Abstract
Many cytokines are involved in the pathogenesis of autoimmune diseases and are recognized as relevant therapeutic targets to attenuate inflammation, such as tumor necrosis factor (TNF)-α in rheumatoid arthritis (RA) and interferon (IFN)-α/γ in systemic lupus erythematosus (SLE). To relate the transcriptional imprinting of cytokines in a cell type- and disease-specific manner, we generated gene expression profiles from peripheral monocytes of SLE and RA patients and compared them to in vitro-generated signatures induced by TNF-α, IFN-α2a, and IFN-γ. Monocytes from SLE and RA patients revealed disease-specific gene expression profiles. In vitro-generated signatures induced by IFN-α2a and IFN-γ showed similar profiles that only partially overlapped with those induced by TNF-α. Comparisons between disease-specific and in vitro-generated signatures identified cytokine-regulated genes in SLE and RA with qualitative and quantitative differences. The IFN responses in SLE and RA were found to be regulated in a STAT1-dependent and STAT1-independent manner, respectively. Similarly, genes recognized as TNF-α regulated were clearly distinguishable between RA and SLE patients. While the activity of SLE monocytes was mainly driven by IFN, the activity from RA monocytes showed a dominance of TNF-α that was characterized by STAT1 down-regulation. The responses to specific cytokines were revealed to be disease-dependent and reflected the interplay of cytokines within various inflammatory milieus. This study has demonstrated that monocytes from RA and SLE patients exhibit disease-specific gene expression profiles, which can be molecularly dissected when compared with in vitro-generated cytokine signatures. The results suggest that an assessment of cytokine-response status in monocytes may be helpful for improvement of diagnosis and selection of the best cytokine target for therapeutic intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic rheumatic diseases like systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) define a group of disorders with unknown etiology, where both genetic predisposition and environmental factors contribute to disease pathogenesis [1]. There are several lines of evidence suggesting that cytokines play an important role in the etiopathogenesis of these diseases and in the maintenance of chronic inflammation, including type I interferon (IFN), BAFF, interleukin (IL)-6, and tumor necrosis factor (TNF)-α [2–4]. To estimate the role of a particular cytokine involved in the immune response is complex, considering the fact that the immune response is orchestrated by multiple cytokines acting within a complex cytokine network. Despite this complex interaction of cytokines, therapeutic strategies in rheumatic diseases that target a particular cytokine, such as TNF-α, IL-1, or IL-6, are very successful, even though a complete suppression of chronic inflammation, and thereby a real cure of the disease, is still not achieved.
To reveal cytokine networks in chronic rheumatic diseases and thereby to identify new molecular targets for therapeutic development, global gene expression profiling strategies have been extensively used [5]. So far, the gene expression profiles from many rheumatic diseases have been reported, including SLE, RA, psoriatic arthritis, dermatomyositis, and systemic onset juvenile idiopathic arthritis (SOJIA) [6–11]. Furthermore, it has been demonstrated that cytokines might shape the transcriptional profile in chronic rheumatic diseases when the type I IFN signature was identified in SLE patients [8, 12]. Later on, the type I IFN signature was recognized in other diseases, such as dermatomyositis, predisposed diabetic patients, a subgroup of RA patients, and can be found in RA and SOJIA patients after anti-TNF-α treatment [7, 9, 10, 13–15]. However, the identification of IFN-regulated genes in various rheumatic diseases showed obvious dissimilarity. The magnitude of changes in gene expression and the number of genes that constitute the IFN response was superior in SLE compared with other rheumatic diseases [8, 9]. A comparison of these previous findings has been complicated by the fact that primarily peripheral blood mononuclear cells (PBMCs) or whole blood cells were used in these studies. It is known that inflammation affects the cellular composition of PBMCs: an increased percentage of activated monocytes can be found in RA and SLE while a decreased percentage of T and B cells are seen in active tuberculosis [6, 14, 16]. An obvious strategy to overcome this experimental limitation is to generate transcriptional profiles of functionally well-defined cell types [16–18].
In this study, we have focused on peripheral blood monocytes, which play an important role in the pathogenesis of chronic rheumatic diseases, including RA and SLE [19–21]. Although, these diseases are mainly manifested in tissues, such as the joints in RA or the kidney and skin in SLE, there are indications that disease-specific transcriptional imprints are already detectable at the level of peripheral monocytes [22, 23]. Therefore, in this study, we focus on characterization of gene expression patterns in a disease-specific and cell-specific manner. The main challenge of this study was to estimate the contribution of cytokines in shaping the gene expression profiles of monocytes isolated from RA and SLE patients. For this purpose, we used in vitro-generated TNF-α, IFN-α2a, and IFN-γ cytokine signatures and compared them with disease-specific profiles. This experimental design allowed us to address the following questions. (1) Are monocytes a suitable cell type to identify disease-specific gene expression profiles? (2) Do monocytes reflect cytokine-specific gene expression profiles after in vitro stimulation? (3) Do comparisons between disease-specific and cytokine-generated gene expression profiles reveal a dominance of a particular cytokine in the pathogenesis of disease? This information could assist in estimating an individual cytokine profile in rheumatic patients, which would finally permit individualized therapy recommendations.
Materials and methods
Clinical classification of patients
Clinical characteristics and treatment of nine SLE and eight RA patients are included in Table 1. Clinical characteristics of additional patients used for prediction analyses, five SLE, and four RA, are also included, and they are labeled as testing samples.
The group of healthy donors included 12 persons whose age was in the range of 20–60. They were without any medications or indications of inflammation (ESR, <30 mm/h and CRP, <5 mg/l).
Blood collection and cell separation
Fifty milliliters of blood from SLE and RA patients or from healthy donors was collected in Vacutainer Heparin Tubes (Becton Dickinson, Heidelberg, Germany). The isolation of monocytes was performed as previously described [24]. The Ethics Committee of the Charité Universitätsmedizin Berlin approved this study. Written informed consent was obtained from all patients and healthy donors.
Blood collection and study design of in vitro-generated TNF-α, IFN-α2a, and IFN-γ signatures
A total of 250 ml of peripheral blood from seven healthy donors was collected in Vacutainer Heparin Tubes (Becton Dickinson, Heidelberg, Germany). Healthy donors selected for this study were not taking any medications. Six of the healthy donors were Caucasian and one was of Asian origin. All were non-smokers, four donors were females (ages 24 to 29), and three were males (ages 24 to 33). Three donors were asked more than once for blood donation. Samples that represented unstimulated controls were immediately processed. Other samples were incubated for 1.5 h at 37 °C either without stimulus or were stimulated with 100 ng/ml TNF-α (Peprotech, London, UK), 100 ng/ml IFN-α2a (Immunotools, Friesoythe, Germany), or 100 ng/ml IFN-γ (Peprotech, London, UK). After stimulation, blood samples were processed identically to patient samples [24].
