain, decreased motility, increased heart and lung weight/body weight ratio were observed in the vehicle group compared to sham group. Rimonabant in the pre-treatment and post-treatment regimes significantly increased weight gain and motility of the animals as well as decreased serum levels of BNP compared with the vehicle group.
Additionally, rimonabant pre-treatment reduced heart weight to body weight ratio and prevented the occurrence of lung oedema. Moreover, rimonabant pre-treatment also normalised prolonged QRS complex duration, which was revealed by ECG in animals post MI.
Transthoracic Doppler echocardiography
The effect of CB1 receptor blockade on cardiac function was studied by transthoracic Doppler echocardiography at 7 days, 3 weeks and 6 weeks after ischaemia. A similar tendency among treatment regimens was observed at all measured time points. The outcomes obtained 7 days and 6 weeks after MI and representative echocardiographic images are presented in Fig. 2. MI induced a significant increase in end-systolic left ventricular (LVIDs) and end-diastolic left ventricular (LVIDd) diameters as well as a decrease in LV EF and FS. MI also impaired LV diastolic function, evidenced by an increased E/A ratio and shortened E-wave deceleration time (EDT). Seven days post MI, rimonabant pre-treatment reduced LVIDs from 5.6 ± 0.17 mm in vehicle to 4.8 ± 0.13 mm (p < 0.01). Rimonabant pre-treatment also reduced LVIDd from 8.2 ± 0.1 mm in vehicle to 7.6 ± 0.09 mm (p < 0.001), raising EF and FS by 6.4 % (p < 0.05) and 4.6 % (p < 0.05), respectively, compared to vehicle.
Haemodynamic variables measured by echocardiography 7 days (white bars) and 6 weeks (black bars) after MI; a diastolic LV internal diameter; b systolic LV internal diameter; c LV EF; d LV FS; e velocity ratio of the early filling wave to atrial contraction filling wave; f deceleration time of early filling wave (EDT); g representative M-mode echocardiograms obtained 6 weeks after MI. Rimonabant pre-treatment (Rim pre-tr.) prevented LV dilatation and improved motility of the LV anterior and posterior wall after MI. *p < 0.05, **p < 0.01 and ***p < 0.001 vs. sham 7 days; † p < 0.05, †† p < 0.01 and ††† p < 0.001 vs. vehicle 7 days; # p < 0.05, ## p < 0.01 and ### p < 0.001 vs. sham 6 weeks; § p < 0.05 and §§ p < 0.01 vs. vehicle 6 weeks; n = 7–12 per group
Six weeks post MI, rimonabant pre-treatment reduced LVIDs from 6.1 ± 0.13 mm in vehicle to 5.1 ± 0.23 mm (p < 0.01) and LVIDd from 8.7 ± 0.14 to 7.9 ± 0.2 mm (p < 0.05). EF and FS were increased after rimonabant pre-treatment by 10.0 % (p < 0.05) and 7.1 % (p < 0.05), respectively, compared to vehicle. Post-ischaemic treatment reduced LVIDd 7 days after MI (p < 0.01), but this effect was not significant 6 weeks after MI. Effect of treatment regimens on EF in individual animals during the course of the study are presented in Supplemental Fig. 2. In the pre-treatment group, EF was improved 7 days after MI compared to vehicle and preserved until 6 weeks after MI, whereas progressive deterioration of EF could be observed in the vehicle group.
Haemodynamic measurements
Haemodynamic parameters measured 6 weeks after MI using the Samba catheter are presented in Table 3. Heart rate and LV systolic and end-diastolic pressure did not differ among the groups. dP/dt max, contractility index and dP/dt min were significantly reduced 6 weeks after MI compared to sham-operated animals. Rimonabant in both treatment regimes significantly increased dP/dt max and dP/dt min, as well as prevented a decrease of contractility compared to vehicle. Aortic systolic and diastolic BP, which were slightly decreased post MI, were normalised after rimonabant treatment.
