Abstract
Background
Systemic sclerosis (SSc) is a systemic connective tissue disease and cardiac involvement is one of the most important causes of death. Right ventricular (RV) systolic dysfunction is a poor prognostic finding in SSc patients. Assessment of RV function has some difficulties because of its crescent shape and extensive trabeculations. Two-dimensional (2D) speckle-tracking echocardiography (STE) is an angle-independent quantitative technique to evaluate myocardial function. The aim of this study was to assess the RV and right atrial (RA) functions of SSc patients without pulmonary hypertension by using 2D STE.
Patients and methods
A total of 40 patients with SSc (mean age 48.5 ± 11.4 years, 28 female) and 40 healthy volunteers (mean age 45.9 ± 7.6 years, 21 female) were included in the study. All subjects underwent transthoracic echocardiography for evaluation of RV and RA functions with 2D STE.
Results
Although left ventricular systolic and diastolic functions, systolic pulmonary artery pressure (PAP), and RA measurements were similar in both groups, tricuspid annular plane systolic excursion (TAPSE) and maximum systolic myocardial velocity (S’) were decreased in SSc patients. The RV free wall global longitudinal strain (GLS) of SSc patients was lower than the controls (− 18.5 ± 4.9 % vs. − 21.8 ± 2.4 %, p < 0.001) and the RA reservoir and conduit functions were also decreased in SSc patients compared with controls (34.4 ± 9.9 % vs. 39.7 ± 11.2 %, p = 0.027 and 15.0 ± 5.7 % vs. 18.7 ± 6.4 %, p = 0.009, respectively). Disease duration was inversely correlated with RVGLS and TAPSE (r: − 0.416, p = 0.018 and r: − 0.383, p = 0.031, respectively).
Conclusion
The use of 2D STE can be helpful in the detection of impairment in RV and RA functions in SSc patients with normal PAP.
Zusammenfassung
Hintergrund
Die systemische Sklerose (SSc) ist eine systemische Bindegewebserkrankung, und die Herzbeteiligung stellt eine der Haupttodesursachen dar. Eine rechtsventrikuläre (RV) systolische Funktionseinschränkung ist ein Befund, der bei SSc-Patienten für eine schlechte Prognose steht. Die Untersuchung der RV-Funktion ist aufgrund der Halbmondform und ausgedehnter Trabekulierungen des RV schwierig. Die zweidimensionale (2-D-)Speckle-Tracking-Echokardiographie (STE) ist eine winkelunabhänigige quantitative Untersuchungstechnik für die Myokardfunktion. Ziel dieser Studie war es, die Funktion des RV und des rechten Vorhofs (RA) bei SSc-Patienten ohne pulmonale Hypertonie mittels 2-D-STE zu ermitteln.
Patienten und Methoden
In die Studie wurden 40 Patienten mit SSc (Durchschnittsalter: 48,5 ± 11,4 Jahre, 28 w) und 40 gesunde Kontrollen (Durchschnittsalter: 45,9 ± 7,6 Jahre, 21 w) aufgenommen. Bei allen Teilnehmern wurden die RV- und RA-Funktion mittels transthorakaler Echokardiographie in Kombination mit 2-D-STE untersucht.
Ergebnisse
Die linksventrikuläre systolische und diastolische Funktion, der systolische Pulmonalarteriendruck (PAP) und die RA-Messungen waren in beiden Gruppen zwar ähnlich, aber die systolische Exkursion auf der Ebene des Trikuspidalrings (TAPSE) und die maximale systolische Myokardgeschwindigkeit (S‘) waren bei SSc-Patienten vermindert. Der globale longitudinale Strain (GLS) der freien RV-Wand war bei SSc-Patienten geringer als bei den Kontrollen (− 18,5 ± 4,9 % vs. − 21,8 ± 2,4 %; p < 0,001) und auch die Reservoir- und Conduitfunktion war bei den SSc-Patienten gegenüber den Kontrollen vermindert (34,4 ± 9,9 % vs. 39,7 ± 11,2 %; p = 0,027 bzw. 15,0 ± 5,7 % vs. 18,7 ± 6,4 %; p = 0,009). Die Krankheitsdauer stand in inverser Korrelation mit dem RV-GLS und TAPSE (r − 0,416; p = 0,018 bzw. r − 0,383; p = 0,031).
