Abstract
Purpose
Transcatheter angiographic embolization (TAE) has been widely accepted as a treatment for hemorrhagic shock associated with pelvic fracture. Gluteal muscle necrosis is a rare but potentially fatal complication of TAE. This study aimed to clarify factors associated with safer embolization procedures by evaluating relationships between embolic site and risk of gluteal skin injury.
Methods
We classified embolized arteries into six groups: group A, nonselective embolization from the main internal iliac artery; group B, selective embolization including the superior gluteal artery but excluding the inferior gluteal artery; group C, selective embolization including the inferior gluteal artery but excluding the superior gluteal artery; group D, selective embolization including both the superior and inferior gluteal arteries; group E, selective embolization excluding both the superior and inferior gluteal arteries; and group F, no embolization. We assessed the frequency of gluteal injuries, relationships between gluteal injuries and embolized arteries, and the contributions of selective embolization, conservation of the superior or inferior gluteal artery, and conservation of both the superior and inferior gluteal arteries to reducing the risk of gluteal injury.
Results
Gluteal skin injuries were seen at 15 of 160 sites (9.4%). A significant difference was noted between the nonselective embolization group (group A: 10/82, 12.2%) and selective embolization excluding both the superior and inferior gluteal arteries (group E: 1/39, 2.6%) (p = 0.042).
Conclusions
If possible, we recommend selective embolization avoiding the superior and inferior gluteal arteries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Serious hemorrhage is a well-recognized complication of unstable pelvic fractures [1–4] and represents a principal cause of early mortality [4]. Transcatheter angiographic embolization (TAE) has been widely accepted as a treatment for hemorrhagic shock associated with pelvic fracture [5–7]. However, complications from embolization of the internal iliac artery have been described, including skin necrosis [8], bladder wall necrosis [9, 10], avascular necrosis of the femoral head [11], and neurological complications such as Brown–Sequard syndrome [12] and paresis [13, 14].
Gluteal muscle necrosis following TAE for pelvic fracture is a rare but potentially fatal complication of the procedure. Due to its rarity, the condition has not been examined in detail. Suzuki et al. [15] reported that all 12 patients with gluteal necrosis they had encountered had undergone TAE of bilateral internal iliac arteries with gelatin sponge slurries. However, the relationships between embolized arteries and gluteal injury are yet to be clarified.
The purpose of this study was therefore to evaluate correlations between embolized arteries and gluteal injury following TAE for hemorrhage associated with pelvic fracture.
Materials and methods
Institutional review board exemption was obtained for this retrospective study. Informed consent for arterial embolization was obtained for all patients in this study.
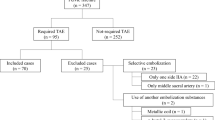
From January 2000 to December 2008, a total of 139 hemodynamically unstable pelvic fracture cases were managed using TAE of the internal iliac arteries to control retroperitoneal bleeding at our trauma center (fall from height, n = 60; traffic accident, n = 70; mechanical compression, n = 9). Among these, 41 patients died within the first 24 h. All 196 internal iliac arteries in the remaining 98 patients (56 men, 42 women) were analyzed for this study. Mean age was 37.4 years (range 16–78 years) and mean injury severity score (ISS) was 21.2 (range 4–50). Gluteal skin injuries that had not been observed on admission were diagnosed in 13 patients (13.3%). Skin injuries localized in the sacral region were excluded in this study, given the strong possibility of decubitus ulcer due to pressure from bony prominences.
Angiography and embolization methods
Intra-arterial digital-subtraction angiography (DSA) (Polystar; Siemens Medical System, Munich, Germany) was performed using a standard technique with a 6-F introducer sheath with a side connection for arterial pressure monitoring.
Femoral artery access was conducted through the side contralateral to the severely injured artery on radiological examinations [as determined from computed tomography (CT) and pelvic plain radiography].
