Abstract
Type A aortic dissection (AD) is a deadly disease. Rapid identification of patients requiring immediate advanced aortic imaging or transfer to specialized centers is needed to improve outcomes. We evaluated the diagnostic performance of transthoracic focus cardiac ultrasound (FOCUS) performed by emergency physicians, alone and in combination with the aortic dissection detection (ADD) risk score in suspected type A AD. This was a prospective study performed on patients with suspected type A AD. FOCUS evaluated the presence of intimal flap/intramural hematoma (direct signs of AD), ascending aorta dilatation, aortic valve insufficiency or pericardial effusion/tamponade (indirect signs of AD). The ADD risk score of each patient was calculated according to guidelines. The final diagnosis was established after review of complete clinical data. 50 (18 %) patients of 281 had a final diagnosis of type A AD. Detection of any FOCUS sign (direct or indirect) of AD had a sensitivity of 88 % (95 % CI 76–95 %) for the diagnosis of type A AD. Presence of ADD risk score > 0 or detection of any FOCUS sign increased diagnostic sensitivity to 96 % (95 % CI 86–99 %). Detection of direct FOCUS signs had a specificity of 94 % (95 % CI 90–97 %), while combination of ADD risk score > 1 with detection of direct FOCUS signs had a specificity of 98 % (95 % CI 96–99 %). FOCUS demonstrated acceptable accuracy as a triage tool to rapidly identify patients with suspected type A AD needing advanced aortic imaging or transfer, but it cannot be used as a stand-alone test even if combined with ADD risk score classification.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute aortic dissection (AD) involving the ascending aorta (type A AD) is a deadly disease affecting 3–5 cases/100,000 individuals/year. Rapid identification of type A AD in the emergency department (ED) is paramount, as mortality rate is as high as 1 % per h without surgical treatment [1]. However, the diagnosis of type A AD is highly challenging, because clinical signs and symptoms are unspecific and most conditions in differential diagnosis are substantially more frequent than AD [1–4]. The aortic dissection detection (ADD) risk score, proposed by the clinical guidelines of the American Heart Association and the American College of Cardiology [5], is a bedside clinical triage tool that can help physicians to stratify patients in low, intermediate and high probability of AD. However, ADD risk score classification cannot be used per se to decide which patients need advanced aortic imaging diagnostic tests [6].
The utility of point-of-care ultrasound in acute cardiovascular diseases, including the use of transthoracic focus cardiac ultrasound (FOCUS) by emergency physicians (EP) to diagnose pericardial effusion, right ventricular strain, cardiac function and volume status, is well established [7]. Indeed, FOCUS is a rapid, safe and easily available imaging modality complementary to physical examination, that can potentially detect both direct sonographic signs (intimal flap and intramural hematoma) and indirect sonographic signs of type A AD (ascending aorta dilatation, pericardial effusion/tamponade and aortic valve insufficiency). The European Association of Echocardiography indicates transthoracic echocardiography as an appropriate triage/first-line imaging technique in the emergency management of patients with suspected AD [8]. Nonetheless, to our knowledge, no previous studies have evaluated so far the diagnostic performance of EP-performed FOCUS in patients suspected of AD. Moreover, although transthoracic echocardiography is not sufficiently accurate to be used as a stand-alone test to diagnose type A AD in all suspected patients [9–14], its diagnostic performance in association with the ADD risk score classification is unknown.
The aims of this study were the following: (1) to investigate the accuracy of EP-performed FOCUS for type A AD in patients presenting to the ED; (2) to evaluate if FOCUS can rule out type A AD in patients at low risk by ADD risk score classification and if FOCUS can rule in type A AD in patients at high risk by ADD risk score classification; (3) to investigate the accuracy of FOCUS in the subgroup of patients with shock/hypotension who are at immediate risk of death.
Methods
Study design
This was a prospective single-center cohort study of a convenience sample of patients presenting to the ED with suspected AD. The institutional review board approved the study and informed consent was obtained from patients (or next of kin, if needed).
Study setting and enrollment
The study was performed in the ED of an adult tertiary university hospital with an annual census of 120,000 visits. The hospital is a regional cardiothoracic surgery hub center providing computed tomography angiography (CTA), transesophageal echocardiography (TEE) and cardio-surgical consultation 24 h/7 days.
