Abstract
Purpose
The aim of this study was to compare the diagnostic accuracy of 3D time-of-flight (TOF-MRA) and contrast-enhanced (CE-MRA) magnetic resonance angiography at 3 T for detection and quantification of proximal high-grade stenosis using multidetector computed tomography angiography (MDCTA) as reference standard.
Methods
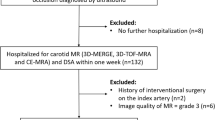
The institutional ethics committee approved this prospective study. A total of 41 patients suspected of having internal carotid artery (ICA) stenosis underwent both MDCTA and MRA. CE-MRA and TOF-MRA were performed using a 3.0-T imager with a dedicated eight-element cervical coil. ICA stenoses were measured according to the North American Symptomatic Carotid Endarterectomy Trial criteria and categorized as 0–25 % (minimal), 25–50 % (mild), 50–69 % (moderate), 70–99 % (high grade), and 100 % (occlusion). Sensitivity and specificity for the detection of high-grade ICA stenoses (70–99 %) and ICA occlusions were determined. In addition, intermodality agreement was assessed with κ-statistics for detection of high-grade ICA stenoses (70–99 %) and ICA occlusions.
Results
A total of 80 carotid arteries of 41 patients were reviewed. Two previously stented ICAs were excluded from analysis. On MDCTA, 7 ICAs were occluded, 12 ICAs presented with and 63 without a high-grade ICA stenosis (70–99 %). For detecting 70–99 % stenosis, both 3D TOF-MRA and CE-MRA were 91.7 % sensitive and 98.5 % specific, respectively. Both MRA techniques were highly sensitive (100 %), and specific (CE-MRA, 100 %; TOF-MRA, 98.7 %) for the detection of ICA occlusion. However, TOF-MRA misclassified one high-grade stenosis as occlusion. Intermodality agreement for detection of 70–99 % ICA stenoses was excellent between TOF-MRA and CE-MRA [κ = 0.902, 95 % confidence interval (CI) = 0.769–1.000], TOF-MRA and MDCTA (κ = 0.902, 95 % CI = 0.769–1.000), and CE-MRA and MDCTA (κ = 0.902, 95 % CI = 0.769–1.000).
Conclusion
Both 3D TOF-MRA and CE-MRA at 3 T are reliable tools for detecting high-grade proximal ICA stenoses (70–99 %). 3D TOF-MRA might misclassify pseudo-occlusions as complete occlusions. If there are no contraindications for CE-MRA, CE-MRA is recommended as primary MR imaging modality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The accurate diagnosis of steno-occlusive disease of the internal carotid artery (ICA) is essential for determining the appropriate therapeutic intervention for primary and secondary stroke prevention [1–4]. In the multidisciplinary German–Austrian guideline of the diagnosis, treatment, and follow-up of extracranial carotid stenoses, Doppler and color-coded duplex sonography are considered the most important non-invasive imaging modalities. Computed tomography angiography (CTA) and magnetic resonance angiography (MRA) serve as complementary imaging modalities [5]. Invasive catheter angiography [digital subtraction angiography (DSA)] is only indicated in exceptional cases, e.g., significantly differing stenosis grade by two non-invasive techniques [5–8].
Multidetector CT angiography (MDCTA) is an accurate tool to determine the degree of carotid artery stenosis [9–17]. In a systematic review, Hollingworth et al. [18] reported on a sensitivity and specificity of CTA of 95 and 98 %, respectively. Excellent sensitivities (100–95 %) and specificities (93–98 %) or excellent agreement with DSA were also reported by various other authors [17, 19–21]. Most recently, Anzidei et al. [22] compared MDCTA with colour Doppler ultrasonography and contrast-enhanced MRA (CE-MRA) using DSA as reference standard and found MDCTA the most accurate technique to evaluate carotid artery stenoses (accuracy, 97 %; sensitivity, 95 %; and specificity, 99.8 %).
Among the MRA techniques, CE-MRA and time-of-flight MRA (TOF-MRA) reliably determine the degree of carotid artery stenoses at 1.5 T [23–30]. Although some studies have been published with regard to plaque imaging, no study compared TOF-MRA and CE-MRA at 3 T so far.
