Abstract
Accurate hemodynamic and intravascular volume status assessment is essential in the diagnostic and therapeutic management of critically ill patients. Over the last two decades, a number of technological advances were translated into a variety of minimally invasive or non-invasive hemodynamic monitoring modalities. Despite the promise of less invasive technologies, the quality, reliability, reproducibility, and generalizability of resultant hemodynamic and intravascular volume status data have been lacking. Since its formal introduction, ultrasound technology has provided the medical community with a more standardized, higher quality, broadly applicable, and reproducible method of accomplishing the above-mentioned objectives. With the advent of portable, hand-carried devices, the importance of sonography in hemodynamic and volume status assessment became clear. From basic venous collapsibility and global cardiac assessment to more complex tasks such as the assessment of cardiac flow and tissue Doppler signals, the number of real-life indications for sonology continues to increase. This review will provide an outline of the essential ultrasound applications in hemodynamic and volume status assessment, focusing on evidence-based uses and indications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hemodynamic monitoring of the intensive care unit (ICU) patient has taken many forms as medical technologies continue to evolve. The current tools for estimating intravascular volume status range from invasive to non-invasive methods, including central venous pressure (CVP) monitors, pulmonary artery catheters (PAC), esophageal Doppler, transesophageal echocardiography, transthoracic echocardiography, impedance plethysmography, and arterial pressure waveform analysis [1–4]. Vincent et al. [5] outlined the desired characteristics of an ideal hemodynamic monitoring system, including the following: (a) measurements are clinically relevant; (b) information provided is accurate and reproducible; (c) data are interpretable; (d) technology is easy to use and readily available; (e) device is operator independent; (f) there is a rapid response time; (g) technology is cost-effective and causes no harm; and (h) information generated is able to guide therapy. Ultrasound is a modality which most closely fits this idealized description. Not surprisingly, hemodynamic assessment and volume status monitoring with ultrasound have gradually emerged as a leading method in the management of critically ill patients [6–12]. The attractiveness of ultrasound is primarily based on its non-invasiveness and versatility [13, 14]. In this article, we review the most common applications of ultrasound in hemodynamic monitoring and provide a framework for its potential applications in the future. It is not our intent to review each pertinent ultrasound technique in detail; rather, it is our goal to create a repository for the sonographer that can be used as a reference source for further clinical learning and research in this important topic area.
Ultrasound: the perfect clinical tool for hemodynamic and volume status assessment
Estimation of intravascular volume status and cardiac function has traditionally posed a challenge for clinicians in the ICU setting [1]. The ideal hemodynamic monitoring system should be able to measure clinically relevant variables, be able to acquire accurate, be reproducible, and resultant data to be interpretable, easy to use, readily available, and operator independent [5]. Any potential harm to the patient should be minimal and response time should be rapid [5]. Other than its operator-dependent nature, ultrasound fulfills almost all of the desired criteria for an optimal clinical tool for evaluating hemodynamic and intravascular volume status.
The advent of intensivist bedside ultrasonography (INBU) for volume assessment has enhanced our ability to assess the intravascular volume status of patients in a variety of clinical settings [1, 6, 15]. In general, INBU utilization in hemodynamic monitoring can be regarded as a subset of point-of-care ultrasonography, defined as sonography performed and interpreted by the clinician at the bedside [16]. The ability for the bedside clinician to acquire ultrasonic images and to subsequently interpret these images toward a goal of implementing treatment-modifying decisions is pivotal in the intensive care setting. This process is exemplified by the I-AIM methodology proposed by Bahner et al. [17], where the key components of clinician-driven, point-of-care diagnosis and treatment include indication, acquisition, interpretation, and medical decision making. Using I-AIM, any clinician equipped with bedside ultrasound technology is empowered to interpret sonographic images in real-time [17]. A general outline of sonography-based techniques for hemodynamic monitoring and intravascular volume assessment is shown in Table 1.
Overview of general ultrasound applications in hemodynamic and volume status assessment
Although the genesis of medical ultrasonography can be traced back to the early 20th Century, it was not until the 1990s that sonography was able to gain acceptance at the patient’s bedside [16, 18]. Point-of-care ultrasonography has since expanded to include procedural, diagnostic, and screening applications in a wide range of specialties [18–23]. Procedural guidance as in central line placement [24, 25], diagnostic assessment as in the Focused Assessment with Sonography in Trauma (FAST) [26–28], thoracic cavitary ultrasonography to assess for pleural effusion, pneumothorax, or pneumonia [29, 30], verification of tracheal airway placement [18], musculoskeletal diagnosis and treatment [14], cardiovascular applications [11, 12, 31], and gynecological screening [32, 33] are now all commonplace in the clinical arena. New applications of ultrasound are presently being explored in the realms of thermal tumor ablation, hemorrhage control, nanotechnology, fracture healing, and noncontact wound therapy [34–39].
Overview of ultrasound in hemodynamic and volume status assessment
Venous collapsibility measurements
Accurate and timely estimation of intravascular volume status is a critical component of the management of critically ill patients. Invasively placed lines may lead to a variety of complications, and the sonographic assessment of the venous collapsibility index (VCI, Fig. 1) is being increasingly recognized as potential replacement or at least an attractive adjunctive modality to traditional methods [4, 40, 41]. This index measures the fractional change in major venous diameters through the respiratory cycle rather than relying on a single measurement of venous diameter [6, 15, 42, 43]. This, in turn, provides internal “standardization” of vessel diameter-derived hemodynamic information. The field of functional hemodynamic monitoring is actively emerging, and despite early skepticism, evidence suggests that dynamic assessment of the change in venous diameter during the respiratory cycle offers a number of unique advantages over the static, single-measurement approach [1, 42]. Although VCI is not without important limitations [44], there seems to be a reasonable correlation between sonographic and traditional markers of intravascular volume status (Table 2), especially when temporal trends are taken into consideration [6, 40].