A 5-F catheter (Formorcath; Cathex, Tokyo, Japan) was first inserted into the contralateral internal iliac artery. Arteriography of the main internal iliac was performed to detect hemorrhagic arterial branches. In severely hemodynamically unstable patients and in patients with multiple hemorrhagic arterial branches, immediate embolization of the main internal iliac artery (nonselective embolization) was performed using approximately 2 × 2 × 2 mm gelatin sponge particles (Gelform; Upjohn, Kalamazoo, MI, USA) made with a scissor-cutting technique until extravasation of the contrast material completely disappeared on arteriography. Additional embolization of the main internal iliac artery with 5–8 mm steel coils (Cook, Bloomington, IN, USA) was often performed as a supplementary procedure. In patients who were not severely hemodynamically unstable, selective catheterization and embolization of the injured arteries was performed through a coaxial catheter (selective embolization) with the gelatin sponge particles (and often steel coils) until extravasation of the contrast material completely disappeared. Ipsilateral internal iliac arteriography was then performed using a 5-F pre-shaped shepherd hook catheter. When embolization successfully stabilized the hemodynamics and the absence of extravasation was confirmed on angiography of the branches, no further embolization was performed in the ipsilateral internal iliac arteries. Hemodynamic condition stabilized immediately following successful embolization.
Assessment of embolic site and skin injury site
The gluteal skin and internal iliac arteries in the 98 patients were divided into 196 sites and arteries (right and left).
Embolized arteries were classified into the following six groups (Fig. 1): group A, nonselective embolization; group B, selective embolization including the superior gluteal artery but conserving the inferior gluteal artery; group C, selective embolization including the inferior gluteal artery but conserving the superior gluteal artery; group D, selective embolization including both the superior and inferior gluteal arteries; group E, selective embolization conserving both the superior and inferior gluteal arteries; and group F, no embolization (only from opposite internal iliac arteries).
Severity of skin injuries was classified into the following four grades: grade 0, no injury; grade I, skin reddish or swelling; grade II, skin ulcer (Fig. 2); and grade III, skin and muscle necrosis (Fig. 3).
Statistical analysis
First, the frequency of gluteal injuries was analyzed. Next, relationships between gluteal injuries and embolized arteries were analyzed. Finally, the contributions of selective embolization and conservation of the superior and/or inferior gluteal arteries to reducing the risk of gluteal injury were assessed.
Statistical analysis was performed using the JMS 5.0.1 J software package (SAS Institute, NC, USA). A value of p < 0.05 was considered significant.
Results
Embolization was performed for 160 of 196 internal iliac arteries (groups A + B + C + D + E). Gluteal skin injuries that had not been observed on admission were identified in 15 of 160 sites (9.4%). Skin injuries were seen in 10 of 82 sites (12.2%) in group A, 0 of 14 (0%) in group B, 3 of 20 (15.0%) in group C, 1 of 5 (20.0%) in group D, and 1 of 39 (2.6%) in group E (Tables 1, 2).
Our study revealed a higher frequency of gluteal skin injuries in the nonselective embolization group (group A: 10/82, 12.2%) (Fig. 4) than in groups with selective embolization of hemorrhagic branches (groups B + C + D + E: 5/78, 6.4%). The odds ratio for gluteal skin injuries in group A compared to groups B + C + D + E was 2.03 (95% confidence interval 0.68–6.78; p = 0.205).
A 40-year-old man injured in a fall from height. Severe gluteal injury including muscle (grade III) was noted on the right side after nonselective embolization (group A). a Right internal iliac arteriogram demonstrating multiple foci of extravasation of contrast medium (arrows). b Extravasation of contrast medium disappeared after embolization
No significant difference was seen between groups with embolization including (groups A + B + D: 11/101, 10.9%) and conserving (groups C + E: 4/59, 6.8%) the superior gluteal arteries (odds ratio 1.68; 95% confidence interval 0.54–6.30; p = 0.379).
Statistical analysis of each selective embolization group compared to the nonselective embolization group is described below. Odds ratios were 4.200 (95% confidence interval 0.23–75.77; p = 0.067) in group B, 0.79 (95% confidence interval 0.21–3.79; p = 0.740) in group C, 0.56 (95% confidence interval 0.07–11.44; p = 0.633) in group D, and 5.83 (95% confidence interval 1.06–108.92; p = 0.041) in group E.
On the other hand, gluteal skin injuries were also identified in sites with no embolization (group F: 2/31, 6.5%). Severe gluteal injuries including muscle (grade III) were noted at 6 sites from 5 cases.