The aim of the present study was to compare the accuracy of CE-MRA and 3D TOF-MRA at 3 T for the detection of proximal high-grade ICA stenosis (70–99 %) using MDCTA as reference standard.
Subjects and Methods
Patients
This prospective study was approved by our institutional ethics committee, and informed consent was obtained before MRA and CTA imaging in all patients enrolled. We included 41 patients with different grades of proximal ICA stenosis detected on duplex ultrasonography before scheduled percutaneous transluminal coronary angioplasty.
Patients’ presentation included history of stroke (n = 11) and transient ischemic attack (n = 2). On duplex ultrasonography, 25 patients had a unilateral 50–100 % and 16 patients had bilateral 50–100 % stenosis of the ICA.
MR Imaging
MR imaging was performed on a 3-T whole-body MR imaging system (Magnetom Trio; Siemens Medical Solutions, Erlangen, Germany) with a fast gradient system (peak gradient amplitude, 40 mT/m; maximum slew rate, 200 mT/m/ms) using a head and neck array coil.
3D-TOF-MRA
The 3D volume was positioned in an axial orientation at the level of the carotid bifurcation with the following imaging parameters: repetition time (TR), 20 ms; echo time (TE), 3.69 ms; bandwidth, 250 Hz/pixel; flip angle, 25°; field of view, 149 × 199 mm2; matrix size, 384 × 288; slice thickness, 1 mm; and number of partitions, 52. Partial Fourier of 6/8 was applied in partition direction. Parallel image acquisition using GRAPPA (Generalized Autocalibrating Partially Parallel Acquisition) algorithm was applied with an acceleration factor of 2 and 24 reference k-space lines. We used two slabs to cover the carotid bifurcation and the extracranial ICA. Voxel dimensions were 0.8 × 0.5 × 1.0 mm, and the acquisition time was 3 min and 13 s.
CE-MRA
CE-MRA was performed in the coronal plane immediately after 3D TOF-MRA. Contrast material (Multihance, Bracco Imaging, Konstanz, Germany) was injected via the ante-cubital vein with a power injector (Spectris Solaris EP, MEDRAD Inc., Warrendale, PA) at a rate of 2.5 ml/s followed by a saline (0.9 %) bolus of 30 ml at 2.5 ml/s. Circulation time was measured with a test bolus of 3 ml. The contrast agent was given at a dose of 0.2 ml/kg bodyweight. The 3D volume was acquired with the following imaging parameters: TR, 3.1 ms; TE, 1.21 ms; bandwidth, 651 Hz/pixel; flip angle, 20°; field-of-view, 225 × 300 mm2; matrix size, 384 × 512; slice thickness, 0.8 mm; with 88 partitions, yielding in spatial resolution of 0.8 × 0.6 × 0.8 mm. Partial Fourier was applied at 6/8 in partition as well as in phase direction. Parallel image acquisition using the GRAPPA algorithm was applied with an acceleration factor of 2 and 24 reference k-space lines. The acquisition time was 20 s.
CTA
Having the high accuracy of MDCTA and the possible technical impairment of DSA in mind [31, 32] and knowing the stroke risk [33–40] and the average applied radiation dose of DSA [41–43], we decided not to expose our patients to any additional harm, and therefore use MDCTA instead of DSA as our reference standard. Furthermore, it would have been very difficult to obtain an approval by the ethics committee for a DSA study with our aforementioned patient population, as DSA is not generally indicated in patients with ICA stenoses.