Schlussfolgerung
Der Einsatz der 2-D-STE könnte zur Erkennung einer Einschränkung der RV- und RA-Funktion bei SSc-Patienten mit normalem PAP von Nutzen sein.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Systemic sclerosis (SSc) is a systemic connective tissue disease characterized by chronic inflammation, fibrosis, and autoimmunity [1]. Excessive fibrosis can affect visceral organ systems such as the heart and lungs and cardiac involvement of SSc patients is one of the most important causes of death [2]. Cardiac manifestations include pulmonary hypertension (PH) and right ventricular (RV) failure secondary to PH in patients with SSc. Although RV impairment is generally related to elevated pulmonary artery pressure (PAP), RV impairment can sometimes be observed in patients with normal PAP due to ongoing ischemic episodes related to vascular lesions [3]. Therefore, detection of RV systolic impairment before the development of PH in SSc patients might be useful in clinical follow-up. Two-dimensional (2D) speckle tracking echocardiography (STE) is a new angle-independent quantitative technique to evaluate the myocardial function by analyzing spots on the 2D grayscale ultrasound images of the myocardium [4]. In previous studies a correlation between 2D STE and conventional echocardiographic parameters was shown in detecting RV systolic dysfunction [5]. The aim of the present study was to assess the RV and right atrial (RA) functions of SSc patients without PH by using 2D STE.
Methods
Study population
In this study 49 patients with SSc followed up by the Department of Rheumatology were evaluated for enrollment between May 2012 and September 2012. The diagnosis of patients with SSc was based on the American Rheumatism Association (ARA) criteria [6]. Patients with coronary artery disease, valvular heart disease, cardiomyopathy, arrhythmias or conduction disorders, left ventricular (LV) systolic dysfunction with LV ejection fractions (LVEF) < 55 %, significant pulmonary arterial hypertension (systolic pulmonary artery pressure > 35 mmHg), chronic obstructive pulmonary disease, asthma, hypertension, and diabetes mellitus were excluded. After exclusion criteria were applied, 40 patients with SSc were included in the study and 40 age- and sex-matched healthy volunteers were included as a control group. The investigation complied with the principles outlined in the Declaration of Helsinki. The study was approved by the local ethics committee and all participants gave written informed consent before participating.
Standard echocardiography and 2D speckle tracking echocardiography
Conventional standard echocardiographic examination of patients was performed by using a commercially available echocardiography device (Vivid 7, GE Vingmed Ultrasound AS, Horten, Norway). Echocardiographic data were obtained with a 3.5 -MHz transducer at a depth of 16 cm in the parasternal and apical views during breath hold, stored in cine loop format from three consecutive beats, and transferred to a workstation for further offline analysis (EchoPAC 6.1; GE Vingmed Ultrasound AS). Gain settings, filters, and pulse repetitive frequency were adjusted to optimize color saturation, and a color Doppler frame scanning rate of 100–140 Hz was used for color tissue Doppler images (TDI). Cardiac dimensions were measured according to the guidelines of the American Society of Echocardiography (ASE) and LVEF was calculated by the biplane Simpson’s method [7]. The LV end diastolic diameter (EDD), LV end systolic diameter (ESD), left atrial area (LAA), mitral inflow early (E wave) and late (A wave) diastolic velocities, deceleration time of early diastolic velocity and early (E’ wave) and late (A’ wave) diastolic annular velocities assessed at the septal mitral annulus, deceleration time (DT), and the E/E’ ratio were used in the analysis. Diastolic dysfunction was defined as a tissue Doppler lateral E’ velocity of less than 10 cm/s. Right ventricular and atrial dimensions were measured as suggested in the ASE guidelines [4]. RV function was also evaluated according to the guidelines of the ASE by using tricuspid annular plane systolic excursion (TAPSE), maximal systolic myocardial velocity (S’) measured with TDI and fractional area change (FAC). Systolic pulmonary artery pressure (sPAP) was calculated by measuring the peak systolic gradient from the peak velocity of the continuous-wave Doppler of the tricuspid regurgitation jet by using the Bernoulli equation.