Consecutive patients aged >18 years, presenting to ED from January 1 2009 to December 31 2012 were prospectively included in the study, if all the following criteria were satisfied: (1) presentation to the ED with any of the following symptoms: chest, pain, abdominal pain, syncope or symptoms of perfusion deficit (central nervous system, mesenteric, myocardial, or limb ischemia), as suggested by clinical guidelines [5]; (2) the clinical suspicion of AD by the attending physician was high enough to request an urgent aortic imaging exam such as CTA or TEE to explicitly identify or rule out AD and (3) FOCUS was performed at patient presentation in the ED before conclusive diagnosis with CTA or TEE.
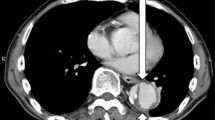
Transthoracic focus heart ultrasound
FOCUS was performed by one of the seven EP-sonographers with at least 2 years of experience in FOCUS. An EP-sonographer was present to enroll patients for an average of 14 h per day (including nights, weekends and festivities). Attending EPs were not blinded to FOCUS results. The following machines equipped with a 2–5 MHz phased array probe were used: MyLab30 Gold (Esaote, Genova, Italy) and HD7 (Philips, Amsterdam, Holland). Evaluation of the aorta was performed with the patient in the supine and left lateral decubitus positions using multiple views: left parasternal, left high parasternal, apical or subcostal. The following were considered direct sonographic signs of type A AD: presence of an intimal flap (flap separating two aortic lumens) or intramural hematoma (circular or crescentic thickening of the aortic wall >5 mm) in the ascending aorta. The following echocardiographic findings indicative of high-risk features or complications were also researched and considered as indirect sonographic signs of type A AD: ascending aorta enlargement (diameter ≥4 cm), pericardial effusion or tamponade and aortic valve regurgitation at color doppler.
Aortic dissection detection risk score classification
For each patient, the ADD risk score was calculated by independent physician review of medical charts, as previously described [6]. The ADD risk score is calculated on the presence of 12 high-risk markers in the clinical categories of predisposing conditions, pain features and physical findings (Table 1). Patients lacking all risk markers (ADD risk score = 0) are classified at low risk for aortic dissection, patients with one or more risk markers in any single category (ADD risk score = 1) are classified at intermediate risk of aortic dissection, while patients with one or more risk markers in two or three categories (ADD risk score > 1) are classified at high risk of aortic dissection.
Aortic imaging and final diagnosis
The aortic imaging tests used to confirm or refuse type A AD in the ED were CTA or TEE. CTA was performed with Somatom definition As4 and AS128 (Siemens, Erlangen, Germany) and TEE with MyLab30 (Esaote, Genova, Italy). CTA and TEE were interpreted by specialized radiologists and cardiologists not involved in the present study.
The final diagnosis was established by two independent senior physicians who reviewed all available clinical data, aortic imaging studies, medical, surgical and autopsy records. In case of discordant diagnosis, SG adjudicated the final diagnosis. Any of the following diagnoses were considered as type A AD: classical Stanford type A aortic dissection, intramural hematoma of the ascending aorta and penetrating aortic ulcer of the ascending aorta.
Statistical analysis
Dichotomous data are expressed as proportions and continuous data are expressed as mean ± standard deviation (SD). Fisher’s exact test was used for the comparison of dichotomous data, and the unpaired Student’s t test was used to compare normally distributed data. The diagnostic performance of direct and indirect sonographic signs of type A AD and of low and high ADD risk categories were assessed by computing sensitivity, specificity, negative and positive predictive values and negative and positive likelihood ratios with their 95 % confident interval (CI). The diagnostic performance of FOCUS was calculated also in combination with ADD risk score classification and in the subgroup of patients with shock/hypotension. P values were two-sided, and a P value lower than 0.05 was considered as statistically significant. Analysis was performed with the SPSS statistical package (version 17.0, SPSS Inc., Chicago, IL).
Results
During the study period, a total of 281 patients were enrolled. Presenting symptoms were the following: anterior chest pain (198, 70.5 %), back pain (72, 25.6 %), abdominal pain (40, 14.2 %), syncope (59, 21 %), symptoms of perfusion deficit (21, 7.5 %). Type A AD was finally diagnosed in 50 (17.8 %) patients: 45 (16 %) patients had classical Stanford type A aortic dissection and 5 (1.8 %) had an intramural hematoma of the ascending aorta. Type A AD was ruled out in 231 (82.2 %) patients, with 13 (4.6 %) patients presenting acute AD not involving the ascending aorta (7 classical Stanford type B AD, 5 intramural hematomas and 1 penetrating aortic ulcer not involving the ascending aorta). Other diagnoses were: acute coronary syndrome (43 patients, 15.3 %), gastrointestinal disease (23, 8.2 %), non-AD-related syncope (20, 7.1 %), pericarditis (20, 7.1 %), non-AD-related stroke (7, 2.5 %), non-AD-related limb or organ acute ischemia (7, 2.5 %), pulmonary embolism (2, 0.7 %), musculoskeletal chest pain (87, 31 %) and other diagnoses (9, 3.2 %). 12 patients (24 % of 50) with type A AD and three patients without type A AD (1.3 % of 231) died during hospital stay.