Arterial stiffness
To assess cardiac afterload, we measured indirect parameters of arterial stiffness by performing PWA on pressure curves obtained from the ascending aorta 7 days (data not shown) and 6 weeks after MI/sham operation. MI deteriorated PWA variables and led to progressive increase in augmentation pressure (AugP) which consequently increased the augmentation index (AIx) for 6.9 % 7 days post MI (not shown) and 12.6 % 6 weeks post MI, compared with the sham group (Fig. 3a, b). Rimonabant, both in pre-treatment and treatment regimen, significantly improved PWA variables. Favourable effect on AugP and AIx was observed 7 days post MI/sham, which was more pronounced 6 weeks post MI/sham (Fig. 3a, b). Pulse pressure and heart rate did not differ between the groups (Table 3). dP/dt max showed a significant and inverse correlation with AIx (R 2 = 0.22, p < 0.01) (Fig. 3d).
Parameters of arterial stiffness, AugP (a) and AIx (b), evaluated by PWA of pressure waveforms in the ascending aorta 6 weeks after MI/sham (sham n = 7, vehicle n = 10, rimonabant pre-treatment (Rim pre-tr.) n = 11, rimonabant treatment (Rim) n = 10); c representative pressure waveforms obtained from ascending aorta in vehicle (left) and rimonabant (right) groups; d inverse correlation between AIx and maximal first derivative of developed LV pressure (n = 38); e hydroxyproline concentration in ascending aorta 6 weeks after MI/sham (n = 3–4); ## p < 0.01 vs. sham; *p < 0.05 vs. vehicle; **p < 0.01 vs. vehicle
Collagen content and expression of TGF-β1 in the heart and cardiac fibroblasts
To further test whether rimonabant may prevent post-infarct remodelling, we studied collagen content in the heart by measuring tissue hydroxyproline concentration in the septum. Six weeks post MI, heart hydroxyproline in vehicle-treated animals was increased twofold compared with sham-operated rats, whereas rimonabant pre-treatment significantly attenuated this increase (Fig. 4b). Interestingly, rimonabant also reduced hydroxyproline concentration in the ascending aorta (Fig. 3e). Consistently, less collagen accumulation was found in the heart after rimonabant treatment as demonstrated by staining with the collagen-specific dye Sirius red (Fig. 4a).
Cardiac fibrosis and TGF-β1 expression in the LV 6 weeks post MI. a Microphotographs of LV myocardium stained with the collagen-specific dye Sirius red. Collagen fibres appear as red structures, and myocytes are yellow (magnification, ×20). A diffuse interstitial fibrosis is evident in vehicle-treated rats. b Hydroxyproline content in heart septum 6 weeks post MI (n = 3). c Relative expression of TGF-β1 mRNA in LV (n = 3). d Relative expression of TGF-β1 protein in LV and representative Western blot (n = 3); # p < 0.05 vs. sham; ## p < 0.01 vs. sham; *p < 0.05 vs. vehicle. e Rimonabant reduces IL-1-stimulated expression of TGF-β1 mRNA in cardiac fibroblasts analysed by real-time PCR; ***p < 0.001 vs. un-stimulated control; ## p < 0.01 and ### p < 0.001 vs. IL-1 stimulation (n = 3)
Since fibrosis is thought to be partially mediated by transforming growth factor-β1 (TGF-β1), a potent stimulator of collagen-producing cardiac fibroblasts, the expression of this factor was investigated in the peri-infarcted LV tissues. Six weeks post MI, TGF-β1 expression in the LV was up-regulated both at the mRNA (15-fold) and protein (7.1-fold) levels in the vehicle compared with the sham group. Rimonabant significantly attenuated both mRNA and protein TGF-β1 increase (Fig. 4c, d). In primary cardiac fibroblasts, rimonabant also strongly down-regulated the IL-1α-stimulated increase of mRNA TGF-β1 (Fig. 4e).
Regulation of MMP-9 by rimonabant in the heart and cardiac fibroblasts
Six weeks after MI, the mRNA levels of MMP-9 were up-regulated in the vehicle group compared to the sham group (Fig. 5a). Rimonabant pre-treatment and treatment reduced the MMP-9 levels by trend. Therefore, we further investigated the effect of rimonabant on the MMP-9 activity in isolated rat cardiac fibroblasts and cardiomyocytes.