Demonstration of inferior vena cava (IVC) collapsibility. In this example, the difference between maximum IVC diameter (left, large arrow) and the minimum IVC diameter (right, small arrow) is >50 %, indicating relatively “low” volume status. Lack of collapsibility, on the other hand, is more suggestive of euvolemia or hypervolemia. Note that the two intermediate images show relatively stable IVC diameter during the mid-portion of the respiratory cycle
Among more recent developments for VCI, the most significant findings include the demonstration that the subclavian vein collapsibility (SCV-CI) fairly well approximates the inferior vena cava collapsibility (IVC-CI) [43]. This, in turn, provides alternative options for estimating VCI when the “gold standard” IVC-CI is unobtainable (i.e., due to patient factors such as morbid obesity or surgical dressings). Although a learning curve is clearly present for both SCV-CI and IVC-CI, the difficulty of these bedside assessments is not prohibitive. In addition to providing a potential alternative to IVC-CI, the subclavian vein-based assessment takes less time than the vena cava assessment according to one preliminary study [43].
There is also growing increasing evidence that venous collapsibility is indeed inversely related to the central venous pressure [6, 7]. Within that very domain, increasing granularity of data measurements allows us to define such relationship at a unitary level. For example, every 1-mm Hg change in CVP correlates with an approximate 3.3 % change in IVC collapsibility [6]. Moreover, the degree of VCI change decreases as the baseline CVP “starting point” increases [i.e., there is more change in VCI at lower CVP ranges (1–7 mmHg) than at high CVP ranges (≥8 mmHg)] [6]. Finally, the effect of positive end-expiratory pressure (PEEP) is only modest at best, dispelling the earlier dogma that VCI is only valid in spontaneously breathing, non-ventilated patients and lending support to replacing “inspiratory” versus “expiratory” venous diameters by the new paradigm of “maximum” versus “minimum” measured venous diameters when calculating collapsibility [6, 7, 15].
Regarding the learning curve for practitioners training to perform VCI assessments, the number of proctored exams needed to attain adequate proficiency is somewhere between 25 and 50 [7]. Once sufficient comfort level is achieved by a practitioner, one can expect that VCI will correlate with expert clinical judgment to the same degree as CVP approximately 67–75 % of the time [1]. It has to be noted, however, that given the relatively low level of correlation, as well as the selection of “clinical judgment” as a gold standard, the evidence presented above may leave some with more questions than answers. In addition, the relative paucity of research in the general area of ultrasonography for hemodynamic assessment highlights a number of important issues that impede more widespread acceptance of this methodology—limited penetration into the mainstream, steep learning curve and the requirement for specialized training, lack of true “gold standard” or a reliable/universal “reference point”, as well as the inherently difficult nature of designing and conducting high-quality studies.
Hemodynamic assessment techniques relying on simplified, ultrasound-based vascular measurements
In addition to the above-mentioned correlations between VCI, central venous pressures, and intravascular volume status, a number of other methods for volume status estimation have been reported. In one report, patients with a jugular vein height-to-width ratio of 0.84 or less were significantly more likely to have a CVP of <8 mmHg [45]. Additionally, inter-observer comparisons were moderately good, and the assessment could readily be performed by non-intensivists [45]. Bailey et al. [46] reported that the simultaneously measured ratio of ≥2 for jugular vein-to-common carotid artery diameter significantly correlated with a CVP of >8 mmHg in pediatric burn patients. Another investigative team found that ultrasound can be helpful in estimating jugular venous pressures [47]. However, in the latter report, both ultrasound and clinical evaluation tended to systematically underestimate the measured CVP [47]. Finally, Schefold et al. [48] demonstrated that inspiratory and expiratory vena cava diameters correlated well with intrathoracic blood volumes, PaO2/FiO2 oxygenation index, and CVP.
Focused echocardiographic determination of hemodynamic status
Manasia et al. [49] reported that intensivists are capable of conducting and accurately interpreting cardiac ultrasounds in as many as 84 % of cases. Moreover, diagnostic information gathered in these studies affected management in nearly 40 % of patients and provided clinically useful information in an additional 48 % of cases [49]. Gunst et al. [50, 51] found that a cardiac index determination using a focused cardiac exam significantly correlated with cardiac index measurements obtained by pulmonary artery catheter. Another group of intensivist sonography investigators published preliminary data correlating the relationship between cardiac pulsed-wave Doppler and tissue Doppler imaging with pulmonary artery and central venous pressures [52]. Melamed et al. [53] reported that intensivists could be trained to estimate left ventricular function and perform fairly advanced cardiac sonography with as little as 6 h of instruction (Fig. 2a). However, significantly more experience is required for the sonographers performing focused exams to become both more comfortable and proficient with advanced cardiac assessment using echocardiography. Additional information on echocardiography is provided below under special topics in hemodynamic monitoring.
a Left a sample transthoracic echocardiographic view demonstrating a long-axis parasternal view (top) with m-mode recording of the aortic outflow (bottom). These images were obtained using a hand-held, point-of-care ultrasound device. This image, including sample caliper measurements, can be obtained by a medical student after approximately 4 h of didactics and 2 h of hands-on training. b Right typical appearance of the McConnell’s sign in a patient with acute pulmonary embolism on a point-of-care echocardiogram. Note the severe dilation of the right ventricle (arrow in the left upper portion of the image) and relative reversal of left-to-right ventricle ratio >1:1. The preservation of the right ventricular apical kinesis is due to an overlapping of the left ventricular fibers onto the conical right ventricle that bloats out under right heart strain and acute rise in pressure
Esophageal Doppler monitoring
Historically, the pulmonary artery catheter (PAC) was regarded as the “gold standard” in evaluating the cardiac output (CO) of the critically ill patient [54]. However, the PAC invasiveness and risk of complications (arrhythmias predominating) make it a less-than-ideal candidate in the clinician armamentarium for measuring cardiac output [4, 54]. Concurrently to the popularization of intensivist-performed, point-of-care sonography using traditional ultrasound equipment, esophageal Doppler monitoring (EDM) devices were introduced to help harness the diagnostic power of ultrasound in a much more focused and less invasive fashion. In brief, EDM probes feature a unidirectional echo-Doppler mini-probe that is positioned so as to capture blood flow characteristics within the descending aorta in real-time fashion [54–57]. A number of correlative studies, both experimental and clinical, established that there is a reasonable degree of correlation between EDM, the PAC, and transesophageal echocardiography, especially in regard to CO estimation [8, 58, 59]. Roeck et al. [60] reported on a prospective cohort of 19 intubated and sedated adult patients, showing a good correlation between EDM and the PAC. Of note, the precision between the two methods was relatively poor [60]. In another report, Hussien et al. [61] demonstrated that EDM could be used as a sole hemodynamic monitoring device during liver transplantation cases. Another uniquely suitable clinical application of the EDM is its use in the organ donor population [9, 62]. Here, many of the limitations associated with EDM use in the general intensive care population are not present, including the requirement for sedation and the associated need for frequent probe repositioning due to Doppler signal loss.