MDCTA acquisition was performed on a 16-section multidetector CT scanner (Sensation 16, Siemens Medical Solutions, Erlangen, Germany). Contrast bolus tracking was performed after contrast administration of Solutrast 300 (Bracco Imaging, Konstanz, Germany), 95 ml at 5 ml/s, followed by a bolus of normal saline (0.9 %), 40 ml at 5 ml/s, via an intravenous 18-gauge needle. An ROI was placed in the ascending aorta, and scanning was initiated by a measured HU (Houndsfield Units) difference of 100 (delay, 3 s). The following parameters were used: 120 kV, 130 mAs (CARE Dose 4D protocol), 0.5-s rotation time, and 1-mm section thickness reconstructed at 0.7-mm intervals. Voxel size was 0.75 × 0.75 × 0.7 mm3. Images were obtained from the aortic arch (level of tracheal bifurcation) to the vertex through to the circle of Willis. Afterward, axial source images were reconstructed and sent to a Syngo 3D work station (Siemens Medical Solutions, Erlangen, Germany) to generate standardized 3D MIP (Maximum Intensity Projection) reformations (coronal and sagittal oblique on both carotid bifurcations).
Image Analysis
Image data were sent to a dedicated workstation (Impax, Agfa-Gevaert, Mortsel, Belgium). CE-MRA, 3D TOF-MRA, and MDCTA images were reviewed separately in different reading sessions by two independent readers (X.X. and X.Y., with 12 and 7 years of experience in neuroimaging, respectively). Vessel diameters were determined on multiplanar reconstructions in the axial plane perpendicular to the axis of the vessel. The degree of ICA stenosis was calculated according to the North American Symptomatic Carotid Endarterectomy Trial using the following equation: Degree of carotid stenosis in percentage = (1 − diameter of minimal residual lumen [mm]/diameter of distal ICA lumen [mm]). The degree of stenosis was categorized as 0–25 % (minimal), 25–50 % (mild), 50–69 % (moderate), 70–99 % (high grade), and 100 % (occlusion).
Statistical Analysis
Analyses were performed with SAS 9.2 (SAS Institute Inc., Cary, NC). Sensitivity and specificity were calculated considering MDCTA as a reference standard, and are presented with exact 95 % confidence intervals (CIs) derived from the binomial distribution. The level of intermodality agreement were determined with respect to the detection of complete occlusions and high-grade stenoses (70–99 %) by calculating the κ coefficient (κ < 0.20 indicated poor agreement; κ = 0.21–0.40, fair agreement; κ = 0.41–0.60, moderate agreement; κ = 0.61–0.80, good agreement; κ = 0.81–0.90, very good agreement; and κ > 0.90, excellent agreement).
Results
Demographics
The study group comprised 41 patients (14 females and 27 males) with a mean age of 72 [standard deviation (SD), ± 8; range, 50–88] years. In all patients, CE-MRA and 3D TOF-MRA were performed during the same imaging session. In 38 cases, MDCTA was performed before or on the same day of the MRA study; 3 patients received MDCTA 3, 5, and 8 days after MRA, respectively. On average, MDCTA was performed 3.2 (SD, ± 9.7; range, − 42 to 8) days before MRA. Two patients previously had unilateral ICA stenting for high-grade ICA stenosis. These vessels were excluded from analysis. Overall, we included 80 vessels of 41 patients in our study, of which 58 were suspicious of having at least a ≥ 50 % carotid stenosis on duplex sonography.
Stenosis Scores by Technique
Mean grade of stenoses on MDCTA, the reference standard of our study, was 44 % (SD, ± 921.7 %; range, 0–100 %). Mean grade of stenoses on 3D TOF-MRA was 43 % (SD, ± 22.3 %; range, 0–100 %). On CE-MRA, the mean grade of stenoses was 44 % (SD, ± 22.6 %; range, 0–100 %). The categorized grades of ICA stenoses and their distribution are displayed in Table 1. A sample carotid stenosis ≥ 70 % determined by 3D TOF-MRA, CE-MRA, and MDCTA is shown in Fig. 1.
Case example: 88-year-old female patient with a left-sided internal carotid artery (ICA) stenosis. The stenosis (arrow) of the left ICA was rated by the observers to be high grade (70–99 %) in all three imaging techniques: 3D time-of-flight magnetic resonance angiography (a), contrast-enhanced magnetic resonance angiography (b), and multidetector computed tomography angiography (c) in sagittal reconstructions. The arrowhead indicates calcifications within the stenotic plaque (c)
Sensitivity and Specificity
The grades of ICA stenoses determined by MDCTA were considered the reference for the calculation of the sensitivity and specificity of 3D TOF-MRA and CE-MRA.