RNA isolation, Affymetrix gene chip hybridization, and quality checks
RNA isolation, Affymetrix gene chip hybridization and quality checks were performed as previously described [22, 24]. Details are provided as Supplementary electronic material.
Selection of differentially expressed genes and chip data analysis
The gene chip analysis, including parameter selection was performed with the BioRetis database, and details are provided as Supplementary electronic material. All chip data are publicly available in GEO.
Results
Peripheral blood monocytes from SLE and RA patients displayed disease-specific gene expression profiles
Monocytes isolated from peripheral blood of SLE patients were characterized by 1,853 probe sets (about 1,220 genes) that were differentially expressed in pair-wise comparisons between 9 SLE patients and 12 normal donors (Fig. 1a; Supplementary Table 1, WS1). Out of these 1,853 probe sets, 926 were up-regulated and 927 were down-regulated. Three SLE patients, referred as SL-1, SL-2, and SL-7, showed weaker changes in gene expression when compared with other SLE patients. Notably, these patients were characterized by less active disease.
Monocytes from SLE and RA patients exhibit different transcriptional profiles. a Gene expression profile of monocytes isolated from SLE patients. Hierarchical clustering of 1,853 probe sets that were differentially expressed between SLE (yellow) and ND (gray) in >30 % of all pair-wise comparisons. b Gene expression profile of monocytes isolated from RA patients. Hierarchical clustering of 1,627 probe sets that were differentially expressed between RA (red) and ND (gray) in >30 % of all pair-wise comparisons. Each row represents one probe set and each column indicates one subject. Colored bar indicates normalized expression values below (green) and above (red) the mean expression (range set to ±2.0). c PCA separates SLE and RA as two different diseases. Based on gene expression profiles from SLE and RA monocytes, these two diseases were classified as distinct diseases. Signals from 2,716 probe sets were used for PCA, including 1,853 probe sets from the SLE profile and 1,627 probe sets from the RA profile (764 probe sets were changed in both diseases, either in the same or opposite directions). The first two components of PCA are presented in the figure (PC1 and PC2). SLE patients, RA patients, and ND were colored in yellow, red, and gray, respectively
Transcriptional profiles of monocytes isolated from RA patients identified 1,627 probe sets (about 1,070 genes) as differentially expressed compared with normal donors (Fig. 1b; Supplementary Table 1, WS2). In pair-wise comparisons between 8 RA patients and 12 normal donors, 1,005 probe sets were up-regulated and 622 were down-regulated. Heterogeneity between RA patients was more obvious than between SLE patients. A subgroup of RA patients was characterized by strong alterations in gene expression (RA1, RA3, RA5, and RA7), two patients showed weaker alterations (RA2 and RA4), and two patients did not exhibit any changes that differentiated them from healthy donors (RA9 and RA11).
A principal component analysis (PCA) was performed, and all probe sets that constitute SLE and RA profiles were included in this analysis. PCA clearly showed that the monocytes derived from patients with these two diseases displayed disease-specific profiles (Fig. 1c).
Ingenuity pathway analysis (IPA) assigned these two diseases to discrete molecular networks. Cytokines, such as TNF-α, IL1, and IL8, were identified as central players in the networks that characterized both SLE and RA profiles. Nevertheless, they were either regulated in opposite directions, as seen for TNF-α and IL8, or they were constituents of distinct molecular networks, as identified for IL1β (Supplementary Fig. 1a–d).
In vitro stimulation of monocytes in whole blood by TNF-α, IFN-α2a or IFN-γ identified cytokine-shared, cytokine-predominant, and cytokine-specific genes
Stimulation of monocytes with pro-inflammatory cytokines, such as TNF-α, IFN-α2a, and IFN-γ, for 1.5 h resulted in distinctive gene expression profiles. When compared with unstimulated control samples, the gene expression profiles of monocytes stimulated with TNF-α, IFN-α2a, or IFN-γ were characterized by differential expression of 5,683, 4,571, and 3,901 probe sets, respectively. Concerning the architecture of Affymetrix gene chips, these numbers of probe sets is related to about 2,630 TNF-α-, 2,120 IFN-α2a-, and 1,800 IFN-γ-regulated genes. Combined, TNF-α, IFN-α2a, and IFN-γ profiles exhibited differential expression of 8,950 probe sets (Fig. 2a). Responses to each of these three individual stimuli are presented in Supplementary Table 2 (WS1–3).
a Gene expression profiles of monocytes stimulated in vitro with TNF-α, IFN-α2a, or IFN-γ for 1.5 h. In total, 8,950 probe sets were differentially expressed after TNF-α, IFN-α2a, and IFN-γ stimulation when compared with unstimulated 1.5 h samples. More precisely, 5,683 probe sets were differentially expressed following TNF-α stimulation, 4,571 following IFN-α2a, and 3,901 following IFN-γ stimulation; 8,950 probe sets were used for hierarchical clustering of three TNF-α, 7 IFN-α2a, and 7 IFN-γ, 11 samples incubated for 1.5 h without any stimulus, and 8 unstimulated samples that were immediately processed. b PCA differentiates gene expression profiles induced by TNF-α, IFN-α2a, and IFN-γ from unstimulated samples. Signals from 8,950 probe sets were used for PCA, including 5,683 probe sets that determined TNF-α stimulation, 4,571 probe sets that determined IFN-α2a stimulation, and 3,901 probe sets that designated IFN-γ stimulation. The number of 8,950 probe sets is related to the probe sets that were differentially expressed by a particular cytokine or shared by two or all three of them. The first two components of PCA were used for data presentation (PC1 and PC2). TNF-α-, IFN-α2a-, and IFN-γ-regulated genes were colored in green, dark blue, and light blue, respectively
The analysis of in vitro-generated cytokine signatures identified probe sets specific for either one cytokine or shared between two or three cytokines. For example, CCL2, CCL3, and CCL4 were induced by all three cytokines (Table 2). However, stimulation with IFN-α2a and IFN-γ led to an up-regulation in CCL2 which were stronger as compared with TNF-α stimulation (FCs of 5, 58, and 59 for TNF-α, IFN-α2a, and IFN-γ, respectively). The expression of CCL4 was more strongly induced by TNF-α than by IFN-α2a or IFN-γ (FCs of 27, 7, and 4 for TNF-α, IFN-α2a, and IFN-γ, respectively). Therefore, if the up-regulation of genes is strongly induced by one cytokine in comparisons to the others, these genes were considered predominantly regulated by this particular cytokine (as described in Supplementary electronic material). However, genes that were altered by just one of these cytokines were considered to be cytokine-specific. Examples of cytokine-specific genes include CCL20 and CCL23, which were induced only by TNF-α. The Supplementary Table 3 includes all 8,950 probe sets, and those determined as specific, predominant, or shared are indicated in separate columns.