Esophageal Doppler ultrasound technology is not without limitations. Over the years, EDM became less popular due to a variety of factors that affect its applicability, including, but not limited to patient discomfort, large probe size, the need for frequent probe readjustments due to patient movement, operator dependence, as well as the need for additional sedation and analgesia due to the very presence of the above factors [8, 10]. As outlined by Schober et al. [63], the Doppler device assumes laminar blood flow in the descending aorta, but this may not be the case in patients with aortic disease. Second, the aortic cross-sectional area is measured or estimated, and the cross-section itself is not perfectly circular; this may give rise to potential inaccuracies in aortic diameter measurements [63]. Third, various pathological states may effectively redistribute the CO, thus altering CO-related EDM-derived calculations. These and other factors must be considered in the utilization of EDM in the critically ill or perioperative patient [63]. In the modern critical care unit, a number of newer, more robust alternatives to the EDM now exist, including reusable and single-use transesophageal echocardiography probes [64, 65]. This emerging technology is discussed below in the special topics section of this review.
Special topics in hemodynamic monitoring
Echocardiography
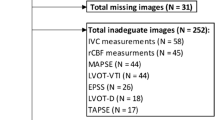
This section includes a brief discussion of echocardiography, focusing on its advantages and disadvantages in the clinical setting of hemodynamic assessment and intravascular volume monitoring. A number of different cardiac windows can be evaluated by transthoracic echocardiography [66]. However, the performance of “surface echo” can be limited by patient body habitus, cutaneous tissue edema, interference from life-saving devices, surgical dressings, or hyperinflated lungs [67–69]. Transesophageal echocardiography (TEE) is a viable alternative in select patient populations. For example, in the intubated or sedated patient, a TEE can be performed to provide a better visualization of cardiac structures [70, 71]. Specialized portable TEE devices have been described for single use [65, 72]. In well-experienced hands these tools are extremely valuable, with clinical tools available to evaluate findings such as cardiac wall motion abnormalities or valvular vegetations (Table 3).
Transthoracic echocardiography
Transthoracic echocardiography (TTE) finds its strengths in the emergency department and the ICU for the evaluation of hemodynamically unstable patients (a category I use) [73]. General indications for use of echocardiography in the ICU include (a) hemodynamic compromise, which includes ventricular function, valvular function, pericardial effusion, volume status, pulmonary embolism, and untoward surgical events; (b) unexplained hypoxemia secondary to shunt or ventricular function, and pulmonary embolism; (c) the diagnosis of infective endocarditis associated with valves and hardware; (d) suspected embolic sources such as left ventricular mural or apical thrombi, atrial thrombi or intracardiac shunts; and (e) aortic dissection diagnostics, identification of origin and type of dissection, aortic diameter, and the presence of potential sequelae of aortic dissections such as pericardial effusion and aortic regurgitation [74]. While there currently is no incontrovertible evidence showing that echocardiography-guided therapy improves outcomes, there are reports that demonstrate that the performance of echocardiography may lead to changes in therapy in as much as 50 % of cases [75, 76]. In addition, obtaining adequate image quality on transthoracic echocardiography may be technically challenging in the critically ill population (see previous section for potential limitations of echocardiography) [67–69, 77]. Consequently, transesophageal echocardiography may be required in some of the more acutely ill patients.
Transesophageal echocardiography
Transesophageal echocardiography (TEE) is a well-established diagnostic and monitoring tool in cardiac surgery for evaluation of global and valvular function along with preload, afterload, and general hemodynamic parameters, as well as demonstration of the success of surgical intervention in the operating room [71]. It is more commonly used in the intensive care setting, mainly because many critically ill patients are already sedated (i.e., requirement of TEE) and mechanically ventilated ahead of the scheduled procedure [78]. Due to its more invasive nature, clinical indications for TEE are more restrictive (i.e., failure to adequately visualize cardiac structures on TTE, need for specific information not otherwise available on TTE, etc.) [78, 79]. Compared to transthoracic echocardiography, TEE provides much better assessment not only of the heart but also of the aortic pathology (i.e., dissection) [80, 81].
Limitations and special considerations of echocardiography
Limitations of both TEE and TTE include the inability to produce continuous data. TTE for post-surgical critically ill patients may be of limited value due to difficulty in obtaining images of sufficient quality for clinical decision making. Postoperative patients often cannot be optimally positioned due to pain, with sonographic visualization frequently distorted by surgical dressings and/or drains. Many critical care physicians experienced at both TTE and TEE use TTE as the firstline modality for assessment of an unstable patient and then use TEE if the acquired images fail to provide clinically actionable information. TEE does provide higher resolution images, particularly of the posterior mediastinal structures (left atrium, distal arch, and descending aorta) but is not without risks. The reported incidence of injury secondary to TEE probe placement is approximately 1 % [82]. Furthermore, the risk of sedation and airway obstruction in patients without an endotracheal tube must be weighed against the diagnostic benefit to the patient. The risk profile of TEE may be unfavorable in patients with abnormalities of the pharynx, esophagus, and stomach.