Influence of rimonabant on the expression and activity of MMPs. a Expression of MMP-9 mRNA in LV tissue 6 weeks post MI analysed by real-time PCR (n = 4). b Representative gelatine zymogram loaded with conditioned media from cardiac fibroblasts. c Semi-quantitative analysis of activity of MMPs produced by cardiac fibroblasts measured by gelatine zymography. Bars represent densitometric data of three independent experiments. d Rimonabant reduces IL-1-stimulated expression of MMP-9 mRNA in cardiac fibroblasts analysed by real-time PCR (n = 3); **p < 0.01 and ***p < 0.001 vs. un-stimulated; # p < 0.05, ## p < 0.01 and ### p < 0.001 vs. IL-1 stimulation
As shown in Fig. 5b, c, stimulation of cardiac fibroblasts with IL-1α significantly increased the activity of secreted MMP-9 (p < 0.01) as measured by gelatine zymography. An increase of MMP-2 activity was not significant. Co-stimulation with rimonabant reduced the MMP-9 activity in a dose-dependent manner, whereas MMP-2 activity was reduced only by trend. Again, at mRNA levels, rimonabant dose-dependently down-regulated the IL-1α-stimulated increase of MMP-9, although an increase of MMP-2 was attenuated only at a concentration 1 μM (Fig. 5d). Moreover, in rat primary cardiomyocytes, rimonabant similarly reduced MMP-9 activity, but not MMP-2 activity (data not shown).
Among other investigated proteins, including markers of apoptosis (Fas ligand, caspase 3), inflammation (IL1, IL6, MCP1) and calcium-regulated proteins (SERCA2a, Na+/Ca2+ exchanger, phospholamban), we found that rimonabant in both treatment regimens significantly increased protein content of SERCA2a in the LV 7 days after MI (Supplemental Fig. 3).
Discussion
This study describes the protective effects of the CB1 receptor antagonist rimonabant on cardiac remodelling in a rat model of metabolic syndrome and MI. Pre-treatment with rimonabant prevented LV dilatation and dysfunction both 7 days and 6 weeks after MI which were evidenced by an improvement of LVIDd, LVIDs, EF and FS as well as dP/dt max and dP/dt min. In addition, pre-treatment with rimonabant prevented ECG abnormalities, decreased serum levels of BNP, increased cardiac protein expression of SERCA2a and improved pulse wave reflection.
Cardioprotective properties of rimonabant have been previously demonstrated in acute ischaemia/reperfusion injury [11], a model, where infarct size is influenced by the destructive actions of reperfusion due to mitochondrial Ca2+ overload, increased ROS, development of cardiomyocyte contracture, inflammation and vascular failure [21]. Differing from an ischaemia/reperfusion model, in the current study, permanent ligation of the left coronary artery was performed. In this model, the degree of impairment of LV function is directly related to the extent of myocardial loss [22]. The results obtained 7 days after MI are in agreement with demonstrated cardioprotective actions of rimonabant obtained in other models such as acute ischaemia/reperfusion injury [11] and doxorubicin-induced cardiotoxicity [12].
Increased production of endocannabinoids has previously been reported in acute MI [23], end-stage HF [24] and doxorubicin-induced cardiotoxicity [12]. Increased levels of endocannabinoids decreased myocardial inotropy directly through cannabinoid-binding receptors expressed in the heart, as shown in vivo and in isolated hearts [7, 23, 25]. In line with these studies, we found general induction of CB1 and CB2 receptor gene expression due to experimental MI 6 weeks after operation (219-fold and 279-fold, respectively), while no significant impact on receptor gene expression was evident due to additional pretreatment or treatment with rimonabant (data not shown). Moreover, inhibition of CB1 receptors with rimonabant rapidly increased heart inotropy in rats 6 weeks after MI but not in healthy rats, implying chronic activation of the endocannabinoid system after ischaemic heart injury.
Importantly, preventive treatment was even more effective compared to post-ischaemic treatment regime. This fact is in agreement with the recent study with rimonabant administration for 7 days, but not shortly before ischaemia reduced infarct size by a CB1-related mechanism [11]. It is also known that positive effects of LPS or heat stress-induced preconditioning against ischaemia/reperfusion injury are mediated by endocannabinoids, acting through the CB2 receptor [26, 27]. Future studies should unravel the importance of different signalling pathways, activated by physiological levels of endogenous cannabinoids after CB1 receptor inhibition, in preconditioning the heart against ischaemic injury.