FOCUS detected direct sonographic signs of type A AD (intimal flap/intramural hematoma) in 27 patients (54 % of 50) with type A AD, including 26 patients (57, 8 % of 45) with classical Stanford type A AD and one patient (20 % of 5) with intramural hematoma of the ascending aorta (Table 2). Direct signs of type A AD at FOCUS were falsely present in 14 patients (6.1 % of 231). The derived sensitivity and specificity were 54 % (95 % CI 39–68 %) and 94 % (95 % CI 90–97 %), respectively. Presence of at least one sonographic sign (either direct or indirect) had a sensitivity of 88 % (95 % CI 76–95 %) and a specificity of 56 % (95 % CI 49–62 %) for the diagnosis of type A AD (Table 3).
The diagnostic accuracy of FOCUS was next assessed when used in combination with ADD risk score classification of study patients. The prevalence of type A AD was, respectively, 7.1 % (5 of 70), 17 % (25 of 147) and 31.2 % (20 of 64) in low-risk (ADD risk score = 0), intermediate-risk (ADD risk score = 1) and high-risk patients (ADD risk score > 1). A “normal” FOCUS (no sonographic signs of type A AD) was present in 36 patients at low risk based on ADD risk score classification, with 2 patients (5.6 %) finally diagnosed with type A AD. Presence of ADD risk score > 0 or detection of any sonographic sign of AD lead to a derived sensitivity and negative predictive value to rule out type A AD of 96 % (95 % CI 86–99 %) and 94 % (95 % CI 81–99 %), respectively (Table 3). Direct sonographic signs of type A AD (intimal flap/intramural hematoma) were present in 16 patients at high risk based on ADD risk score classification, with four patients (25 %) receiving a final alternative diagnosis. Combination of high risk (ADD risk score > 1) with detection of direct sonographic signs of type A AD lead to a derived specificity and positive predictive value to rule in type A AD of 98 % (95 % CI 96–99 %) and 86 % (95 % CI 81–90 %), respectively (Table 3).
The diagnostic accuracy of FOCUS was finally analyzed in patients presenting with shock or hypotension, where a prompt diagnosis of type A AD is essential to allow immediate life-saving surgical intervention. In 33 (11.7 %) patients with suspected type A AD presenting with shock/hypotension, presence of intimal flap/intramural hematoma at FOCUS showed a sensitivity, specificity, positive and negative predictive value of 60 % (95 % CI 36–81 %), 100 %, 100 % and 62 % (95 % CI 38–82 %), respectively. In this patient subgroup, presence of any sonographic sign (either direct or indirect) of type A AD showed a sensitivity, specificity, positive and negative predictive value of 100 %, 54 % (95 % CI 25–81 %), 77 % (95 % CI 56–91 %) and 100 %, respectively.
Discussion
FOCUS is widely available in almost all EDs, and may be used also out of hospital. It can be performed in few minutes and while other diagnostic or therapeutic procedures are in place. At the same time, FOCUS can provide pivotal information immediately at patient’s presentation. Type A AD is a cardiovascular emergency characterized by a high mortality rate concentrated within few hours from presentation without specialized surgical treatment [1, 2]. Hence, EP-performed FOCUS appears as a potentially ideal triage tool for patients with suspected AD. The present study is, to our knowledge, the first assessing the diagnostic accuracy of EP-performed FOCUS in suspected type A AD.
So far, transthoracic echocardiography performed by specialized cardiologists in different clinical settings has shown variable levels of sensitivity (from 57 to 88 %) and specificity (from 65 to 96 %) for the detection of classic type A AD [9–14]. In a recent study by Cecconi and co-workers [14] evaluating the diagnostic performance of transthoracic echocardiography performed by well-trained cardiologists with a long-standing experience, in 270 patients with suspected type A AD in intensive care unit or ED, the sensitivity of direct sonographic signs of AD was substantially higher (87%, 95 % CI 75–93 %) than in our study (54 %, 95 % CI 39–68 %), indicating that specialized training and experience in echocardiography largely affect the sensitivity of this technique [14]. Nonetheless, in our study, presence of at least one sonographic sign (either direct or indirect) of type A AD leads to a similar diagnostic sensitivity (88 %, 95 % CI 76–95 %). The specificity of direct sonographic sign was similar in the study by Cecconi (91 %, 95 % CI 85–94 %) and in the present study (96 %, 95 % CI 90–97 %).