More recently, single-use miniaturized indwelling TEE probes have been developed that can be used for up to 3 days [83]. The single-use probe is a biplane device that can assess LV filling and function, right ventricular function, and fluid responsiveness, and can acquire three primary views: the mid esophageal four-chamber view, the trans-gastric short axis, and the superior vena cava [65]. New generation of devices will feature TEE microprobe (i.e., micro-TEE) [84]. Although not yet as capable as full-feature TEE devices, micro-TEE probes can provide clinically useful images of the heart and pulmonary arteries [84]. Decreasing diameters of newer single-use and micro-TEE probes makes it possible to significantly reduce the need for procedural sedation [84] and to extend the probe indwelling time to as long as 72 h so that truly continuous data can be acquired and trends observed over time [85].
While the use of TEE is associated with more severe complications than TTE, TTE is associated with higher rates of inappropriate use with a significant increase in resultant costs [86, 87]. Appropriate use criteria (AUC) have been published in 2007 and updated in 2011 [88, 89]. There is evidence that only about one-third of TTEs result in a change of care and one-fifth result in no change of care. Attempts to reduce the use of TTE by a decrease in reimbursement have not been successful because of the increasing overall utilization of this modality [87]. Mondillo et al. [64] published an excellent overview on hand-held echocardiography, including a classification of sonographic techniques based on increasing technical difficulty and level of operator training (Fig. 3).
Future directions include hand-held and portable devices that can wirelessly interface with, and transmit sonographic images to a wide range of electronic devices (i.e., desktops, laptops, smart phones, tablets) for ease of interpretation [90]. Moreover, advanced software applications will provide decision support models that incorporate prediction horizons [91]. TEE and TTE will remain integral parts of our armamentarium in the ICU, the emergency department, and the operating room for the foreseeable future. Their indications, limitations, complications, and costs should be well known to all healthcare providers.
Pulmonary embolism
The topic of venous thromboembolism continues to pose a diagnostic dilemma. The main challenge clinicians facing today is the urgent need for better methods of quickly and reliably diagnosing pulmonary embolism (PE) and the ability to nearly immediately institute life-saving therapy [92, 93]. Historically, the “McConnell sign,” defined as right ventricular (RV) dilation (Fig. 2b) with free wall hypokinesis in the presence of normal RV apical contractility, was regarded as a pathognomonic for acute PE [94]. However, subsequent research demonstrated that disregarding the right ventricular afterload severely limited the diagnostic accuracy of the McConnell’s sign [95]. With overall sensitivity of approximately 50–80 % and specificity of about 90 %, TTE and TEE are not sufficient to make the diagnosis of PE in cases without obvious findings (i.e., clot in the right ventricle) [96, 97]. Still, there continues to be an important role for TTE in the diagnosis of acute PE, especially when the patient is not hemodynamically stable enough to be safely transported to the imaging department for definitive diagnostic testing [11, 12]. Nazeyrollas et al. [98] encourage the use of transthoracic Doppler echocardiography combined with clinical and electrocardiographic data in diagnosing acute PE. Of greater importance is the use of combined echocardiographic signs that cumulatively suggest that acute PE could be occurring [12, 99]. Moreover, there are data to support that TTE may be helpful in tracking the progress of therapeutic interventions directed at the pulmonary embolism. More specifically, the degree of right ventricular strain and other PE-associated signs tend to improve with increasing duration of definitive anticoagulation and hemodynamic support [12].
One study specifically examined echocardiographic characteristics of surgical intensive care patients who underwent TTE within 72 h of known diagnosis of PE [12]. Based on study findings, the authors of the study were able to propose the following as the most common echocardiographic findings in the study (in descending order): (a) tricuspid regurgitation; (b) pulmonary hypertension; (c) dilated right ventricle; (d) right heart strain; (e) hyperdynamic underfilled LV; and (f) septal wall motion abnormalities [12]. The greater the number of abnormal findings from the above list, the more acute and more likely was the PE. The study group also provided preliminary evidence that conducting serial TTE examinations as opposed to a single snapshot TTE for suspected PE in the ICU setting may provide additional diagnostic detail and help document the overall therapeutic response [12]. In summary, the study suggested that TTE may be a valuable diagnostic adjunct, in conjunction to high clinician suspicion of PE. Finally, the same group proposed a clinical diagnostic and treatment algorithm incorporating TTE in the setting of suspected PE [11].
Patient safety considerations
Our discussion of ultrasound technology would not be complete without a brief section on patient safety. Although a significant proportion of safety-related issues are associated with incorrect interpretation of sonographic images, a small but very real concern about ultrasound exposure exists. While there is a general agreement that ultrasound is very safe [100], it is worth mentioning that acoustic exposure levels from modern machines should be monitored to ensure patient safety. The ALARA (as low as reasonably achievable) principle should be applied during every ultrasound exposure, regardless of the low overall baseline risk profile [101, 102].
Ultrasound in hemodynamic monitoring and volume status estimation: future applications and avenues for research
Ultrasound shows great promise as a non-invasive, point-of-care modality to assess intravascular volume status and cardiac function by a variety of methods. It meets nearly all criteria for such modality as set forth by Vincent et al. [5]. While provider training and proficiency expectations should be established, most of the commonly performed ultrasound-based hemodynamic assessments do not require sonography experts [48]. Moreover, these simple point-of-care tests have been shown to affect clinical management in a significant proportion of cases [1, 103]. Given the great promise of I-AIM methodology [17] in this very context, future work should focus on demonstrating the effect of focused bedside sonography on patient outcomes. Given the increasing problem of under-staffed sonography and echocardiography units world-wide and lack of around-the-clock availability of highly trained staff, the urgent need for wider implementation of point-of-care, provider-based ultrasound testing becomes an item of great importance [104–107]. Even in locations without shortages, ultrasound studies may not be available around-the-clock or may take significant amounts of time before an ultrasound technician obtains necessary sonographic views or a radiologist issues a definitive interpretation of corresponding images.