An over-activated endocannabinoid system is known to contribute to obesity through central and peripheral mechanisms [28]. In this study, spontaneously hypertensive obese rats (SHROB or Koletsky rats) were used to investigate the effects of rimonabant on cardiac function in a model that closely resembles human metabolic syndrome. Despite the regular diet, SHROB rats are characterised by obesity, hypertension, hyperinsulinaemia, hyperlipidaemia and nephropathy. Here, we demonstrated that SHROB rats also had depressed systolic function in comparison to age-matched lean Wistar rats, as evidenced by decreased EF and FS. In fact, treatment with rimonabant for 2 weeks improved systolic function and, in parallel, significantly reduced weight gains. Thus, the CB1 receptor blockade in metabolic syndrome may improve cardiac performance in two ways: via direct cardiac protection and via improvement of metabolic status.
We further investigated whether chronic treatment with rimonabant ameliorated adverse post-ischaemic cardiac remodelling. We focused on the post-ischaemic cardiac fibrosis because it may preclude deterioration of cardiac function and progression to HF through increased cardiac stiffness. Additionally, we investigated the effect of rimonabant on TGF-β1 expression, a pro-fibrotic cytokine that stimulates the production of extracellular matrix proteins. TGF-β1 is extensively expressed after ischaemia and associated with post-ischaemic fibrosis that affects not only infarcted but also remote myocardium [29]. This study, to our knowledge, is the first to demonstrate that blockade of CB1 receptors by rimonabant prevented the up-regulation of both mRNA and protein levels of TGF-β1 in the left ventricle after MI. Our in vitro experiment in cardiac fibroblasts demonstrated that rimonabant attenuated the increase of TGF-β1 mRNA, in a dose-dependent manner, suggesting that signalling through CB1 receptors regulate TGF-β1 at the transcriptional level. Consequently, rimonabant decreased collagen accumulation in the remote myocardium after ischaemia as demonstrated histologically and by measuring the concentration of hydroxyproline. These data are also in agreement with a previous report demonstrating an anti-fibrotic effect of CB1 receptor blockade in hepatic fibroblasts [30]. On the other hand, genetic deletion of CB2 receptors lead to activation of cardiac fibroblasts and increased TGF-β1 and collagen production [31], indicating that CB1 and CB2 receptors have opposing effects on fibrotic processes. Thus, the anti-fibrotic effects observed in our study may be a result of both CB1 receptor inhibition and indirect stimulation of unopposed CB2 receptors by increased post-ischaemic levels of endocannabinoids.
Furthermore, it has been recognised that MMPs and the tissue inhibitors of MMPs play an important role in matrix remodelling in cardiac disease [32]. We focused to investigate the expression and activity of the gelatinases MMP-2 and MMP-9 because they are known to possess substrate affinity for denatured fibrillar collagen as well as to exhibit proteolytic activity against elastin and proteoglycans. Indeed, MI led to an up-regulation in mRNA expression of MMP-2 and MMP-9 in the left ventricle 7 days post MI. Although rimonabant did not significantly prevent the increase of mRNA transcripts of MMPs in the myocardium, our in vitro experiments in cardiac fibroblasts clearly demonstrated that rimonabant dose-dependently reduced the activity of MMP-9 but not MMP-2. Further studies should unravel the molecular mechanisms driven by CB1 signalling which are involved in the regulation of MMP activity. In addition, CB1/2 receptors are present in immune cells [33] through which they could modulate cytokine secretion and influence matrix remodelling, but addressing this issue was beyond the scope of the current investigations.