The results of our study indicate that FOCUS performed by EPs can be used as a triage tool in patients with suspected type A AD to rapidly identify patients requiring immediate execution of advanced aortic imaging exams or rapid patient transport to specialized centers for further life-saving evaluation or surgical treatment. However, as shown in previous studies, FOCUS cannot be used as a stand-alone test to rule in or to rule out type A AD in all patients. In our cohort, for instance, six potentially life-saving operations would have been missed if the decision had been based only on the detection of a “normal” FOCUS; and if one had based the decision to send patients to immediate surgery on the diagnosis of intimal flap/intramural hematoma at FOCUS examination, 14 inappropriate interventions would have been generated. The inadequate accuracy of FOCUS has to be compared with 95–100 % sensitivity and 94–100 % specificity when using advanced aortic imaging studies such as CTA, TEE or magnetic resonance imaging [2, 15–17].
A key finding of our study is that type A AD cannot be safely ruled out or ruled in by FOCUS at bedside even if combined with ADD risk score classification. In fact, a “normal” FOCUS was present in two patients at low ADD risk score finally diagnosed with type A AD. The false negative proportion (5.6 %) was higher than the estimated threshold clinical probability of AD above which the benefits of testing with magnetic resonance (2 %) or CTA (3 %) outweigh its risks [18]. On the other hand, combination of high risk based on ADD risk score classification with the detection of an intimal flap/intramural hematoma at FOCUS showed a high specificity (98 %, 95 % CI 96–99 %). However, FOCUS was falsely positive in four patients at high risk, thus raising doubts about the opportunity of operating on these patients without further advance aortic imaging. As proposed by the European Association of Echocardiography [8], to save time, patients at high risk of AD with a direct sign of type A AD detected at FOCUS could be sent directly to surgery only provided that intraoperative TEE is performed before surgery.
A special consideration has to be done for severe patients with shock/hypotension, where FOCUS detection of direct signs of type AD showed 100 % specificity. In these patients, FOCUS could substantially impact on clinical decisions, as patient transport to CTA may not be safe or feasible and patients might proceed directly to the operative room and diagnostic evaluation completed by intraoperative TEE. Furthermore, in patients with shock/hypotension without direct or indirect sonographic signs of type A AD (“normal” FOCUS), type A AD could be ruled out with 100 % sensitivity.
Limitations
This study was performed at a single tertiary care center, which may limit its generalizability. Seven EPs performed FOCUS and were available to enroll study subjects for approximately 100 h per week. Consequently, the study used a convenience sample based on sonographer availability. Attending physicians were not blinded to FOCUS results, which could have influenced in some cases their decision to perform further testing. Finally, the study was not specifically powered to evaluate the diagnostic performance of FOCUS in the subgroup of patients with shock and hypotension.
Conclusions
FOCUS can be used as a rapid first-line tool to triage patients with suspected type A AD, providing the EP with important elements in his/her decision to proceed rapidly with advanced aortic imaging tests or with patient transfer to specialized facilities in a hub-and-spoke healthcare system. However, FOCUS cannot be used as a stand-alone test to rule in and rule out type A AD even if combined with ADD risk score classification. Preliminary findings indicate that FOCUS can rapidly provide crucial diagnostic information in patients presenting with shock or hypotension, but further larger studies are warranted.