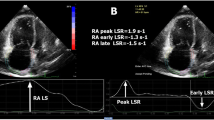
The speckles, natural acoustic markers equally distributed throughout the myocardium, can be detected and tracked on the standard grayscale 2D images. Myocardial strain can be calculated by measuring the change of the position of the speckles within a myocardial segment along the cardiac cycle. The assessment of global radial strain (GRS) and global circumferential strain (GCS) of the LV were performed by applying 2D speckle tracking imaging to the parasternal short-axis views of the LV. The midventricular short axis of the LV was divided into six segments, and the values of GRS and GCS were derived from the average of the six segmental peak systolic strain values. The assessment of global longitudinal peak systolic strain was performed by applying 2D speckle tracking imaging to the apical four-chamber views of the LV. The LV was divided into six segments in apical view. The values of global longitudinal strain (GLS) were derived from the average of the six segmental peak systolic longitudinal strain values. The RV strain was also assessed using 2D speckle tracking imaging as previously described from the apical four-chamber view [8] and The RV basal lateral and midlateral wall endocardial borders were manually traced at the end systolic frame. The epicardial border was traced automatically by software (Fig. 1). If necessary, to obtain optimal tracking the region of interest (ROI) was modified by the observer. The RVGLS was derived from the average of these two segments.
For the RA speckle tracking analysis, RA-focused images in apical four-chamber view were obtained. A minimum frame rate of 40 frames per second was required for the reliable operation of this program. For 2D speckle tracking strain analysis, a line was manually drawn along the RA endocardial border of the apical four-chamber view after contraction (Fig. 1), when the RA was at its minimum volume, using the point-and-click approach as previously described [9, 10]. The software then automatically generated additional lines near the atrial epicardium and mid-myocardial line, with the narrowest ROI. The ROI then included the entire RA myocardial wall and was adjusted for the thickness. The software generated strain curves for each atrial segment. The value of peak early and late diastolic longitudinal strains was determined as right atrial reservoir (RA Res) and conduit (RA Con) functions.
Statistical analysis
Statistical analyses were performed using the SPSS15.0 statistical package for Windows. Continuous data were expressed as mean ± standard deviation while categorical data were presented as percentages. The χ2 test was used for comparison of categorical variables while Student’s t test or the Mann–Whitney U test was used to compare parametric and nonparametric continuous variables, respectively. For correlation analysis, the Spearman test was used. Intraobserver and interobserver variability was calculated as the absolute difference between two measurements as a percentage of the mean. A value of p < 0.05 was considered statistically significant.
Results
The 40 patients with SSc (mean age 48.5 ± 11.4 years, 28 female) were compared with 40 healthy age- and sex-matched controls (mean age 45.9 ± 7.6 years, 21 female, p = 0.16 and p = 0.10, respectively). Baseline characteristics and clinical data of SSc patients are displayed in Tab. 1.
LV echocardiographic parameters of the SSc patients and healthy controls are compared in Tab. 2. Conventional LV dimensions and EF were similar in both groups. Although LV diastolic dysfunction was observed more commonly in SSc patients than in the control group, it did not reach statistical significance (p = 0.180). We also evaluated LV function by using 2D STE and LVGLS, GRS, and GCS were similar between the two groups (p > 0.05).
Right ventricular and atrial dimensions and functions are shown in Tab. 3. The RV annulus diameter and RV inflow tract diameter were higher in SSc patients compared with controls (p = 0.010 and p = 0.014, respectively). Mean RAA was slightly lower in SSc patients (13 cm2 vs. 14.2 cm2, p = 0.040), but when we normalized to body surface area (BSA), RAA/BSA was similar between the two groups (7.8 ± 1.2 vs. 7.6 ± 1.0, p = 0.470). Although sPAP was within normal limits, the sPAP of SSc patients was slightly higher compared with the controls (24.2 ± 5.7 vs. 19.8 ± 6.2 mmHg, p = 0.002). Evaluation of RV systolic function by TAPSE and RVS’ showed that the RV function of SSc patients was decreased compared with controls (TAPSE 21.1 ± 3.2 vs. 24.3 ± 3.4 mm, p < 0.01 and S’ 10.1 ± 1.5 vs. 12.9 ± 3.0 cm/s, p < 0.001), but the TAPSE and S’ value of SSc patients were nearly normal compared with previous reports. The RVFAC was similar between the two groups (p = 0.300) and RVGLS was significantly decreased in SSc patients compared with the controls (RVGLS − 18.5 ± 4.9 % vs − 21.8 ± 2.4 %, p < 0.001). The RA reservoir and conduit functions were significantly lower than the controls (RA res 34.4 ± 9.9 % vs. 39.7 ± 11.2 %, p = 0.02 and RA con 15.0 ± 5.7 % vs. 18.7 ± 6.4 %, p < 0.01). To evaluate the effect of LV diastolic dysfunction on RV systolic function, we divided the SSc patients into two groups according to the presence of diastolic dysfunction, and found that RV systolic functions were similar between the two groups (Tab. 4). Correlation analysis was performed to evaluate associations between sPAP, RVS, and TAPSE. We did not observe any significant correlation between RVS, TAPSE, and sPAP (p > 0.05 for all). We also analyzed RV function and its relation with disease duration. We demonstrated an inverse correlation between disease duration and RVGLS and TAPSE (r=− 0.41, p = 0.01 and r= − 0.38, p = 0.03, respectively; Fig. 2).