Increased pulse wave reflection is known to deteriorate cardiac output by increasing the LV afterload. Endothelial dysfunction and augmented collagen accumulation are important pathophysiological mechanisms which contribute to increased wave reflection in patients with HF [34, 35]. It was initially suggested that inhibition of CB1 receptor deteriorates endothelial function after MI [13]. In contrast, a recent study provided evidence that inhibition of CB1 receptor improves endothelium-dependent relaxation of aortic rings by mechanism that involves down-regulation of AT1 receptor expression [16]. To our knowledge, current study provides the first in vivo experimental evidence that pulse wave reflection and probably arterial stiffness progressively increases after MI. Additionally, we demonstrated that inhibition of CB1 receptor by rimonabant ameliorated pulse wave reflection after MI in vivo. Reduced deposition of collagen in the ascending aorta might alter arterial stiffness, though pulse wave velocity as a direct measure of arterial stiffness was not measured. We observed that dP/dt max inversely correlated with AIx. Additionally, the beneficial effect of rimonabant on wave reflections is mirrored by a raise in aortic diastolic pressure compared to vehicle. Therefore, it is likely that reduced AIx partly contributed to the improvement in cardiac function by reducing afterload in systole and preserving myocardial perfusion during diastole.
Rimonabant was the first selective inhibitor of cannabinoid receptor to be used for treating obesity. Despite its side effects resulting from the actions at CB1 receptors in the brain, the effects of CB1 receptor blockade, as shown by rimonabant in our study, might show the potential of endocannabinoid receptor blockers as a pharmacological tool in the cardiovascular system. In the light of current investigations, the CB1 receptor inhibitors, which do not penetrate the blood–brain barrier, could be of clinical relevance in cardiology. Indeed, AM6545, another CB1 receptor antagonist, was earlier shown to lack central nervous system side effects [36]. Nonetheless, this neutral antagonist induced weight-independent improvements in glucose homeostasis and plasma lipid profiles in mice. While we did not detect a significant impact on IL-1α-stimulated MMP secretion in primary cardiac fibroblasts (data not shown), which was in contrast to the inverse antagonist rimonabant, other effects on cardiovascular cells or disorders might exist. Furthermore, additional approaches interfering with the CB receptor system might pave the way to develop newer compounds with beneficial impact on cardiovascular and metabolic disorders, while the central nervous system remains less affected than by rimonabant.
In summary, this study demonstrated that long-term inhibition of CB1 receptors with rimonabant improved post-ischaemic cardiac function by preventing the adverse myocardial remodelling and reducing the pulse wave reflections. Furthermore, rimonabant improved depressed systolic function in animals with metabolic syndrome. This study is of clinical relevance because it supports the hypothesis that the endocannabinoid system could represent a novel pharmacological target in post-ischaemic HF treatment.
Study limitation
MI could be reliably induced only in previously healthy Wistar rats but not in SHROB rats due to high operation-associated mortality rate of SHROB rats. Importantly, chronicle conditions including hypertension, hypertrophy or diabetes could interfere with or even completely abrogate treatment effects [37]. This limitation should be addressed by future studies.
References
Tamargo J, López-Sendón J (2011) Novel therapeutic targets for the treatment of heart failure. Nat Rev Drug Discov 10(7):536–555
De Petrocellis L, Cascio MG, Di Marzo V (2004) The endocannabinoid system: a general view and latest additions. Br J Pharmacol 141(5):765–774