The sensitivity and specificity for the detection of ICA occlusions were 100 % (95 % CI, 0.646–1.000) and 98.7 % (95 % CI, 0.927–0.998 %) for 3D TOF-MRA and 100 % (95 % CI, 0.646–1.000) and 100 % (95 % CI, 0.951–1.000) for CE-MRA, respectively. All true occlusions have been detected by both MRA techniques. One high-grade stenosis was misclassified by 3D TOF-MRA as occlusion (Fig. 3).
The sensitivity and specificity for detection of high-grade ICA stenoses (70–99 %) in 80 vessels were 91.7 % (95 % CI, 0.646–0.985) and 98.5 % (95 % CI, 0.921–0.997), respectively, for both 3D TOF-MRA and CE-MRA. Case examples of incongruent findings are displayed in Figs. 2 and 3.
Case example: 79-year-old male patient with a right-sided internal carotid artery (ICA) stenosis. Sagittal reconstructions of the 3D time-of-flight magnetic resonance angiography (TOF-MRA; a), contrast-enhanced magnetic resonance angiography (CE-MRA; b), and multidetector computed tomography angiography (MDCTA; c) show the stenotic ICA (arrows). On 3D TOF-MRA and MDCTA, the stenosis was considered high grade (80 and 75 % according to the North American Symptomatic Carotid Endarterectomy Trial criteria, respectively). The degree of stenosis calculated on the basis of the CE-MRA was 62 %. Arrowhead indicates calcifications within the stenotic vessel segment
Case example: 74-year-old male patient with a right-sided internal carotid artery (ICA) stenosis. Sagittal reconstructions of the 3D time-of-flight magnetic resonance angiography (a) show an absence of flow signal along the course of the ICA. On contrast-enhanced magnetic resonance angiography (CE-MRA; b) and multidetector computed tomography angiography (MDCTA; c), the post-stenotic ICA is clearly shown (arrow). The degree of stenoses (North American Symptomatic Carotid Endarterectomy Trial) for CE-MRA and MDCTA were 76 and 74 %, respectively
Intermodality Agreement
Intermodality agreement for the detection of an ICA occlusion was excellent. For the agreement between 3D TOF-MRA and CE-MRA, κ-value was 0.926 (CI = 0.709–1.000); for 3D TOF-MRA and MDCTA, it was 0.926 (CI = 0.738–1.000); and for CE-MRA and MDCTA, it was 1.000 (CI = 1.000–1.000).
Intermodality agreement for detection of high-grade ICA stenoses (70–99 %) was excellent between 3D TOF-MRA and CE-MRA (κ = 0.902, 95 % CI = 0.769–1.000), 3D TOF-MRA and MDCTA (κ = 0.902, 95 % CI = 0.769–1.000), and CE-MRA and MDCTA (κ = 0.902, 95 % CI = 0.769–1.000).
Discussion
MRA at 3 T, no matter whether as 3D TOF-MRA or CE-MRA, is very sensitive and specific in detecting high-grade ICA stenoses (70–99 %) and occlusions when compared with MDCTA, serving as reference standard. However, on 3D TOF-MRA, pseudo-occlusions may be misinterpreted as occlusions.
There is ongoing discussion as to which MRA technique is more accurate in depicting proximal carotid artery stenoses. Willinek et al. [28] reported on a sensitivity of 100 % and a specificity of 99.3 % in detecting 70–90 % stenoses with 1.5-T CE-MRA. Fellner et al. [44] found a sensitivity of 100 % for both CE-MRA and TOF-MRA. Specificity of TOF-MRA was superior to CE-MRA (96.7 versus 80.6 %). Babiarz et al. compared 1.5-T CE-MRA and 2D TOF-MRA to detect ≥ 70 % ICA stenosis and found CE-MRA to be more sensitive (84 versus 80 % for 2D TOF-MRA). Specificity was high for both techniques (96 % for CE-MRA and 95 % for 2D TOF-MRA). They concluded that the administration of gadolinium did not offer a significant advantage in distinguishing surgically treatable ICA stenosis [30]. In their meta-analysis, Chapell et al. [45] found CE-MRA as the most accurate non-invasive imaging technique for the detection of 70–99 % stenosis, with a reported sensitivity and specificity of both 85 %. Anzidei et al. described a sensitivity of 88 % and specificity of 95 % for CE-MRA at 1.5 T. Higher accuracy values are likely related to the improvement of coils and imaging sequences, including intelligent k-space sampling. Only if operated as a steady-state CE-MRA with an increased spatial resolution (0.7 × 0.7 × 0.7 mm3), it was possible to achieve a very good sensitivity (93 %) and an almost perfect specificity 97 % [22].