References
Coady MA, Rizzo JA, Goldstein LJ, Elefteriades JA (1999) Natural history, pathogenesis, and etiology of thoracic aortic aneurysms and dissections. Cardiol Clin 17(4):615–635
Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, Evangelista A, Fattori R, Suzuki T, Oh JK, Moore AG, Malouf JF, Pape LA, Gaca C, Sechtem U, Lenferink S, Deutsch HJ, Diedrichs H, Marcos y Robles J, Llovet A, Gilon D, Das SK, Armstrong WF, Deeb GM, Eagle KA (2000) The international registry of acute aortic dissection (IRAD) new insights into an old disease. JAMA 283:897–903
Sullivan PR, Wolfson AB, Leckey RD, Burke JL (2000) Diagnosis of acute thoracic aortic dissection in the emergency department. Am J Emerg Med 18:46–50
Hansen MS, Nogareda GJ, Hutchison SJ (2007) Frequency of and inappropriate treatment of misdiagnosis of acute aortic dissection. Am J Cardiol 99:852–856
Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, Eagle KA, Hermann LK, Isselbacher EM, Kazerooni EA, Kouchoukos NT, Lytle BW, Milewicz DM, Reich DL, Sen S, Shinn JA, Svensson LG, Williams DM (2010) 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines, American Association for thoracic surgery, American College of radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation 121:e266–e369
Nazerian P, Giachino F, Vanni S, Veglio MG, Castelli M, Lison D, Bitossi L, Moiraghi C, Grifoni S, Morello F (2014) Diagnostic performance of the aortic dissection detection risk score in patients with suspected acute aortic dissection. Eur Heart J Acute Cardiovasc Care (Epub ahead of print)
Labovitz AJ, Noble VE, Bierig M, Goldstein SA, Jones R, Kort S, Porter TR, Spencer KT, Tayal VS, Wei K (2010) Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr 23(12):1225–1230
Evangelista A, Flachskampf FA, Erbel R, Antonini-Canterin F, Vlachopoulos C, Rocchi G, Sicari R, Nihoyannopoulos P, Zamorano J (2010) Echocardiography in aortic diseases: EAE recommendations for clinical practice. Eur J Echocardiogr 11:645–658
McLeod AA, Monaghan MJ, Richardson PJ, Jackson G, Jewitt DE (1983) Diagnosis of acute aortic dissection by M-mode and cross-sectional echocardiography: a five-year experience. Eur Heart J 4:196–202
Roudaut RP, Billes MA, Gosse P, Deville C, Baudet E, Fontan F, Besse P, Bricaud H, Dallocchio M (1988) Accuracy of M-mode and two dimensional echocardiography in the diagnosis of aortic dissection: an experience with 128 cases. Clin Cardiol 11:553–562
Khandheria BK, Tajik AJ, Taylor CL, Safford RE, Miller FA Jr, Stanson AW, Sinak LJ, Oh JK, Seward JB (1989) Aortic dissection: review of value and limitations of two-dimensional echocardiography in a six-year experience. J Am Soc Echocardiogr 2:17–24
Enia F, Ledda G, Lo Mauro R, Matassa C, Raspanti G, Stabile A (1989) Utility of echocardiography in the diagnosis of aortic dissection involving the ascending aorta. Chest 95:124–129
Evangelista A, Avegliano G, Aguilar R, Cuellar H, Igual A, González-Alujas T, Rodríguez-Palomares J, Mahia P, García-Dorado D (2010) Impact of contrast-enhanced echocardiography on the diagnostic algorithm of acute aortic dissection. Eur Heart J 31:472–479
Cecconi M, Chirillo F, Costantini C, Iacobone G, Lopez E, Zanoli R, Gili A, Moretti S, Manfrin M, Münch C, Torracca L, Perna GP (2012) The role of transthoracic echocardiography in the diagnosis and management of acute type A aortic syndrome. Am Heart J 163(1):112–118
Cigarroa JE, Isselbacher EM, DeSanctis RW, Eagle KA (1993) Diagnostic imaging in the evaluation of suspected aortic dissection. N Engl J Med 328:35–43
Ballal RS, Nanda NC, Gatewood R, D’Arcy B, Samdarshi TE, Holman WL, Kirklin JK, Pacifico AD (1991) Usefulness of transesophageal echocardiography in assessment of aortic dissection. Circulation 84:1903–1914
Shiga T, Wajima Z, Apfel CC, Inoue T, Ohe Y (2006) Diagnostic accuracy of transesophageal echocardiography, helical computed tomography, and magnetic resonance imaging for suspected thoracic aortic dissection. Arch Intern Med 166:1350–1356
Sarasin FP, Louis-Simonet M, Gaspoz JM, Junod AF (1996) Detecting acute thoracic aortic dissection in the emergency department: time constraints and choice of the optimal diagnostic test. Ann Emerg Med 28:278–288
Acknowledgments
The authors thank all patients and personnel involved.
Conflict of interest
The authors have no potential conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nazerian, P., Vanni, S., Castelli, M. et al. Diagnostic performance of emergency transthoracic focus cardiac ultrasound in suspected acute type A aortic dissection. Intern Emerg Med 9, 665–670 (2014). https://doi.org/10.1007/s11739-014-1080-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-014-1080-9