As mentioned above and shown by PCA in Fig. 2b, IFN-α2a and IFN-γ exhibited similar profiles and the following cytokines were identified as being up-regulated by both IFNs: CCL2, CCL3, CCL4, CCL7, CCL8, CXCL9, CXCL10, CXCL11, IL15, IL7, and IL27. Furthermore, both types of IFNs induced expression of the following genes: STAT1, STAT2, IFI16, IFI27, IFI35, and IFI44. Although responses to types I and II IFNs were almost identical, stimulus-specific genes could be identified. For example, the up-regulation of IL15R, CD163, CD55, SOCS2, and TNFSF18 was specific for IFN-α2a while the up-regulation of CCR5, CD53, CD97, CIITA, CXCL16, ICOSLG, JAK2, JAK3, and JUN was identified as IFN-γ specific.
Venn diagrams in Supplementary Fig. 2a, b display an overview of probe sets identified as cytokine shared or cytokine specific. Most of cytokine-shared probe sets changed their expression in the same direction. Nevertheless, 670 probe sets belong to the cytokine shared, but their expression changed in opposite directions. More precisely, 665 probe sets were altered in opposite directions between TNF-α and IFNs, and 10 probe sets between IFN-α2a and IFN-γ (Supplementary Table 3). Five of these ten probe sets changed in the same direction with TNF-α and therefore, the total number of probe sets is 670. The probe sets that were regulated in opposite directions by TNF-α and IFNs (665 probe sets) are also presented in the Supplementary Fig. 3. Among the genes that were up-regulated by TNF-α but down-regulated by IFNs, we identified CXCL1, CXCL2, CXCL3, IL8, TNFSF8, and TNFSF10. In contrast, genes such as IFIT1, IFIT3, IFIT5, IFI16, IFI44, IFI44L, OAS1, OAS2, and STAT1 were down-regulated by TNF-α and up-regulated by IFNs. These genes were frequently detected in different inflammatory diseases, including SLE and RA, as summarized below.
Disease dependent diversity of IFN-α2a-, IFN-γ-, and TNF-α-regulated genes in SLE and RA
Disease-specific IFN-α2a imprints in SLE and RA monocytes
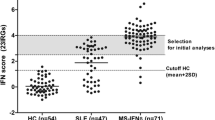
Comparisons between the IFN-α2a signature and profiles from SLE and RA patients revealed an overlap of 551 and 328 differentially expressed probe sets, respectively (Supplementary Table 1, the last three columns in WS1 and WS2 represent cytokine-regulated genes in SLE and RA, respectively). An IFN-α2a imprint was identified in six out of nine SLE patients (Fig. 3a, b), and it was not obvious in patients that were characterized by a more inactive diseases course (SL-1, SL-2, and SL-7). The same 551 probe sets, that determined the IFN-α2a imprint in SLE, were used for classification of the same nine SLE patients by prediction analysis of microarrays algorithm (PAM). In total, eight out of nine patients were classified as SLE (Fig. 3c). Five additional patients with SLE were used for testing the relevance of these 551 probe sets. These extra patients were not used for initial selection of IFN-α2a-regulated probe sets. All five patients were classified as SLE (Fig. 3d).
Disease-modulated IFN-α2a-responses in SLE and RA monocytes. a A total number of 551 differentially expressed probe sets obtained after in vitro stimulation by IFN-α2a were also identified in SLE monocytes, and they were used for hierarchical cluster (HC) analysis of SLE and ND samples. b The same 551 probe sets as in (a) were selected from the in vitro-generated IFN-α2a reference signature and arranged in the same order as identified by HC of SLE and ND in (a). c In total, 551 probe sets that were presented by hierarchical clustering in (a) were used for prediction analysis of microarrays (PAM) of identical SLE and ND samples. d The same 551 probe sets as in (a), (b), and (c) were used for PAM analysis of testing samples, which represented an independent cohort of SLE patients. e A total of 328 differentially expressed probe sets obtained after in vitro stimulation by IFN-α2a were also identified in RA monocytes, and they were used for HC analysis of RA and ND samples. f The same 328 probe sets as in (e) were selected from the in vitro-generated IFN-α2a reference signature and arranged in the same order as identified by HC of RA and ND in (e). g In total, 328 probe sets that were presented by hierarchical clustering in (e) were used for PAM analysis of identical RA and ND samples. h The same 328 probe sets as in (e), (f), and (g) were used for PAM analysis of testing samples, which represented an independent cohort of RA patients. i In total, 746 probe sets determined IFN-α2a imprints in SLE and RA, and they were used for HC of SLE, RA, and ND samples. Within 746 probe sets, 551 and 328 probe sets were related to IFN-α2a imprint in SLE and RA, respectively, and 133 probe sets were shared between them. j The same 746 probe sets as in (i) were selected from the in vitro-generated IFN-α2a reference signature and arranged in the same order as identified by HC of SLE, RA, and ND in (i). SLE patients, RA patients, and ND were colored in yellow, red, and gray, respectively. IFN-α2a and unstimulated samples were colored in dark blue and gray, respectively.
The SLE-associated IFN-α2a imprint included the up-regulation of the following probe sets: CCL2, CCL8, CD164, CXCL10, CXCL11, FAS, IFI16, IFI27, IFI44, IFI44L, IL15, IL15RA, MX1, MX2, OAS1, OAS2, OAS3, OASL, SIGLEC1, SSB, STAT1, STAT2, STAT3, and TNFSF10. The IFN-α2a imprint in SLE also included the following probe sets that were down-regulated: CENTD2, CYP1B1, GPX4, ID2, IER3, IRS2, JUN, KLF13, KLF2, KLF4, PTAFR, TNFAIP2, and TNFRSF10B.
A distinct IFN-α2a-related imprint was identified in five out of eight patients with RA (Fig. 3e, f). The IFN-α2a imprint in RA included the up-regulation of CD163, CD55, CITED2, IL6ST, FOSL2, MAFF, ATF3, and MT2A and the down-regulation of CCNG2, CXCR4, ICAM2, FADD, GPX3, NGRN, PURA, TNFSF8, and TP53.
IFN-α2a-regulated genes in RA (328 probe sets) were used for a classification of RA patients by PAM. The same RA patients, RA4, RA7, and RA11, which did not show the IFN-α2a imprint by hierarchical clustering, revealed identical results by PAM (Fig. 3g). Four additional RA patients were utilized for estimating the probability that 328 probe sets were relevant for an accurate classification of new RA patients. Three out of four patients were classified as RA (Fig. 3h).