With a higher signal-to-noise ratio (SNR) using an eight-channel head and neck coil at 3 T, even higher accuracy values for 3D TOF and CE-MRA seem reasonable. DeMarco et al. [46] already found 3-T TOF-MRA superior to 1.5-T TOF-MRA due to an increased SNR and contrast-to-noise ratio.
Our data suggest that 3D TOF-MRA and CE-MRA both reliably detect high-grade (70–99 %) ICA stenoses at 3 T. In our study, sensitivities and specificities were 91.7 and 98.5 %, respectively, for both 3D TOF-MRA and CE-MRA.
A well-known limitation of 3D TOF-MRA is the misclassification of pseudo-occlusions as occlusions. Obviously, this limitation exists also with higher field strengths diminishing the diagnostic value of 3D TOF- in comparison with CE-MRA.
For CE-MRA, we could not prove an obvious benefit in terms of sensitivity and specificity when performed at 3 T. However, total acquisition time decreased and anatomical coverage was larger compared with sequences at 1.5 T.
Coverage from the aortic arch up to the circle of Willis—an important feature when, e.g., planning for stenting of a high-grade ICA stenosis—has to be considered a major advantage of CE-MRA when compared with TOF-MRA. In addition, the shorter acquisition time of CE-MRA allows for a higher spatial resolution focused on the arterial phase of the passage of the contrast agent.
Further potential for improvement is found in the spatial resolution as was shown by Anzidei et al. [22], who increased the sensitivity and specificity of CE-MRA by approximately 5 % when performing a steady-state instead of a first-pass MRA.
For the detection of ICA occlusions, CE-MRA has proven excellent and completely agrees with MDCTA (100 % sensitive and 100 % specific). 3D TOF-MRA shows a sensitivity of 100 % but a lower specificity of 98.7 %. Compared with former studies at 1.5 T, CE-MRA confirmed its already very good diagnostic value for detecting ICA occlusions, while 3D TOF-MRA has even increased its accuracy [1, 23, 25, 28].
We acknowledge the following limitations of this study: first, it was conducted in a single centre. Second, we did not perform DSA but used MDCTA as reference standard. A former limitation of CTA—the existence of calcified plaques—has become less limiting due to the progress in CT hard- and software. That is why MDCTA is now regarded as being able to quantify carotid stenosis with a high accuracy [14, 22]. In addition, DSA alone may result in an underestimation of ICA stenoses compared with rotational angiography [47]. Third, our study population with hemodynamically relevant ICA stenoses was small, leading to wide 95 % CIs. This was due to patient selection, consisting only of patients who had a borderline high-grade ICA stenosis. Further studies with a larger population are needed to confirm the high quality of 3-T TOF-MRA and CE-MRA with a greater precision.
Conclusion
Both 3D TOF-MRA and CE-MRA at 3 T are reliable tools for detecting high-grade extracranial ICA stenoses (70–99 %). 3D TOF-MRA might misclassify pseudo-occlusions as complete occlusions. If there are no contraindications for CE-MRA, it is recommended as primary MR imaging modality.