Matsuda LA, Lolait SJ, Brownstein MJ, Young AC, Bonner TI (1990) Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature 346(6284):561–564
Pacher P, Mukhopadhyay P, Mohanraj R, Godlewski G, Bátkai S, Kunos G (2008) Modulation of the endocannabinoid system in cardiovascular disease: therapeutic potential and limitations. Hypertension 52(4):601–607
Després J-P, Golay A, Sjöström L (2005) Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N Engl J Med 353(20):2121–2134
Felder CC, Nielsen A, Briley EM, Palkovits M, Priller J, Axelrod J, Nguyen DN, Richardson JM, Riggin RM, Koppel GA et al (1996) Isolation and measurement of the endogenous cannabinoid receptor agonist, anandamide, in brain and peripheral tissues of human and rat. FEBS Lett 393(2–3):231–235
Bonz A, Laser M, Küllmer S, Kniesch S, Babin-Ebell J, Popp V, Ertl G, Wagner JA (2003) Cannabinoids acting on CB1 receptors decrease contractile performance in human atrial muscle. J Cardiovasc Pharmacol 41(4):657–664
Gebremedhin D, Lange AR, Campbell WB, Hillard CJ, Harder DR (1999) Cannabinoid CB1 receptor of cat cerebral arterial muscle functions to inhibit L-type Ca2+ channel current. Am J Physiol 276(6 Pt 2):H2085–H2093
Liu J, Gao B, Mirshahi F, Sanyal AJ, Khanolkar AD, Makriyannis A, Kunos G (2000) Functional CB1 cannabinoid receptors in human vascular endothelial cells. Biochem J 346(Pt 3):835–840
Sterin-Borda L, Del Zar CF, Borda E (2005) Differential CB1 and CB2 cannabinoid receptor-inotropic response of rat isolated atria: endogenous signal transduction pathways. Biochem Pharmacol 69(12):1705–1713
Lim SY, Davidson SM, Yellon DM, Smith CCT (2009) The cannabinoid CB1 receptor antagonist, rimonabant, protects against acute myocardial infarction. Basic Res Cardiol 104(6):781–792
Mukhopadhyay P, Bátkai S, Rajesh M, Czifra N, Harvey-White J, Haskó G, Zsengeller Z, Gerard NP, Liaudet L, Kunos G et al (2007) Pharmacological inhibition of CB1 cannabinoid receptor protects against doxorubicin-induced cardiotoxicity. J Am Coll Cardiol 50(6):528–536
Wagner JA, Hu K, Karcher J, Bauersachs J, Schäfer A, Laser M, Han H, Ertl G (2003) CB(1) cannabinoid receptor antagonism promotes remodeling and cannabinoid treatment prevents endothelial dysfunction and hypotension in rats with myocardial infarction. Br J Pharmacol 138(7):1251–1258
Rinaldi-Carmona M, Barth F, Héaulme M, Shire D, Calandra B, Congy C, Martinez S, Maruani J, Néliat G, Caput D (1994) SR141716A, a potent and selective antagonist of the brain cannabinoid receptor. FEBS Lett 350(2–3):240–244
Matias I, Di Marzo V (2007) Endocannabinoids and the control of energy balance. Trends Endocrinol Metab 18(1):27–37
Tiyerili V, Zimmer S, Jung S, Wassmann K, Naehle CP, Lütjohann D, Zimmer A, Nickenig G, Wassmann S (2010) CB1 receptor inhibition leads to decreased vascular AT1 receptor expression, inhibition of oxidative stress and improved endothelial function. Basic Res Cardiol 105(4):465–477
Kaschina E, Grzesiak A, Li J, Foryst-Ludwig A, Timm M, Rompe F, Sommerfeld M, Kemnitz UR, Curato C, Namsolleck P et al (2008) Angiotensin II type 2 receptor stimulation: a novel option of therapeutic interference with the renin-angiotensin system in myocardial infarction? Circulation 118(24):2523–2532
Paulis L, Becker STR, Lucht K, Schwengel K, Slavic S, Kaschina E, Thöne-Reineke C, Dahlöf B, Unger T, Steckelings U (2012) Direct angiotensin II type 2 receptor stimulation in Nω-nitro-l-arginine-methyl ester-induced hypertension: the effect on pulse wave velocity and aortic remodeling. Hypertension 59(2):485–492
Agocha AE, Eghbali-Webb M (1997) A simple method for preparation of cultured cardiac fibroblasts from adult human ventricular tissue. Mol Cell Biochem 172(1–2):195–198
Vosgerau U, Lauer D, Unger T, Kaschina E (2010) Cleaved high molecular weight kininogen, a novel factor in the regulation of matrix metalloproteinases in vascular smooth muscle cells. Biochem Pharmacol 79(2):172–179
Piper HM, Meuter K, Schäfer C (2003) Cellular mechanisms of ischemia–reperfusion injury. Ann Thorac Surg 75(2):S644–S648