Combined, 746 probe sets were detected in SLE and RA that were regulated by IFN-α2a, and hierarchical clustering of these probe sets showed distinctive patterns of IFN-α2a-regulated genes in SLE and RA (Fig. 3i, j). Out of these 746 probe sets, only 133 were common for both diseases. Based on the number of genes regulated by this cytokine, it was obvious that the IFN-α2a imprint was more dominant in SLE than RA, and that some SLE patients showed no IFN-α2a response at all. The magnitude of changes in gene expression was calculated for the top 50 probe sets induced by IFN-α2a both in SLE and RA (Supplementary Fig. 4a). The quantification of disease-specific IFN-α2a imprints showed that this imprint was more dominant in SLE patients as compared with those in RA. Nevertheless, SLE1, SLE2, and SLE7 revealed a weak response to IFN-α2a while RA3 showed a very strong response to this cytokine. Although the magnitude of changes in gene expression induced by IFN-α2a in RA3 was in the range of those induced in SLE, the response to IFN-α2a in RA was qualitatively dissimilar as compared with those in SLE.
By characterizing the IFN-α2a-regulated genes in SLE and RA with IPA, a high functional dissimilarity between the IFN-α2a imprints in SLE and RA was revealed. The molecular network that exhibited an IFN-α2a-response in SLE was dominated by the up-regulation of STAT1, STAT2, IRF7, IRF9, CXCL10, CXCL11, and CCL2 while the network identified as IFN-α2a-response in RA revealed an up-regulation of CCL3, CCL4, and ATF3, and a down-regulation of TP53, FOXO3, and CXCR4 (Supplementary Fig. 5a, b).
To visualize the patterns of gene expression from SLE and RA monocytes in three-dimensional space and to mark those that constitute the cytokine-regulated genes in these diseases, we applied a terrain map analysis [25]. The SLE profile (1,853 probe sets) was displayed with one central peak, which presents one dominant group of co-regulated genes (Fig. 4a). When the SLE profile was overlaid with IFN-α2a-regulated genes, the dominant group of co-regulated genes was revealed to be enriched by those regulated by IFN-α2a. Unlike the gene expression profile from SLE patients, the profile from RA patients revealed a few dominant peaks that represented a few groups of co-expressed genes (Fig. 4b). An overlay of the RA profile with IFN-α2a-regulated genes demonstrated that the genes regulated by this cytokine are uniformly distributed within the profile.
Gene expression terrain map analysis revealed groups of co-regulated genes in the SLE and RA transcriptomes and emphasizes the existence of disease-specific IFN-α2a imprints in monocytes. Terrain map analysis revealed groups of co-regulated probe sets in SLE (a) and RA (b). The height of the peaks indicates the number of co-regulated probe sets, which are shown as dots located above the terrain peaks. a IFN-α2a regulated probe sets were ascertained in SLE monocytes as a group of co-regulated genes and they belong to the highest peak; 551 probe sets regulated by IFN-α2a in SLE were marked as dark blue dots located above the terrain peaks. b IFN-α2a-regulated genes were more homogeneously spread throughout the profile of RA monocytes; 328 probe sets regulated by IFN-α2a in RA were marked as dark blue dots located above the terrain peaks. For generation of terrain maps, the number of neighbors was 40 and Pearson squared was used as the measure of distance for co-regulated genes
Disease-specific IFN-γ imprints in SLE and RA monocytes
Although IFN-γ-regulated genes in SLE and RA were characterized by a lower absolute number of differentially expressed probe sets as compared with IFN-α2a, the IFN-γ-regulated genes identified in SLE and RA were similar to those identified as IFN-α2a-regulated genes (Fig. 5a–j). There were a few SLE and RA patients that did not exhibit an IFN-γ imprint, and these patients were also negative for an IFN-α2a imprint (Fig. 5a, e).
Disease-modulated IFN-γ responses in SLE and RA monocytes. a A total of 425 differentially expressed probe sets obtained after in vitro stimulation by IFN-γ were also identified in SLE monocytes, and they were used for HC analysis of SLE and ND samples. b The same 425 probe sets as in (a) were selected from the in vitro-generated IFN-γ reference signature and arranged in the same order as identified by HC of SLE and ND in (a). c In total, 425 probe sets that were presented by hierarchical clustering in (a) were used for PAM analysis of identical SLE and ND samples. d The same 425 probe sets as in (a), (b), and (c) were utilized for PAM analysis of testing samples, which represented an independent cohort of SLE patients. e A total of 297 differentially expressed probe sets obtained after in vitro stimulation by IFN-γ were also identified in RA monocytes, and they were used for HC analysis of RA and ND samples. f The same 297 probe sets as in (e) were selected from the in vitro-generated IFN-γ reference signature and arranged in the same order as identified by HC of RA and ND in (e). g In total, 297 probe sets that were presented by hierarchical clustering in (e) were used for PAM analysis of identical RA and ND samples. h The same 297 probe sets as in (e), (f), and (g) were utilized for PAM analysis of testing samples, which represented an independent cohort of RA patients. i In total, 618 probe sets determined IFN-γ imprints in SLE and RA and they were used for HC of SLE, RA, and ND samples. Among 618 probe sets, 425 and 297 probe sets were related to IFN-γ imprint in SLE and RA, respectively, and 104 probe sets were shared between them. j The same 618 probe sets as in (i) were selected from the in vitro-generated IFN-γ reference signature and arranged in the same order as identified by HC of SLE, RA, and ND in (i). SLE patients, RA patients, and ND were colored in yellow, red, and gray, respectively. IFN-γ and unstimulated samples were colored in light blue and gray, respectively
These results could be confirmed by PAM analysis (Fig. 5c, d, g, and h). In total, 425 and 297 probe sets, which determined the IFN-γ imprints in SLE and RA, were used for classification. Different from the results obtained by PAM analysis for IFN-α2a-regulated genes in SLE, two healthy donors, ND14 and ND114, were classified as SLE patients. These two healthy donors also showed a weak IFN-γ response by hierarchical clustering (Fig. 5a, b).
Functional annotation of IFN-γ-regulated genes in SLE and RA, determined by IPA, identified different molecular networks. For instance, the network that characterized SLE contained genes such as STAT1, STAT3, IFI16, IRF7, CXCL10, and TNFSF10. In contrast, the network that displayed an IFN-γ imprint in RA contained genes such as CCL3, CCL4, CXCR4, and ATF3 (Supplementary Fig. 6a, b).