The field of bedside ultrasonography for non-invasive intravascular volume and hemodynamic monitoring will continue to grow due to its ability to provide instantaneous clinically relevant results and very favorable risk–benefit ratio. Furthermore, most of these sonographic assessments do not require the operator to be an expert in sonography [48], and many of the skills can be learned quickly [53]. Here, the I-AIM approach to the clinician-performed ultrasound (Table 4) needs to be specifically mentioned because it spells out indications and ways to acquire images and ties them directly to well-defined patient management issues, offers study-specific training guidelines, and allows the information to be gleaned from scans to directly affect patient management. As such, this model is likely to serve as the basis for further expansion of clinician-performed ultrasound. One important limitation of current research on ultrasound in intravascular volume status monitoring is that efforts have been devoted to comparisons of sonography to other clinical techniques and standards. As more operators enter the field of point-of-care ultrasonograpy and the clinical implementation of ultrasound-based protocols increases, more research inquiries will be directed toward generating high-level, evidence-based outcome data specifically focusing on sonography.
Future directions in point-of-care ultrasound research and development are outlined in Table 5. These include the development and dissemination of hand-held devices/probes that can be carried in coat pockets and easily interfaced with smart phones and tablets, including software-based decision support models that incorporate prediction horizons [90, 108]. TEE and TTE will remain as part of our armamentarium in the ICU, emergency department, and the operating room for the foreseeable future [103, 109–111]. Specific indications, limitations, complications, and costs should be well known to providers. One last area not specifically included in this review, but certainly deserving a brief mention, is the use of bedside ultrasound in detection, follow-up, and treatment of a variety of peripheral arterial and venous conditions [112–118], including deep vein thrombosis [119, 120].
Conclusions
The modern day intensivist and emergency practitioner are faced with a variety of diagnostic, as well as therapeutic, dilemmas. Among these, accurate assessment of intravascular volume status and cardiac function continues to pose significant challenges. Despite the large amount of research and advances in this area, no one technology has emerged as the gold standard. When properly used by non-experts, ultrasound-based techniques offer an accurate, reproducible, low-risk, real-time approach for assessing intravascular volume status and cardiac function. Specific approaches utilizing ultrasound in fluid status determination include static venous measurements, venous collapsibility determination, focused transthoracic echocardiography, esophageal Doppler monitoring, and transesophageal echocardiography. The availability of real-time information on cardiac-specific parameters (i.e., preload, afterload) can help modify medical decision making. Other clinical applications for point-of-care sonographic assessment include TTE for pulmonary embolism investigation, cardiac activity/function determination, and single-use TEE devices. Although research clearly shows the cost-effectiveness of bedside sonography, more information is needed to better understand the effect of point-of-care ultrasound on patient outcomes including morbidity and mortality.
References
Carr BG, et al. Intensivist bedside ultrasound (INBU) for volume assessment in the intensive care unit: a pilot study. J Trauma. 2007;63(3):495–500 (discussion 500–2).
Eiferman DS, et al. Two methods of hemodynamic and volume status assessment in critically ill patients: a study of disagreement. J Intensive Care Med. 2014.
Bache RJ, Harley A, Greenfield JC Jr. Evaluation of thoracic impedance plethysmography as an indicator of stroke volume in man. Am J Med Sci. 1969;258(2):100–13.
Evans DC, et al. Complications associated with pulmonary artery catheters: a comprehensive clinical review. Scand J Surg. 2009;98(4):199–208.
Vincent JL, et al. Clinical review: update on hemodynamic monitoring—a consensus of 16. Crit Care. 2011;15(4):229.
Stawicki SP, et al. Prospective evaluation of intravascular volume status in critically ill patients: does inferior vena cava collapsibility correlate with central venous pressure? J Trauma Acute Care Surg. 2014;76(4):956–63 (discussion 963–4).
Stawicki SP, et al. Intensivist use of hand-carried ultrasonography to measure IVC collapsibility in estimating intravascular volume status: correlations with CVP. J Am Coll Surg. 2009;209(1):55–61.
Stawicki PS, Braslow B, Gracias VH. Exploring measurement biases associated with esophageal Doppler monitoring in critically ill patients in intensive care unit. Ann Thorac Med. 2007;2(4):148–53.
Cipolla J, Stawicki S, Spatz D. Hemodynamic monitoring of organ donors: a novel use of the esophageal echo-Doppler probe. Am Surg. 2006;72(6):500–4.
Stawicki SP, et al. Use of non-invasive esophageal echo-Doppler system in the ICU: a practical experience. J Trauma. 2005;59(2):506–7.
Stawicki SP, et al. Transthoracic echocardiography for suspected pulmonary embolism in the intensive care unit: unjustly underused or rightfully ignored? J Clin Ultrasound. 2008;36(5):291–302.
Stawicki SP, et al. Transthoracic echocardiography for pulmonary embolism in the ICU: finding the “right” findings. J Am Coll Surg. 2008;206(1):42–7.
Khasawneh FA, Smalligan RD. Focused transthoracic echocardiography. Postgrad Med. 2010;122(3):230–7.
Royall NA, et al. Ultrasound-assisted musculoskeletal procedures: a practical overview of current literature. World J Orthop. 2011;2(7):57–66.
Stawicki SP, Bahner DP. Evidence tables: inferior vena cava collapsibility index (IVC-CI). OPUS 12. Scientist. 2012;6(1):3–5.
Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749–57.
Bahner DP, Hughes D, Royall NA. I-AIM: a novel model for teaching and performing focused sonography. J Ultrasound Med. 2012;31(2):295–300.
Bahner DP, et al. What’s new in critical illness and injury science? The challenge of verifying tracheal airway placement: solving the puzzle one piece at a time. Int J Crit Illn Inj Sci. 2013;3(2):105–7.
Arslanoglu I, et al. Real-time sonography for screening of gallbladder dysfunction in children with type 1 diabetes mellitus. J Pediatr Endocrinol Metab. 2001;14(1):61–9.