Pfeffer MA, Pfeffer JM, Fishbein MC, Fletcher PJ, Spadaro J, Kloner RA, Braunwald E (1979) Myocardial infarct size and ventricular function in rats. Circ Res 44(4):503–512
Wagner JA, Hu K, Bauersachs J, Karcher J, Wiesler M, Goparaju SK, Kunos G, Ertl G (2001) Endogenous cannabinoids mediate hypotension after experimental myocardial infarction. J Am Coll Cardiol 38(7):2048–2054
Weis F, Beiras-Fernandez A, Sodian R, Kaczmarek I, Reichart B, Beiras A, Schelling G, Kreth S (2010) Substantially altered expression pattern of cannabinoid receptor 2 and activated endocannabinoid system in patients with severe heart failure. J Mol Cell Cardiol 48(6):1187–1193
Ford WR, Honan SA, White R, Hiley CR (2002) Evidence of a novel site mediating anandamide-induced negative inotropic and coronary vasodilatator responses in rat isolated hearts. Br J Pharmacol 135(5):1191–1198
Lagneux C, Lamontagne D (2001) Involvement of cannabinoids in the cardioprotection induced by lipopolysaccharide. Br J Pharmacol 132(4):793–796
Joyeux M, Arnaud C, Godin-Ribuot D, Demenge P, Lamontagne D, Ribuot C (2002) Endocannabinoids are implicated in the infarct size-reducing effect conferred by heat stress preconditioning in isolated rat hearts. Cardiovasc Res 55(3):619–625
Cota D, Marsicano G, Tschöp M, Grübler Y, Flachskamm C, Schubert M, Auer D, Yassouridis A, Thöne-Reineke C, Ortmann S et al (2003) The endogenous cannabinoid system affects energy balance via central orexigenic drive and peripheral lipogenesis. J Clin Invest 112(3):423–431
Dobaczewski M, Chen W, Frangogiannis NG (2011) Transforming growth factor (TGF)-β signaling in cardiac remodeling. J Mol Cell Cardiol 51(4):600–606
Teixeira-Clerc F, Julien B, Grenard P, Tran Van Nhieu J, Deveaux V, Li L, Serriere-Lanneau V, Ledent C, Mallat A, Lotersztajn S (2006) CB1 cannabinoid receptor antagonism: a new strategy for the treatment of liver fibrosis. Nat Med 12(6):671–676
Defer N, Wan J, Souktani R, Escoubet B, Perier M, Caramelle P, Manin S, Deveaux V, Bourin MC, Zimmer A et al (2009) The cannabinoid receptor type 2 promotes cardiac myocyte and fibroblast survival and protects against ischemia/reperfusion-induced cardiomyopathy. FASEB J 23(7):2120–2130
Spinale FG (2007) Myocardial matrix remodeling and the matrix metalloproteinases: influence on cardiac form and function. Physiol Rev 87(4):1285–1342
Galiègue S, Mary S, Marchand J, Dussossoy D, Carrière D, Carayon P, Bouaboula M, Shire D, Le Fur G, Casellas P (1995) Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur J Biochem 232(1):54–61
Ramsey MW, Goodfellow J, Jones CJ, Luddington LA, Lewis MJ, Henderson AH (1995) Endothelial control of arterial distensibility is impaired in chronic heart failure. Circulation 92(11):3212–3219
Bonapace S, Rossi A, Cicoira M, Golia G, Zanolla L, Franceschini L, Conte L, Marino P, Vassanelli C (2006) Aortic stiffness correlates with an increased extracellular matrix turnover in patients with dilated cardiomyopathy. Am Heart J 152(1):93.e1–93.e6
Tam J, Vemuri VK, Liu J, Bátkai S, Mukhopadhyay B, Godlewski G, Osei-Hyiaman D, Ohnuma S, Ambudkar SV, Pickel J et al (2010) Peripheral CB1 cannabinoid receptor blockade improves cardiometabolic risk in mouse models of obesity. J Clin Invest 120(8):2953–2966
Ferdinandy P, Schulz R, Baxter GF (2007) Interaction of cardiovascular risk factors with myocardial ischemia/reperfusion injury, preconditioning, and postconditioning. Pharmacol Rev 59(4):418–458
Acknowledgments
This study was supported by Sanofi-Aventis Deutschland GmbH.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(PDF 241 kb)
Rights and permissions
About this article
Cite this article
Slavic, S., Lauer, D., Sommerfeld, M. et al. Cannabinoid receptor 1 inhibition improves cardiac function and remodelling after myocardial infarction and in experimental metabolic syndrome. J Mol Med 91, 811–823 (2013). https://doi.org/10.1007/s00109-013-1034-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-013-1034-0