As expected, IPA identified the IFN signaling pathway, which includes both types I and II IFNs, as a pathway that was significantly altered in SLE (Supplementary Table 4). Genes included in this pathway were up-regulated both by IFN-α2a or IFN-γ (Fig. 6a). In RA, IPA showed that the IFN signaling pathway was also modulated, but in this case, genes like STAT1, MX1, IFIT1, IFIT3, and OAS1 were identified as down-regulated (Fig. 6b). A detailed analysis of these down-regulated genes revealed that TNF-α was able to silence their expression, which implicated that these genes were part of TNF-α imprint found in RA.
IFN-α/β and IFN-γ signaling pathways identified by IPA in SLE and RA monocytes were modulated in opposite directions. a IFN-α/β and IFN-γ pathways were positively triggered in SLE monocytes. However, b shows that these pathways were rather silenced in RA monocytes, as revealed by decreased expression of STAT1, MX1, OAS1, IFIT1, and IFIT3. Up- and down-regulated genes were shaded in red and green, respectively
Genes regulated by IFN-α2a and IFN-γ were found to be very similar, and thus, the terrain maps that represent IFN-γ-regulated genes in SLE and RA resembled maps that displayed IFN-α2a-regulated genes in these diseases (Supplementary Fig. 7a, b).
Disease-dependent imprint of TNF-α in SLE and RA monocytes
The in vitro-induced TNF-α signature was compared with profiles from SLE and RA patients, where 303 and 397 probe sets were identified as commonly regulated, respectively. The TNF-α imprint in SLE included up-regulation of the following genes: ALCAM, C3AR1, LYN, MYC, REL, TCF7L2, TLR2, and NFKBIA. Down-regulation of genes was also a part of TNF-α imprint in SLE, and it included genes such as BAX, CD1D, FLT3, HDAC1, KLF10, LILRA2, NCOA3, NR4A2, and PDGFC. Hierarchical clustering of TNF-α-regulated genes in SLE allowed a discrimination of all SLE patients from normal donors (Fig. 7a, b).
Disease-specific patterns of TNF-α-regulated genes in SLE and RA monocytes. a A total of 303 differentially expressed probe sets obtained after in vitro stimulation by TNF-α were also identified in SLE monocytes, and they were used for HC analysis of SLE and ND samples. b The same 303 probe sets as in (a) were selected from the in vitro-generated TNF-α reference signature and arranged in the same order as identified by HC of SLE and ND in (a). C In total 303 probe sets that were presented by hierarchical clustering in (a) were used for PAM analysis of identical SLE and ND samples. d The same 303 probe sets as in (a), (b), and (c) were utilized for PAM analysis of testing samples, which represented an independent cohort of SLE patients. e A total of 397 differentially expressed probe sets obtained after in vitro stimulation by TNF-α were also identified in RA monocytes, and they were used for HC analysis of RA and ND samples. f The same 397 probe sets as in (e) were selected from the in vitro-generated TNF-α reference signature and arranged in the same order as identified by HC of RA and ND in (e). g In total, 397 probe sets that were presented by hierarchical clustering in (e) were used for PAM analysis of identical RA and ND samples. h The same 397 probe sets as in (e), (f), and (g) were utilized for PAM analysis of testing samples, which represented an independent cohort of RA patients. i In total, 608 probe sets determined TNF-α imprints in SLE and RA, and they were used for HC of SLE, RA, and ND samples. Among the 608 probe sets, 303 and 397 probe sets were related to TNF-α imprint in SLE and RA, respectively and 92 probe sets were shared between them. j Here, the same 608 probe sets as in (i) were selected from the in vitro-generated TNF-α reference signature and arranged in the same order as identified by HC of SLE, RA, and ND in (i). SLE patients, RA patients, and ND were colored in yellow, red, and gray, respectively. TNF-α and unstimulated samples were colored in green and gray, respectively
The probe sets that determined the TNF-α imprint in SLE were used for PAM analysis. All patients were classified as SLE. The TNF-α imprint was used for classification of five additional SLE patients. In total, four out of five patients were classified as SLE (Fig. 7c, d).
The TNF-α imprint in RA included up-regulation of the following genes: ATF4, BCL6, CXCL2, EREG, IL8, NFKB2, PLAUR, SPI1, STAB1, TNF, and TNFAIP3. It also included down-regulation of genes, such as CD164, HDAC9, HHEX, IRF2, ITGA4, OAS1, OAS2, STAT1, TLR4, and TLR8. The imprint of TNF-α was not present in all RA patients, suggesting that RA patients might be sub-classified in groups with and without the TNF-α imprint (Fig. 7e, f).
PAM classification of RA patients by 397 probe sets, which determined a TNF-α imprint in RA, revealed six out of eight patients as being RA (Fig. 7g). Four additional RA patients were utilized as test samples and a TNF-α imprint was identified in two out of four patients (Fig. 7h).
The disease-specific nature of TNF-α imprints became apparent by analyzing all TNF-α-regulated genes in SLE and RA together by hierarchical clustering (Fig. 7i, j). A TNF-α imprint was identified in all SLE patients and in a sub-group of RA patients. A sub-group of RA patients, RA1, RA2, RA3, RA5, and RA7, revealed a TNF-α imprint that was characterized by a larger number of differentially expressed probe sets. The quantification of the RA-specific TNF-α imprint in each individual RA and SLE patient identified this imprint as being very strong in RA1, RA2, and RA3 and as being weaker in RA5 and RA6 (Supplementary Fig. 4c). As expected, SLE patients were negative or only weakly positive for the RA-specific TNF-α imprint.
An additional characteristic of the TNF-α imprint in RA was its obvious counteracting effect on typical IFN-α/γ-induced genes. For example, down-regulation of IFIT1, IFI44, IFI44L, OAS1, OAS2, and STAT1 emphasized the dominance of TNF-α over IFN-α/γ in RA.
Upon analyses by IPA, TNF-α-regulated genes in SLE were revealed to fit within a molecular network characterized by the transcription factors MYC, TCF7L2, CIITA, NR4A2, and EGR1. In contrast, the TNF-α imprint in RA was characterized by a molecular network composed of TNF-α, and the transcription factors MAFF, KLF6, and SPI1 (Supplementary Fig. 8a, b).
The terrain map revealed TNF-α-regulated genes as uniformly distributed within SLE and RA profiles and without preferences for dominant clustering (Supplementary Fig. 9a, b).
The absolute number of probe sets that determined the imprints of TNF-α, IFN-α2a, and IFN-γ in SLE and RA were shown in Supplementary Fig. 10a, b.