Abbreviations
- CCA:
-
Common carotid artery
- CE-MRA:
-
Contrast-enhanced magnetic resonance angiography
- CI:
-
Confidence interval
- CNR:
-
Contrast-to-noise ratio
- DSA:
-
Digital subtraction angiography
- GRAPPA:
-
Generalized Autocalibrating Partially Parallel Acquisition
- HU:
-
Houndsfield Units
- ICA:
-
Internal carotid artery
- MDCTA:
-
Multidetector CTA
- MIP:
-
Maximum Intensity Projection
- NASCET:
-
North American Symptomatic Carotid Endarterectomy Trial
- ROI:
-
Region of interest
- SNR:
-
Signal-to-noise ratio
- TOF-MRA:
-
Time-of-flight magnetic resonance angiography
References
Debrey SM, Yu H, Lynch JK, Lövblad KO, Wright VL, Janket SJ, et al. Diagnostic accuracy of magnetic resonance angiography for internal carotid artery disease: a systematic review and meta-analysis. Stroke. 2008;39:2237–48.
Barnett HJ, Taylor DW, Eliasziw M. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. NASCET Collaborators. N Engl J Med. 1998;339:1415–25.
North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1991;325:445–53.
MRC European Carotid Surgery Trial. Interim results for symptomatic patients with severe (70–99 %) or with mild (0–29 %) carotid stenosis. European Carotid Surgery Trialists’ Collaborative Group. Lancet. 1991;337:1235–43.
Eckstein HH, Kühnl A, Dörfler A, opp IB, Lawall H, Ringleb PA. Clinical practical guideline: the diagnosis, treatment, and follow-up of extracranial carotid stenosis—a multidisciplinary German-Austrian guideline based on evidence and consensus. Dtsch Arztebl Int. 2013;110:468–76.
Boehm G. Praeinterventionelle Diagnostik vor Karotisstenting. Z Gefässmed. 2008;5(4):12–20.
Jaff MR. Imaging the carotid bifurcation: toward standardization. Semin Vasc Surg. 2008;21:73–9.
Lanzino G, Tallarita T, Rabinstein AA. Internal carotid artery stenosis: natural history and management. Semin Neurol. 2010;30:518–27.
Saba L, Sanfilippo R, Pirisi R, Pascalis L, Montisci R, Mallarini G. Multidetector-row CT angiography in the study of atherosclerotic carotid arteries. Neuroradiology. 2007;49:623–37.
Yoon DY, You SY, Choi CS, Chang SK, Yun EJ, Seo YL, et al. Multi-detector row CT of the head and neck: comparison of different volumes of contrast material with and without a saline chaser. Neuroradiology. 2006;48:935–42.
Bartlett ES, Walters TD, Symons SP, Fox AJ. Carotid stenosis index revisited with direct CT angiography measurement of carotid arteries to quantify carotid stenosis. Stroke. 2007;38:286–91.
Borisch I, Boehme T, Butz B, Hamer OW, Feuerbach S, Zorger N. Screening for carotid injury in trauma patients: image quality of 16-detector-row computed tomography angiography. Acta Radiol. 2007;48:798–805.
de Monye C, de Weert TT, Zaalberg W, Cademartiri F, Siepman DA, Dippel DW, et al. Optimization of CT angiography of the carotid artery with a 16-MDCT scanner: craniocaudal scan direction reduces contrast material-related perivenous artifacts. AJR Am J Roentgenol. 2006;186:1737–45.
Bartlett ES, Walters TD, Symons SP, Fox AJ. Quantification of carotid stenosis on CT angiography. AJNR Am J Neuroradiol. 2006;27:13–9.
Koelemay MJ, Nederkoorn PJ, Reitsma JB, Majoie CB. Systematic review of CTA for assessment of carotid artery disease. Stroke. 2004;35:2306–12.
Lell M, Fellner C, Baum U, Hothorn T, Steiner R, Lang W, et al. Evaluation of carotid artery stenosis with multisection CT and MR imaging: influence of imaging modality and postprocessing. AJNR Am J Neuroradiol. 2007;28:104–10.
Silvennoinen HM, Ikonen S, Soinne L, Railo M, Valanne L. CT angiographic analysis of carotid artery stenosis: comparison of manual assessment, semiautomatic vessel analysis, and digital subtraction angiography. AJNR Am J Neuroradiol. 2007;28:97–103.
Hollingworth W, Nathens AB, Kanne JP, Crandall ML, Crummy TA, Hallam DK, et al. The diagnostic accuracy of computed tomography angiography for traumatic or atherosclerotic lesions of the carotid and vertebral arteries: a systematic review. Eur J Radiol. 2003;48:88–102.