Bakker J, et al. Sonography as the primary screening method in evaluating blunt abdominal trauma. J Clin Ultrasound. 2005;33(4):155–63.
Madjar H, et al. Value of high resolution sonography in breast cancer screening. Ultraschall Med. 1994;15(1):20–3.
Roll SC, et al. Screening for carpal tunnel syndrome using sonography. J Ultrasound Med. 2011;30(12):1657–67.
Youk JH, Kim EK. Supplementary screening sonography in mammographically dense breast: pros and cons. Korean J Radiol. 2010;11(6):589–93.
Fry WR, Clagett GC, O’Rourke PT. Ultrasound-guided central venous access. Arch Surg. 1999;134(7):738–40 (discussion 741).
Denys BG, et al. An ultrasound method for safe and rapid central venous access. N Engl J Med. 1991;324(8):566.
Stawicki SP, et al. Portable ultrasonography in mass casualty incidents: the CAVEAT examination. World J Orthop. 2010;1(1):10–9.
Cunningham AR. FAST scan: ultrasound’s role in trauma. Radiol Technol. 2008;79(5):455–8.
Vance S. Evidence-based emergency medicine/systematic review abstract. The FAST scan: are we improving care of the trauma patient? Ann Emerg Med. 2007;49(3):364–6.
Kartasasmita CB, Yogi A, Rosmayudi O. Pleural effusion examination by ultrasound. J Singapore Paediatr Soc. 1987;29(Suppl 1):117–9.
Chavez MA, et al. Lung ultrasound for the diagnosis of pneumonia in adults: a systematic review and meta-analysis. Respir Res. 2014;15:50.
Kobal SL, Atar S, Siegel RJ. Hand-carried ultrasound improves the bedside cardiovascular examination. Chest. 2004;126(3):693–701.
Estroff JA. Emergency obstetric and gynecologic ultrasound. Radiol Clin North Am. 1997;35(4):921–57.
Higgins RV, et al. Transvaginal sonography as a screening method for ovarian cancer. Gynecol Oncol. 1989;34(3):402–6.
McGuire J, Wood BD. Prospective advancements in ultrasound imaging. Radiol Technol. 2014;85(4):463–6.
Zhou YF. High intensity focused ultrasound in clinical tumor ablation. World J Clin Oncol. 2011;2(1):8–27.
Vaezy S, Zderic V. Hemorrhage control using high intensity focused ultrasound. Int J Hyperthermia. 2007;23(2):203–11.
Hantes ME, et al. Low-intensity transosseous ultrasound accelerates osteotomy healing in a sheep fracture model. J Bone Joint Surg Am. 2004;86-A(10):2275–82.
McAlinden MM. Fracture healing using low-intensity pulsed ultrasound. CMAJ. 2002;167(2):128 (author reply 128).
Kavros SJ, et al. Expedited wound healing with noncontact, low-frequency ultrasound therapy in chronic wounds: a retrospective analysis. Adv Skin Wound Care. 2008;21(9):416–23.
Pasquero P, et al. Inferior vena cava diameters and collapsibility index changes reveal early volume depletion in a healthy donor model. Crit Ultrasound J. 2012;4(Suppl 1):A29.
Thanakitcharu P, Charoenwut M, Siriwiwatanakul N. Inferior vena cava diameter and collapsibility index: a practical non-invasive evaluation of intravascular fluid volume in critically-ill patients. J Med Assoc Thai. 2013;96(Suppl 3):S14–22.
Cavallaro F, Sandroni C, Antonelli M. Functional hemodynamic monitoring and dynamic indices of fluid responsiveness. Minerva Anestesiol. 2008;74(4):123–35.
Kent A, et al. Sonographic evaluation of intravascular volume status in the surgical intensive care unit: a prospective comparison of subclavian vein and inferior vena cava collapsibility index. J Surg Res. 2013;184(1):561–6.
Resnick J, et al. Ultrasound does not detect early blood loss in healthy volunteers donating blood. J Emerg Med. 2011;41(3):270–5.
Keller AS, et al. Diagnostic accuracy of a simple ultrasound measurement to estimate central venous pressure in spontaneously breathing, critically ill patients. J Hosp Med. 2009;4(6):350–5.
Bailey JK, et al. Correlation of internal jugular vein/common carotid artery ratio to central venous pressure: a pilot study in pediatric burn patients. J Burn Care Res. 2012;33(1):89–92.
Deol GR, et al. Ultrasound accurately reflects the jugular venous examination but underestimates central venous pressure. Chest. 2011;139(1):95–100.
Schefold JC, et al. Inferior vena cava diameter correlates with invasive hemodynamic measures in mechanically ventilated intensive care unit patients with sepsis. J Emerg Med. 2010;38(5):632–7.
Manasia AR, et al. Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothorac Vasc Anesth. 2005;19(2):155–9.
Gunst M, et al. Accuracy of cardiac function and volume status estimates using the bedside echocardiographic assessment in trauma/critical care. J Trauma. 2008;65(3):509–16.
Gunst M, et al. Bedside echocardiographic assessment for trauma/critical care: the BEAT exam. J Am Coll Surg. 2008;207(3):e1–3.
Stawicki SP, et al. Intensivist use of hand-carried ultrasound to measure E/E’ and IVC collapsibility in estimating volume status: correlations with pulmonary artery and central venous pressures. South Med J. 2008;101:861.
Melamed R, et al. Assessment of left ventricular function by intensivists using hand-held echocardiography. Chest. 2009;135(6):1416–20.
Laupland KB, Bands CJ. Utility of esophageal Doppler as a minimally invasive hemodynamic monitor: a review. Can J Anaesth. 2002;49(4):393–401.
Eachempati SR, et al. The clinical use of an esophageal Doppler monitor for hemodynamic monitoring in sepsis. J Clin Monit Comput. 1999;15(3–4):223–5.
Kauffman KE. Newer trends in monitoring: the esophageal Doppler monitor. AANA J. 2000;68(5):421–8.