Promoter analysis revealed distinctive transcriptional programs induced in SLE and RA monocytes
We performed a whole-genome rVISTA analysis for the identification of transcription factor binding sites (TFBSs), which were statistically over-represented in regions 1 kb upstream of the transcriptional start sites. All genes that constitute SLE and RA gene expression profiles were included in this analysis (1,853 probe sets from SLE and 1,627 probe sets from RA profiles, as described in the Supplementary electronic material). Both common and specific TFBSs were identified within the promoter regions of SLE and RA profiles. In total, 42 TFBSs for SLE and 59 TFBSs for RA were identified (Supplementary Table 5, WS1). Therefore, we can speculate that different transcription factors are responsible for driving gene expression in SLE and RA monocytes in dissimilar manners. For example, TFBSs for interferon-stimulated response element (ISRE), EGR1 and EGR2 were specific for the SLE profile while TFBSs for ATF3, CREBP1, and CREPB1CJUN were restricted to the RA profile.
Promoter analysis was also performed for the genes that composed the IFN-α2a, IFN-γ, and TNF-α imprints in SLE and RA monocytes. These results revealed that TFBSs for STAT1 and ISRE, which binds the transcription factor complex that contains STAT1, were present only within the promoter regions of IFN-regulated genes in SLE. In contrast, TFBSs for ATF3 and CREPB1CJUN were detectable exclusively within the promoter regions of IFN-regulated genes in RA (Supplementary Table 5, WS2–4).
Discussion
In this study, monocyte-specific gene expression profiles from RA and SLE patients were generated, and the analysis was focused on estimating cytokine-specific imprints in these autoimmune diseases. RA and SLE gene expression profiles were identified as being disease specific, where the RA profile was able to disclose a high degree of heterogeneity between patients. To analyze SLE and RA profiles in more detail, we generated cytokine reference signatures following monocytes stimulation in vitro by TNF-α, IFN-α2a, and IFN-γ. A comparison between disease specific and in vitro-generated signatures revealed that the monocyte profile in SLE was predominantly shaped by IFNs while the RA profile was mainly patterned by TNF-α. However, the cytokine imprints in these diseases were obviously much more complex than expected, considering the fact that IFNs and TNF-α responses were also identified in RA and SLE, respectively. Remarkably, IFNs and TNF-α responses in these two rheumatic diseases were shown to be disease dependent, and they exhibited quantitative and qualitative differences. In addition, it seems reasonable to assume that the appearance of disease-specific cytokine imprints can be used to sub-stratify SLE and RA patients.
We performed a comprehensive analysis of the in vitro-generated signatures induced by TNF-α and IFNs. This analysis suggested that transcriptional changes induced by cytokines are interconnected under chronic inflammatory conditions. The cytokine responses were characterized by thousands of differentially expressed genes, which were categorized as cytokine shared, cytokine predominant, and cytokine specific.
Regarding IFN-α2a and IFN-γ stimulation, very similar gene expression profiles were observed in monocytes, although both cytokines act via binding to different receptors: IFNAR and IFNGR, respectively. However, both types of receptors are able to activate the JAK-STAT signaling cascade and to regulate the expression of interferon-stimulated genes (ISGs) [26]. While type I IFN preferentially activates the trimeric IFN-stimulated gene factor 3 (ISGF3, composed of phosphorylated STAT1 and STAT2 and unphosphorylated IRF9), IFN-γ favors activation of STAT1 homodimers. Furthermore, both types of IFNs are also able to activate gene expression by alternative pathways and independently of STAT1 [27, 28]. Therefore, the wide overlap between types I and II IFN responses suggested that the type I IFN signature was less specific than previously taught.
Direct comparison of in vitro-generated IFN-α2a and IFN-γ reference signatures with disease-specific profiles revealed IFN-shared and IFN-α2a/IFN-γ-specific responses in monocytes from SLE and RA patients. It was apparent that IFN signatures in these two diseases only partially overlapped. Genes such as IFI44, IFI44L, IFIH1, MX1, OAS1, OAS2, and STAT1, which were already described as type I IFN genes in PBMCs of SLE patients, were also identified in our study as a classical type I IFN response in monocytes from SLE patients [8, 12]. Furthermore, terrain maps showed IFN-regulated genes in monocytes from SLE patients as a group of co-expressed genes that dominated the disease. Considering the comprehensive in vitro-generated IFN profiles, it was obvious that RA monocytes also exhibited the IFN imprint. Nevertheless, it was mainly characterized by a separate set of genes that was not shared by the classical type I IFN signature in SLE. For example, STAT1 and its co-expressed genes were not dominant in RA. However, it is known that genes, such as ATF3, CCL3, CCL4, EGR2, FOSL2, JUN, PIM1, SOCS3, and ZFP36 are regulated by IFN-γ but independent of STAT1 [29, 30]. In our study, we showed that these genes constituted the IFN imprint in RA, which was regulated in a STAT1-independent manner. A substantial number of genes up-regulated by IFN in SLE were identified as down-regulated in RA, including IFI44, IFI44L, IFIT1, IFIT5, OAS1, OAS2, OAS3, and STAT1. Notably, these genes were suppressed by TNF-α what indicates for a more dominant role of TNF-α in RA. Thus, inversely regulated genes are helpful for estimating the balance between IFNs and TNF-α in SLE and RA. Interestingly, this pattern of genes was also reported to be up-regulated after anti-TNF-α therapy in SOJIA and RA patients [10, 15]. Based on our data, these results can be explained in a way that neutralization of TNF-α in these patients favors the up-regulation of genes, which were previously silenced by TNF-α.
So far, mostly PBMCs have been used for genome-wide expression analyses in SLE, RA, dermatomyositis, and SOJIA [6–8, 10]. A prototypical type I IFN signature has been identified for the first time in PBMCs from SLE patients [8]. The type I IFN signature was initially described as a pattern composed of 14 genes, which was later extended to 22 genes [7, 8, 12, 31]. It is necessary to mention that from the initial description of in vitro-generated IFN signature, consisting of 286 genes, only a small number of these genes was also identified in SLE [8, 12]. Those genes originally identified in SLE are the only genes that are considered as type I IFN imprint. In other studies, only these genes have been used to determine a possible IFN imprint in diseases such as dermatomyositis, RA patients, and diabetes [7, 9, 10, 13, 15]. Nevertheless, the IFN imprint in these diseases was different to that identified in SLE [7–10, 12, 13, 15]. Recently, it has been shown that a type I IFN signature was also apparent in patients with active tuberculosis [14]. However, based on the extensive overlap between IFN-α2a- and IFN-γ-regulated genes shown in our study, we should be cautious to consider IFN-regulated genes in rheumatic diseases, tuberculosis and generally in infectious diseases as exclusively type I IFN regulated.