Lell M, Anders K, Leidecker C, Lang W, Bautz W, Uder M. CTA of carotid artery with different scanner types. Radiologe. 2004;44:967–74.
Leclerc X, Godefroy O, Pruvo JP, Leys D. Computed tomographix angiography for the evalutation of carotid artery stenosis. Stroke. 1995;26:1577–81.
Puchner S, Popovic M, Wolf F, Reiter M, Lammer J, Bucek RA. Multidetector CTA in the quantification of internal carotid artery stenosis: value of different reformation techniques and axial source images compared with selective carotid arteriography. J Endovasc Ther. 2009;16:336–42.
Anzidei M, Napoli A, Zaccagna F, Di Paolo P, Saba L, Cavallo Marincola B, et al. Diagnostic accuracy of colour Doppler ultrasonography, CT angiography and blood-pool-enhanced MR angiography in assessing carotid stenosis: a comparative study with DSA in 170 patients. Radiol Med. 2012;117:54–71.
Remonda L, Heid O, Schroth G. Carotid artery stenosis, occlusion, and pseudo-occlusion: first-pass, gadolinium-enhanced, three-dimensional MR angiography—preliminary study. Radiology. 1998;209:95–102.
Sundgren PC, Sundén P, Lindgren A, Lanke J, Holtås S, Larsson EM. Carotid artery stenosis: contrast-enhanced MR angiography with two different scan times compared with digital subtraction angiography. Neuroradiology. 2002;44:592–9.
Remonda L, Senn P, Barth A, Arnold M, Lövblad KO, Schroth G. Contrast-enhanced 3D MR angiography of the carotid artery: comparison with conventional digital subtraction angiography. AJNR Am J Neuroradiol. 2002;23:213–9.
Cosottini M, Pingitore A, Puglioli M, Michelassi MC, Lupi G, Abbruzzese A, et al. Contrast-enhanced three-dimensional magnetic resonance angiography of atherosclerotic internal carotid stenosis as the noninvasive imaging modality in revascularization decision making. Stroke. 2003;34:660–4.
Borisch I, Horn M, Butz B, Zorger N, Draganski B, Hoelscher T, et al. Preoperative evaluation of carotid artery stenosis: comparison of contrast-enhanced MRA and duplex sonography with digital subtraction angiography. AJNR Am J Neuroradiol. 2003;24:1117–22.
Willinek WA, von Falkenhausen M, Born M, Gieseke J, Höller T, Klockgether T, et al. Noninvasive detection of steno-occlusive disease of the supra-aortic arteries with three-dimensional contrast-enhanced magnetic resonance angiography: a prospective, intra-individual comparative analysis with digital subtraction angiography. Stroke. 2005;36:38–43.
Barth A, Arnold M, Mattle HP, Schroth G, Remonda L. Contrast-enhanced 3-D MRA in decision making for carotid endarterectomy: a 6-year experience. Cerebrovasc Dis. 2006;21:393–400.
Babiarz LS, Romero JM, Murphy EK, Brobeck B, Schaefer PW, González RG, et al. Contrast-enhanced MR angiography is not more accurate than unenhanced 2D time-of-flight MR angiography for determining ≥ 70 % internal carotid artery stenosis. AJNR Am J Neuroradiol. 2009;30:761–8.
Elgersma OE, Buijs PC, Wüst AF, van der Graaf Y, Eikelboom BC, Mali WP. Maximum internal carotid arterial stenosis: assessment with rotational angiography versus conventional intraarterial digital subtraction angiography. Radiology. 1999;213:777–83.
Anazalone N, Scomazzoni F, Catellano R, Strada L, Righi C, Politi LS, et al. Carotid artery stenosis: intraindividual correlations of 3D time-of-flight MR angiography, contrast-enhanced MR angiography, conventional DSA, and rotational angiography for detection and grading. Radiology. 2005;236:204–13.