Atlas G, Mort T. Placement of the esophageal Doppler ultrasound monitor probe in awake patients. Chest. 2001;119(1):319.
Lichtenberger M, et al. Comparison of esophageal Doppler monitor generated minute distance and cardiac output in a porcine model of ventricular fibrillation. Resuscitation. 1999;41(3):269–76.
DiCorte CJ, et al. Esophageal Doppler monitor determinations of cardiac output and preload during cardiac operations. Ann Thorac Surg. 2000;69(6):1782–6.
Roeck M, et al. Change in stroke volume in response to fluid challenge: assessment using esophageal Doppler. Intensive Care Med. 2003;29(10):1729–35.
Hussien M, et al. Use of transesophageal Doppler as a sole cardiac output monitor for reperfusion hemodynamic changes during living donor liver transplantation: an observational study. Saudi J Anaesth. 2011;5(3):264–9.
Stawicki SP, et al. Esophageal Doppler monitoring during organ donor resuscitation: new benefits of existing technology. Prog Transplant. 2005;15(4):320.
Schober P, Loer SA, Schwarte LA. Perioperative hemodynamic monitoring with transesophageal Doppler technology. Anesth Analg. 2009;109(2):340–53.
Mondillo S, et al. Hand-held echocardiography: its use and usefulness. Int J Cardiol. 2006;111(1):1–5.
ImaCor, Inc. The hTEE approach. 2014 (cited 2014 August 15, 2014). Available from: http://imacorinc.com/htee/the-htee-approach.html.
Shillcutt SK, Bick JS. Echo didactics: a comparison of basic transthoracic and transesophageal echocardiography views in the perioperative setting. Anesth Analg. 2013;116(6):1231–6.
Mintz GS, Kotler MN. Clinical value and limitations of echocardiography. Its use in the study of patients with infectious endocarditis. Arch Intern Med. 1980;140(8):1022–7.
DeMaria AN, et al. Value and limitations of two dimensional echocardiography in assessment of cardiomyopathy. Am J Cardiol. 1980;46(7):1224–31.
DeMaria AN, et al. Value and limitations of contrast echocardiography in cardiac diagnosis. Cardiovasc Clin. 1983;13(3):167–79.
Mathur SK, Singh P. Transoesophageal echocardiography related complications. Indian J Anaesth. 2009;53(5):567–74.
Kneeshaw JD. Transoesophageal echocardiography (TOE) in the operating room. Br J Anaesth. 2006;97(1):77–84.
Sarosiek K, et al. Perioperative use of the imacor hemodynamic transesophageal echocardiography probe in cardiac surgery patients—initial experience. ASAIO J. 2014;60:553–8.
Cheitlin MD, et al. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). Circulation. 2003;108(9):1146–62.
Kenaan M, Gajera M, Goonewardena SN. Hemodynamic assessment in the contemporary intensive care unit: a review of circulatory monitoring devices. Crit Care Clin. 2014;30(3):413–45.
Joseph MX, et al. Transthoracic echocardiography to identify or exclude cardiac cause of shock. Chest. 2004;126(5):1592–7.
Vieillard-Baron A, et al. Echo-Doppler demonstration of acute cor pulmonale at the bedside in the medical intensive care unit. Am J Respir Crit Care Med. 2002;166(10):1310–9.
Stawicki SP, et al. Incidental findings on intensivist bedside ultrasonographic (INBU) examinations: why should we care? OPUS 12. Scientist. 2008;2(3):11–4.
Colreavy FB, et al. Transesophageal echocardiography in critically ill patients. Crit Care Med. 2002;30(5):989–96.
Price S, et al. Echocardiography in the critically ill: current and potential roles. Intensive Care Med. 2006;32(1):48–59.
Erbel R, et al. Echocardiography in diagnosis of aortic dissection. Lancet. 1989;1(8636):457–61.
Nienaber CA, et al. The diagnosis of thoracic aortic dissection by noninvasive imaging procedures. N Engl J Med. 1993;328(1):1–9.
Hilberath JN, et al. Safety of transesophageal echocardiography. J Am Soc Echocardiogr. 2010;23(11):1115–27 (quiz 1220-1).
Wagner CE, et al. Use of a miniaturized transesophageal echocardiographic probe in the intensive care unit for diagnosis and treatment of a hemodynamically unstable patient after aortic valve replacement. J Cardiothorac Vasc Anesth. 2012;26(1):95–7.
Stec S, et al. First experience with microprobe transoesophageal echocardiography in non-sedated adults undergoing atrial fibrillation ablation: feasibility study and comparison with intracardiac echocardiography. Europace. 2011;13(1):51–6.
Vieillard-Baron A, et al. A pilot study on safety and clinical utility of a single-use 72-h indwelling transesophageal echocardiography probe. Intensive Care Med. 2013;39(4):629–35.
Matulevicius SA, et al. Appropriate use and clinical impact of transthoracic echocardiography. JAMA Intern Med. 2013;173(17):1600–7.
Alqarqaz M, et al. Applicability, limitations and downstream impact of echocardiography utilization based on the appropriateness use criteria for transthoracic and transesophageal echocardiography. Int J Cardiovasc Imaging. 2012;28(8):1951–8.
Douglas PS, et al. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 appropriateness criteria for transthoracic and transesophageal echocardiography: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American Society of Echocardiography, American College of Emergency Physicians, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society for Cardiovascular Magnetic Resonance. Endorsed by the American College of Chest Physicians and the Society of Critical Care Medicine. J Am Soc Echocardiogr. 2007;20(7):787–805.
American College of Cardiology Foundation Appropriate Use Criteria Task Force et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance American College of Chest Physicians. J Am Soc Echocardiogr. 2011;24(3):229–67.
Mertz L. Ultrasound? Fetal monitoring? Spectrometer? There’s an app for that!: biomedical smart phone apps are taking healthcare by storm. IEEE Pulse. 2012;3(2):16–21.
Crofts G, Padman R, Maharaja N. Toward image analysis and decision support for ultrasound technology. Stud Health Technol Inform. 2013;192:1088.