We used gelatin sponge particles alone in 47 and additional steel coils in 113 internal iliac arteries. Six of 47 sites (12.8%) in which gelatin sponge particles were used alone and 11 of 113 sites (9.7%) in which additional steel coils were used showed gluteal skin injuries. The odds ratio for additional coils compared to gelatin sponge particles alone was 0.74 (95% confidence interval 0.26–2.26; p = 0.572) (Fig. 5).
Discussion
Ischemic necrosis of the buttock muscles following TAE is rare, because a potentially well-developed network of arterial collaterals in the hip region is available to maintain a sufficient blood supply. In our study, 9.4% of the embolized sites showed skin injuries. However, the rate of severe skin injury requiring clinical care (grade II or III, n = 11) was 6.9% among the embolic sites. Soft tissue injuries extending to deep spaces normally require the use of skin/muscle flaps for stable wound coverage. Skin grafts often show unsuccessful results in the presence of such ischemic injuries.
As serious hemorrhage in pelvic fracture is a life-threatening complication, nonselective embolization of bilateral internal iliac arteries with gelatin sponge particles will be necessary to control multiple bleeding sites and concealed arterial injuries caused by vasospasm, in order to preserve life in cases of major hemodynamic instability that persist despite failure to identify any arterial lesion [16, 17]. Velmahos et al. [16] noted no severe morbidity in relation to nonselective embolization of bilateral internal iliac arteries in the 30 patients in their study. Although nonselective occlusion of bilateral internal iliac arteries has not generally been thought to give rise to any complications [18–20], some disadvantages to TAE of the internal iliac artery have been reported [15, 21].
The present study revealed a higher frequency of gluteal skin injuries in cases with nonselective embolization of the main internal iliac artery compared to selective embolization. Nonselective embolized sites showed skin injuries in 12.2%.
Gluteal soft tissue is almost entirely supplied by the superior and inferior gluteal arteries, so we tried to evaluate the importance of selective embolization conserving those arteries. The superior gluteal artery is one of the main feeding arteries for the gluteal region, and embolization is easily avoided without wasting time in emergency situations because of the anatomical position. However, no significant difference was seen between groups with embolization including the superior gluteal arteries and those conserving the superior gluteal arteries. Statistical analysis of the groups with each selective embolization compared to groups with nonselective embolization found significant differences only in the group with selective embolization conserving both the superior and inferior gluteal arteries. As bleeding in muscles is easily stopped due to the tamponade effect, we suggest avoiding embolization of the superior and inferior gluteal arteries to reduce the risk of skin injury, if the hemodynamic condition of the patient is tolerable.
Gelatin sponge particles are appropriate emboli in cases involving single or multiple injuries of small arteries, and are also useful when more distal occlusion is needed or when multiple collateral channels are considered to be present. As gelatin sponge particles represent temporary occluding agents, the affected arteries often recanalize within a few days. However, embolization with small particles reaching to the capillary level is contraindicated because of the potential for elimination of collateral flow, resulting in massive tissue necrosis. Addition of steel coils to reduce blood flow toward the injured vessels is considered to have little influence on gluteal skin injuries, because steel coils only clamp the proximal portion of a vessel without impairing the development of distal collateral pathways.
Gluteal skin injuries were also shown at three sites in the nonembolization group. We cannot draw any conclusion from our study regarding why skin injuries were noted. Pelvic fracture sometimes accompanies gluteal soft tissue injuries, although the significance of injuries may not initially be apparent. Peripheral hypocirculation due to unstable blood pressure could also potentially interrupt the development of collateral arteries.
Conclusion
Based on the present findings, we recommend performing selective embolization while avoiding the superior and inferior gluteal arteries wherever possible in cases of hemorrhagic pelvic fracture. If only the superior gluteal artery is conserved, no decrease in skin injury risk can be obtained. The possibility of skin injuries in unembolized gluteal regions must also be recognized.
References
Evers BM, Cryer HM, Miller FB. Pelvic fracture hemorrhage. Priorities in management. Arch Surg. 1989;124(4):422–4.
Ghanayem AJ, Stover MD, Goldstein JA, Bellon E, Wilber JH. Emergent treatment of pelvic fractures. Comparison of methods for stabilization. Clin Orthop Relat Res. 1995;318:75–80.
Moreno C, Moore EE, Rosenberger A, Cleveland HC. Hemorrhage associated with major pelvic fracture: a multispecialty challenge. J Trauma. 1986;26(11):987–94.