Our study has demonstrated that IFN signatures in monocytes completely recapitulate the currently published IFN genes and strongly implies that monocytes are important players in shaping IFN profiles within PBMCs. Since, receptors for types I and II IFNs are widely expressed, there is no doubt that other leukocyte subsets will also respond to these cytokines [27, 28]. However, based on a rapid turnover of monocytes in circulation and their unique position in immunity, as a cell type that is placed on the cross-road between innate and adaptive immunity, monocytes possess the capacity to act as “biosensors” for the detection of inflammatory immune responses [19]. For an unambiguous cellular allocation of transcriptional responses detected in SLE and RA patients, every particular cell type including T cell and their subsets, B cell, NK, and NKT cells has to be analyzed separately”.
By whole genome rVISTA analysis, we could identify different TFBSs in the promoter regions of genes that composed SLE and RA profiles. The identified TFBSs indicate that distinct transcriptional programs, characterized by a different interplay of transcription factors, drive the pathogenesis of SLE and RA. A promoter analysis of the IFN imprints in SLE and RA identified TFBS for STAT1 only in SLE monocytes. Furthermore, the promoter analysis of IFN imprint in SLE disclosed a lower number of TFBSs as compared with those in RA, which suggests a more uniform transcriptional control. This was confirmed by terrain map analysis, since SLE profile was displayed by a dominant group of co-expressed genes composed of IFN-regulated genes. The expression of those typical IFN-regulated genes was mainly guided by transcription factor STAT1 [27, 32]. The promoter analysis of the IFN imprint in RA revealed a larger number of TFBSs. Since, the terrain map of RA profile showed many groups of co-expressed genes, it is more likely that the gene expression in each of these groups was guided by different transcriptional program. TFBSs for ATF3, CREB1 and CREB1JUN were identified only in RA. It has been shown that these transcription factors were induced by IFN [28, 33, 34]. Since, the TNF-α-response in RA caused a down-regulation of STAT1, we determined that the IFN-α2a/IFN-γ imprints in RA were rather regulated in a STAT1-independent manner.
The involvement of TNF-α, IFN-α2a, or IFN-γ in the pathogenesis of SLE and RA has been reported, but the detailed molecular effects of these cytokines in monocytes have been analyzed in this study for the first time [2, 35, 36]. Monocyte transcriptomes showed that the response to the same cytokine predominantly depends on the disease-specific inflammatory milieu. Although TNF-α, types I and II IFNs imprints were detected both in SLE and RA patients, their influence in shaping disease profiles were dissimilar. The knowledge about cytokine-regulated genes in a particular disease offers a unique opportunity for a selection of biomarkers relevant for clinical diagnosis and patient stratification, particularly for SLE and RA, which are known to be complex heterogeneous rheumatic disorders. Because, an increasing number of anti-cytokine drugs have been approved for clinical applications in the last decade, the knowledge generated from cell type-specific and cytokine-specific transcriptomes will be indispensable for patient sub-stratification and for identifying the best cytokine target for therapeutic interventions.
References
Marrack P, Kappler J, Kotzin BL (2001) Autoimmune disease: why and where it occurs. Nat Med 7:899–905. doi:10.1038/90935
Ronnblom L, Elkon KB (2010) Cytokines as therapeutic targets in SLE. Nat Rev Rheumatol 6:339–347. doi:10.1038/nrrheum.2010.64
McInnes IB, Schett G (2007) Cytokines in the pathogenesis of rheumatoid arthritis. Nat Rev Immunol 7:429–442
Aringer M, Smolen JS (2008) The role of tumor necrosis factor-alpha in systemic lupus erythematosus. Arthritis Res Ther 10:202. doi:10.1186/ar2341
Burmester GR, Haupl T (2004) Strategies using functional genomics in rheumatic diseases. Autoimmun Rev 3:541–549
Batliwalla FM, Baechler EC, Xiao X, Li W, Balasubramanian S, Khalili H, Damle A, Ortmann WA, Perrone A, Kantor AB et al (2005) Peripheral blood gene expression profiling in rheumatoid arthritis. Genes Immunol 6:388–397
Baechler EC, Bauer JW, Slattery CA, Ortmann WA, Espe KJ, Novitzke J, Ytterberg SR, Gregersen PK, Behrens TW, Reed AM (2007) An interferon signature in the peripheral blood of dermatomyositis patients is associated with disease activity. Mol Med 13:59–68
Baechler EC, Batliwalla FM, Karypis G, Gaffney PM, Ortmann WA, Espe KJ, Shark KB, Grande WJ, Hughes KM, Kapur V et al (2003) Interferon-inducible gene expression signature in peripheral blood cells of patients with severe lupus. Proc Natl Acad Sci U S A 100:2610–2615
van der Pouw Kraan TC, Wijbrandts CA, van Baarsen LG, Voskuyl AE, Rustenburg F, Baggen JM, Ibrahim SM, Fero M, Dijkmans BA, Tak PP et al (2007) Rheumatoid arthritis subtypes identified by genomic profiling of peripheral blood cells: assignment of a type I interferon signature in a subpopulation of patients. Ann Rheum Dis 66:1008–1014. doi:10.1136/ard.2006.063412
Palucka AK, Blanck JP, Bennett L, Pascual V, Banchereau J (2005) Cross-regulation of TNF and IFN-alpha in autoimmune diseases. Proc Natl Acad Sci U S A 102:3372–3377. doi:10.1073/pnas.0408506102
Batliwalla FM, Li W, Ritchlin CT, Xiao X, Brenner M, Laragione T, Shao T, Durham R, Kemshetti S, Schwarz E et al (2005) Microarray analyses of peripheral blood cells identifies unique gene expression signature in psoriatic arthritis. Mol Med 11:21–29
Baechler EC, Gregersen PK, Behrens TW (2004) The emerging role of interferon in human systemic lupus erythematosus. Curr Opin Immunol 16:801–807
Reynier F, Pachot A, Paye M, Xu Q, Turrel-Davin F, Petit F, Hot A, Auffray C, Bendelac N, Nicolino M et al (2010) Specific gene expression signature associated with development of autoimmune type-I diabetes using whole-blood microarray analysis. Genes Immunol 11:269–278. doi:10.1038/gene.2009.112