Torbicki A, Tramarin R, Morpurgo M. Role of echo/Doppler in the diagnosis of pulmonary embolism. Clin Cardiol. 1992;15(11):805–10.
Lau G, Ther G, Swanevelder J. Echo rounds: McConnell’s sign in acute pulmonary embolism. Anesth Analg. 2013;116(5):982–5.
McConnell MV, et al. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996;78(4):469–73.
Casazza F, et al. Regional right ventricular dysfunction in acute pulmonary embolism and right ventricular infarction. Eur J Echocardiogr. 2005;6(1):11–4.
Cohen R, et al. Echocardiographic findings in pulmonary embolism: an important guide for the management of the patient. World J Cardiovasc Dis. 2012;2:161–4.
Pruszczyk P, et al. Noninvasive diagnosis of suspected severe pulmonary embolism: transesophageal echocardiography vs spiral CT. Chest. 1997;112(3):722–8.
Nazeyrollas P, et al. Use of transthoracic Doppler echocardiography combined with clinical and electrocardiographic data to predict acute pulmonary embolism. Eur Heart J. 1996;17(5):779–86.
Vaid U, et al. Poor positive predictive value of McConnell’s sign on transthoracic echocardiography for the diagnosis of acute pulmonary embolism. Hosp Pract (1995). 2013;41(3):23–7.
Joy J, Cooke I, Love M. Is ultrasound safe? Obstet Gynaecol. 2006;8(4):222–7.
Eeg KR, et al. Single center experience with application of the ALARA concept to serial imaging studies after blunt renal trauma in children—is ultrasound enough? J Urol. 2009;181(4):1834–40 (discussion 1840).
Toms DA. The mechanical index, ultrasound practices, and the ALARA principle. J Ultrasound Med. 2006;25(4):560–1 (author reply 561–2).
Canty DJ, et al. The impact of pre-operative focused transthoracic echocardiography in emergency non-cardiac surgery patients with known or risk of cardiac disease. Anaesthesia. 2012;67(7):714–20.
Lockhart ME, et al. The sonographer practitioner: one piece to the radiologist shortage puzzle. J Ultrasound Med. 2003;22(9):861–4.
Walvoord KH. Understanding sonographer burnout. J Diagn Med Sonogr. 2006;22:200–5.
Ferraioli G, Meloni MF. Sonographic training program at a district hospital in a developing country: work in progress. AJR Am J Roentgenol. 2007;189(3):W119–22.
Witt S. the sonographer shortage: a misguided debate or the real deal? J Am Soc Echocardiogr. 2005;18:A25–6.
Scholten C, et al. Hand-held miniaturized cardiac ultrasound instruments for rapid and effective bedside diagnosis and patient screening. J Eval Clin Pract. 2005;11(1):67–72.
Adams MS. Teaching TEE for use in the operating room: where are things now…and where are we going? J Am Soc Echocardiogr. 2012;25(6):17A–8A.
Nazerian P, et al. Diagnostic performance of emergency transthoracic focus cardiac ultrasound in suspected acute type A aortic dissection. Intern Emerg Med. 2014;9:665–70.
Hoffmann B, Gullett JP. Bedside transthoracic sonography in suspected pulmonary embolism: a new tool for emergency physicians. Acad Emerg Med. 2010;17(9):e88–93.
American Institute of Ultrasound in. M., R. American College of, and U. Society of Radiologists in, AIUM practice guideline for the performance of peripheral arterial ultrasound examinations using color and spectral doppler imaging. J Ultrasound Med. 2014;33(6):1111–21.
Mustapha JA, et al. Comparison between angiographic and arterial duplex ultrasound assessment of tibial arteries in patients with peripheral arterial disease: on behalf of the Joint Endovascular and Non-Invasive Assessment of LImb Perfusion (JENALI) Group. J Invasive Cardiol. 2013;25(11):606–11.
Liu YT, Alsaawi A, Bjornsson HM. Ultrasound-guided peripheral venous access: a systematic review of randomized-controlled trials. Eur J Emerg Med. 2014;21(1):18–23.
Stawicki SP, Hoey BA. Lower extremity arterial thrombosis following sonographically guided thrombin injection of a femoral pseudoaneurysm. J Clin Ultrasound. 2007;35(2):88–93.
Stawicki SP, et al. Vena cava filters: a synopsis of complications and related topics. J Vasc Access. 2008;9(2):102–10.
Chiles K, Nagdev A. Accidental carotid artery cannulation detected by bedside ultrasound. West J Emerg Med. 2011;12(1):100–1.
Hyman BN. Doppler sonography: a bedside noninvasive method for assessment of carotid artery disease. Am J Ophthalmol. 1974;77(2):227–31.
Zierler BK. Screening for acute DVT: optimal utilization of the vascular diagnostic laboratory. Semin Vasc Surg. 2001;14(3):206–14.
Magazzini S, et al. Duplex ultrasound in the emergency department for the diagnostic management of clinically suspected deep vein thrombosis. Acad Emerg Med. 2007;14(3):216–20.
Kircher BJ, Himelman RB, Schiller NB. Noninvasive estimation of right atrial pressures from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990;66:493–6.
Otto CM. Textbook of clinical echocardiography. 3rd ed. Philadelphia: W. B. Saunders; 2004.
Conflict of interest
The following authors of this manuscript: Nicholas Kelly, Rogette Esteve, Thomas J. Papadimos, Richard P. Sharpe, Scott A. Keeney, Robert DeQuevedo, Marc Portner, David P. Bahner, and Stanislaw P. Stawicki declare that they have no conflict of interest related to this work.
Compliance with ethical requirements
This work is in compliance with ethical requirements.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kelly, N., Esteve, R., Papadimos, T.J. et al. Clinician-performed ultrasound in hemodynamic and cardiac assessment: a synopsis of current indications and limitations. Eur J Trauma Emerg Surg 41, 469–480 (2015). https://doi.org/10.1007/s00068-014-0492-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-014-0492-6