Rothenberger DA, Fischer RP, Strate RG, Velasco R, Perry JF Jr. The mortality associated with pelvic fractures. Surgery. 1978;84(3):356–61.
Westhoff J, Laurer H, Wutzler S, Wyen H, Mack M, Maier B, Marzi I. Interventional emergency embolization for severe pelvic ring fractures with arterial bleeding. Integration into the early clinical treatment algorithm. Unfallchirurg. 2008;111(10):821–8.
Margolies MN, Ring EJ, Waltman AC, Kerr WS Jr. Baum S: arteriography in the management of hemorrhage from pelvic fractures. N Engl J Med. 1972;287(7):317–21.
Ben-Menachem Y, Coldwell DM, Young JW, Burgess AR. Hemorrhage associated with pelvic fractures: causes, diagnosis, and emergent management. Am J Roentgenol. 1991;157(5):1005–14.
Lang EK. Transcatheter embolization of pelvic vessels for control of intractable hemorrhage. Radiology. 1981;140(2):331–9.
Hietala SO. Urinary bladder necrosis following selective embolization of the internal iliac artery. Acta Radiol Diagn (Stockh). 1978;19(2):316–20.
Sieber PR. Bladder necrosis secondary to pelvic artery embolization: case report and literature review. J Urol. 1994;151(2):422.
Obaro RO, Sniderman KW. Case report: avascular necrosis of the femoral head as a complication of complex embolization for severe pelvic haemorrhage. Br J Radiol. 1995;68(812):920–2.
Giuliani L, Carmignani G, Belgrano E, Puppo P. Gelatin foam and isobutyl-2-cyanoacrylate in the treatment of life-threatening bladder haemorrhage by selective transcatheter embolisation of the internal iliac arteries. Br J Urol. 1979;51(2):125–8.
Diamond NG, Casarella WJ, Bachman DM, Wolff M. Microfibrillar collagen hemostat: a new transcatheter embolization agent. Radiology. 1979;133(3 Pt 1):775–9.
Hare WS, Holland CJ. Paresis following internal iliac artery embolization. Radiology. 1983;146(1):47–51.
Suzuki T, Shindo M, Kataoka Y, Kobayashi I, Nishimaki H, Yamamoto S, Uchino M, Takahira N, Yokoyama K, Soma K. Clinical characteristics of pelvic fracture patients with gluteal necrosis resulting from transcatheter arterial embolization. Arch Orthop Trauma Surg. 2005;125(7):448–52.
Velmahos GC, Chahwan S, Hanks SE, Murray JA, Berne TV, Asensio J, Demetriades D. Angiographic embolization of bilateral internal iliac arteries to control life-threatening hemorrhage after blunt trauma to the pelvis. Am Surg. 2000;66(9):858–62.
Velmahos GC, Toutouzas KG, Vassiliu P, Sarkisyan G, Chan LS, Hanks SH, Berne TV, Demetriades D. A prospective study on the safety and efficacy of angiographic embolization for pelvic and visceral injuries. J Trauma. 2002;53(2):303–8. Discussion 308.
Andriole GL, Sugarbaker PH. Perineal and bladder necrosis following bilateral internal iliac artery ligation. Report of a case. Dis Colon Rectum. 1985;28(3):183–4.
Connolly JE, Ingegno M, Wilson SE. Preservation of the pelvic circulation during infrarenal aortic surgery. Cardiovasc Surg. 1996;4(1):65–70.
Sadahiro S, Ishida H, Suzuki T, Ishikawa K, Tajima T, Makuuchi H. Vesicular blood flow after ligation of the internal iliac arteries in low anterior resection or abdominoperineal resection. Dis Colon Rectum. 1999;42(11):1475–9.
Takahira N, Shindo M, Tanaka K, Nishimaki H, Ohwada T, Itoman M. Gluteal muscle necrosis following transcatheter angiographic embolisation for retroperitoneal haemorrhage associated with pelvic fracture. Injury. 2001;32(1):27–32.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hamaguchi, S., Nakajima, Y. & Inoue, T. Clinical re-evaluation of the relationship between gluteal injuries and embolized arteries in patients with massive hemorrhage following pelvic fracture. Eur J Trauma Emerg Surg 38, 417–421 (2012). https://doi.org/10.1007/s00068-011-0174-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-011-0174-6