Berry MP, Graham CM, McNab FW, Xu Z, Bloch SA, Oni T, Wilkinson KA, Banchereau R, Skinner J, Wilkinson RJ et al (2010) An interferon-inducible neutrophil-driven blood transcriptional signature in human tuberculosis. Nature 466:973–977. doi:10.1038/nature09247
van Baarsen LG, Wijbrandts CA, Rustenburg F, Cantaert T, van der Pouw Kraan TC, Baeten DL, Dijkmans BA, Tak PP, Verweij CL (2010) Regulation of IFN response gene activity during infliximab treatment in rheumatoid arthritis is associated with clinical response to treatment. Arthritis Res Ther 12:R11. doi:10.1186/ar2912
Lyons PA, McKinney EF, Rayner TF, Hatton A, Woffendin HB, Koukoulaki M, Freeman TC, Jayne DR, Chaudhry AN, Smith KG (2010) Novel expression signatures identified by transcriptional analysis of separated leucocyte subsets in systemic lupus erythematosus and vasculitis. Ann Rheum Dis 69:1208–1213. doi:10.1136/ard.2009.108043
Gruetzkau A, Radbruch A (2008) Separation of whole blood cells and its impact on gene expression. In: Bosio A, Gerstmeyer B (eds) Microarrays in Inflammation. Birkhaeuser Verlag, Basel, pp 31–40
Grutzkau A, Grun J, Haupl T, Burmester GR, Radbruch A (2007) Gene expression in inflammatory rheumatic diseases. Dtsch Med Wochenschr 132:1888–1891. doi:10.1055/s-2007-984982
Gordon S, Taylor PR (2005) Monocyte and macrophage heterogeneity. Nat Rev Immunol 5:953–964
Kinne RW, Stuhlmuller B, Burmester GR (2007) Cells of the synovium in rheumatoid arthritis. Macrophages. Arthritis Res Ther 9:224. doi:10.1186/ar2333
Jiang N, Reich CF 3rd, Pisetsky DS (2003) Role of macrophages in the generation of circulating blood nucleosomes from dead and dying cells. Blood 102:2243–2250. doi:10.1182/blood-2002-10-3312
Biesen R, Demir C, Barkhudarova F, Grun JR, Steinbrich-Zollner M, Backhaus M, Haupl T, Rudwaleit M, Riemekasten G, Radbruch A et al (2008) Sialic acid-binding Ig-like lectin 1 expression in inflammatory and resident monocytes is a potential biomarker for monitoring disease activity and success of therapy in systemic lupus erythematosus. Arthritis Rheum 58:1136–1145. doi:10.1002/art.23404
Stuhlmuller B, Haupl T, Hernandez MM, Grutzkau A, Kuban RJ, Tandon N, Voss JW, Salfeld J, Kinne RW, Burmester GR (2010) CD11c as a transcriptional biomarker to predict response to anti-TNF monotherapy with adalimumab in patients with rheumatoid arthritis. Clin Pharmacol Ther 87:311–321. doi:10.1038/clpt.2009.244
Smiljanovic B, Grun JR, Steinbrich-Zollner M, Stuhlmuller B, Haupl T, Burmester GR, Radbruch A, Grutzkau A, Baumgrass R (2010) Defining TNF-alpha- and LPS-induced gene signatures in monocytes to unravel the complexity of peripheral blood transcriptomes in health and disease. J Mol Med 88:1065–1079. doi:10.1007/s00109-010-0648-8
Kim SK, Lund J, Kiraly M, Duke K, Jiang M, Stuart JM, Eizinger A, Wylie BN, Davidson GS (2001) A gene expression map for Caenorhabditis elegans. Science 293:2087–2092. doi:10.1126/science.1061603
Der SD, Zhou A, Williams BR, Silverman RH (1998) Identification of genes differentially regulated by interferon alpha, beta, or gamma using oligonucleotide arrays. Proc Natl Acad Sci U S A 95:15623–15628
van Boxel-Dezaire AH, Rani MR, Stark GR (2006) Complex modulation of cell type-specific signaling in response to type I interferons. Immunity 25:361–372. doi:10.1016/j.immuni.2006.08.014
van Boxel-Dezaire AH, Stark GR (2007) Cell type-specific signaling in response to interferon-gamma. Curr Top Microbiol Immunol 316:119–154
Ramana CV, Gil MP, Han Y, Ransohoff RM, Schreiber RD, Stark GR (2001) Stat1-independent regulation of gene expression in response to IFN-gamma. Proc Natl Acad Sci U S A 98:6674–6679. doi:10.1073/pnas.111164198
Gil MP, Bohn E, O'Guin AK, Ramana CV, Levine B, Stark GR, Virgin HW, Schreiber RD (2001) Biologic consequences of Stat1-independent IFN signaling. Proc Natl Acad Sci U S A 98:6680–6685. doi:10.1073/pnas.111163898
Bauer JW, Baechler EC, Petri M, Batliwalla FM, Crawford D, Ortmann WA, Espe KJ, Li W, Patel DD, Gregersen PK et al (2006) Elevated serum levels of interferon-regulated chemokines are biomarkers for active human systemic lupus erythematosus. PLoS Med 3:e491
Ramana CV, Gil MP, Schreiber RD, Stark GR (2002) Stat1-dependent and -independent pathways in IFN-gamma-dependent signaling. Trends Immunol 23:96–101
Zhao LJ, Hua X, He SF, Ren H, Qi ZT (2011) Interferon alpha regulates MAPK and STAT1 pathways in human hepatoma cells. Virol J 8:157. doi:10.1186/1743-422X-8-157
Taylor MW, Grosse WM, Schaley JE, Sanda C, Wu X, Chien SC, Smith F, Wu TG, Stephens M, Ferris MW et al (2004) Global effect of PEG-IFN-alpha and ribavirin on gene expression in PBMC in vitro. J Interferon Cytokine Res 24:107–118. doi:10.1089/107999004322813354
Karonitsch T, Feierl E, Steiner CW, Dalwigk K, Korb A, Binder N, Rapp A, Steiner G, Scheinecker C, Smolen J et al (2009) Activation of the interferon-gamma signaling pathway in systemic lupus erythematosus peripheral blood mononuclear cells. Arthritis Rheum 60:1463–1471. doi:10.1002/art.24449
Feldmann M (2002) Development of anti-TNF therapy for rheumatoid arthritis. Nat Rev Immunol 2:364–371. doi:10.1038/nri802
Acknowledgments
We are grateful to Heidi Schliemann for generating the gene expression data and to Dr. Hans-Joachim Mollenkopf for valuable discussion.
Funding source
The work was supported by the German Ministry of Education and Research (BMBF) within the National Genome Research Network NGFN (01GS0413) and ArthroMark (01EC1009A), by the European Union’s Sixth Framework Programme (project AutoCure; LSHB-CT-2006-018861), and by the IMI JU funded project BeTheCure, contract no 115142-2.
Authorship
Conceived and designed the research: AG, AR, BS, TH, WM, RBa, GRB. Performed research: BS, AG, RB. Analyzed data: BS, AG, RBa, JG, USW, TH, FH, BSt. Wrote the paper: BS, AG, TH.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Smiljanovic, B., Grün, J.R., Biesen, R. et al. The multifaceted balance of TNF-α and type I/II interferon responses in SLE and RA: how monocytes manage the impact of cytokines. J Mol Med 90, 1295–1309 (2012). https://doi.org/10.1007/s00109-012-0907-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-012-0907-y