Heiserman JE, Dean BL, Hodak JA, Flom RA, Bird CR, Drayer BP, et al. Neurologic complications of cerebral angiography. AJNR Am J Neuroradiol. 1994;15:1401–7.
Cloft HJ, Joseph GJ, Dion JE. Risk of DSA in patients with SAH, cerebral aneurysm, and AVM: a meta-analysis. Stroke. 1999;30:317–20.
Willinsky RA, Taylor SM, TerBrugge K, Farb RI, Tomlinson G, Montanera W. Neurologic complications of cerebral angiography: prospective analysis of 2,899 procedures and review of the literature. Radiology. 2003;227:522–8.
Kaufmann TJ, Huston J 3rd, Mandrekar JN, Schleck CD, Thielen KR, Kallmes DF. Complications of diagnostic cerebral angiography: evaluation of 19,826 consecutive patients. Radiology. 2007,243(3):812–9.
Burger IM, Murphy KJ, Jordan LC, Tamargo RJ, Gailloud P. Safety of cerebral digital subtraction angiography in children: complication rate analysis in 241 consecutive diagnostic angiograms. Stroke. 2006;37:2535–9.
Maldonado TS. What are current preprocedure imaging requirements for carotid artery stenting and carotid endarterectomy: have magnetic resonance angiography and computed tomographic angiography made a difference? Semin Vasc Surg. 2007;20:205–15.
Connors JJ 3rd, Sacks D, Furlan AJ, Selman WR, Russell EJ, Stieg PE, et al. Training, competency, and credentialing standards for diagnostic cervicocerebral angiography, carotid stenting, and cerebrovascular intervention: a joint statement from the American Academy of Neurology, the American Association of Neurological Surgeons, the American Society of Interventional and Therapeutic Neuroradiology, the American Society of Neuroradiology, the Congress of Neurological Surgeons, the AANS/CNS Cerebrovascular Section, and the Society of Interventional Radiology. J Vasc Interv Radiol. 2004;15:1347–56.
Cloft HJ, Joseph GJ, Dion JE. Risk of cerebral angiography in patients with subarachnoid hemorrhage, cerebral aneurysm, and arteriovenous malformation: a meta-analysis. Stroke. 1999;30:317–20.
Feygelman VM, Huda W, Peters KR. Effective dose equivalents to patients undergoing cerebral angiography. AJNR Am J Neuroradiol. 1992;13:845–9.
Gkanatsios NA, Huda W, Peters KR. Adult patient doses in interventional neuroradiology. Med Phys. 2002;29:717–23.
Topaltzikis T, Rountas C, Fezoulidis I, Kappas C, Theodorou K. In vivo dosimetry during DSA of the carotid and renal arteries. Derivation of local DRLs. Phys Med. 2009;25:166–71.
Fellner C, Lang W, Janka R, Wutke R, Bautz W, Fellner FA. Magnetic resonance angiography of the carotid arteries using three different techniques: accuracy compared with intraarterial x-ray angiography and endarterectomy specimens. J Magn Reson Imaging. 2005;21:424–31.
Chappell FM, Wardlaw JM, Young GR, Gillard JH, Roditi GH, Yip B, et al. Carotid artery stenosis: accuracy of noninvasive tests—individual patient data meta-analysis. Radiology. 2009;251:493–502.
DeMarco JK, Huston J 3rd, Nash AK. Extracranial carotid MR imaging at 3T. Magn Reson Imaging Clin N Am. 2006;14:109–21.
Anzalone N, Scomazzoni F, Castellano R, Strada L, Righi C, Politi LS, et al. Carotid artery stenosis: intraindividual correlations of 3D time-of-flight MRA, contrast-enhanced MRA, conventional DSA, and rotational angiography for detection and grading. Radiology. 2005;236:204–13.
Conflict of Interest
The authors declare that there are no actual or potential conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Weber, J., Veith, P., Jung, B. et al. MR Angiography at 3 Tesla to Assess Proximal Internal Carotid Artery Stenoses: Contrast-Enhanced or 3D Time-of-Flight MR Angiography?. Clin Neuroradiol 25, 41–48 (2015). https://doi.org/10.1007/s00062-013-0279-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-013-0279-x