Discussion
In the present study we showed that RV systolic function of the SSc patients without PH was significantly decreased compared with healthy controls by using 2D STE. The RA reservoir and conduit functions were also impaired in SSc patients compared with controls.
SSc is a progressive, systemic disease characterized by inflammation, fibrosis, and autoimmunity [1]. Excessive fibrosis mainly affects the skin and visceral organ systems. In a recently published meta-analysis, the most severe organ complications related with scleroderma involved the heart, lungs, kidneys, muscles, joints, and fingers [11]. Cardiopulmonary involvement was the most important cause of death [2]. Cardiac manifestations were more common in African-Americans, and the 20-year mortality was 32 % [12].
Cardiac manifestations in patients with SSc include LV diastolic and systolic dysfunctions, PH, and RV failure secondary to PH. Although RV impairment is generally related to higher PAP in patients with SSc, RV impairment may be observed in patients without PH. The possible underlying mechanism of impairment of the RV function is myocardial fibrosis secondary to repeated ischemia-reperfusion abnormalities due to vascular lesions in SSc patients [3].
Assessment of RV function in SSc patients by echocardiography has been performed in several studies, but because of the crescent shape and extensive trabeculations of the RV it has some limitations. The most commonly used conventional echocardiographic parameters to evaluated RV function are tissue Doppler-derived peak systolic velocities (S’) and TAPSE [13, 14, 15] and TAPSE could also be used to predict the re-hospitalization rate of SSc patients [15]. A recently published trial on assessment of RV function by using conventional echocardiographic parameters and its correlation with EF measured by magnetic resonance imaging demonstrated that the cut-off values of RVS’ and TAPSE for detection of RVEF < 50 % were 11 cm/s and 17 mm, respectively [14].
Two-dimensional STE is new echocardiographic technique that has been validated in the assessment of LV function by several studies [16, 17, 18, 19, 20] and was also used to evaluate the right side of the heart in various diseases [21, 22, 23, 24]. Meris et al. [5] compared normal subjects with patients who had RV dysfunction, and found that the RV global longitudinal systolic strain cut-off value of −19 % was helpful in distinguishing the two groups. There was limited data about using 2D STE to evaluate RV function in SSc patients. In a previous study reported by Matias et al. [25], the RV basal free wall strain of SSc patients without PH was not different from controls whereas Schattke et al. [26] demonstrated that the RV basal and mid-free wall strain value of SSc patients without PH was lower than controls.
In our study, although RV systolic function of SSc patients without PH was decreased compared with the controls, TAPSE was not lower than previously described cut-off values and S’ and RV GLS were very close to the cut-off value used to distinguish RV failure. One of the possible explanations of these results is that RV failure generally related to increased afterload [27], but in our study patients did not have PH. In addition, another reason for RV failure may be LV diastolic dysfunction but we did not observe any differences in RV function of SSc patients with and without LV diastolic dysfunction. Another reason why RV functions of SSc patients were closer to normal levels is an inadequate duration of time for the development of RV failure in SSc patients. In our study we demonstrated a negative correlation between RV function and disease duration. In patients with SSc, increased afterload is not the only reason for RV failure and SSc is a progressive disease characterized by fibrosis. The possible underlying mechanism of ventricular impairment could be myocardial fibrosis secondary to repeated ischemia-reperfusion abnormalities due to vascular lesions in SSc patients [3]. In a study comparison between SSc patients with PH and idiopathic pulmonary arterial hypertension (IPAH) it was shown that although RV afterload was similar in both disease groups, the prognosis of SSc with PH was worse than for IPAH patients [28]. This demonstrated that an intrinsic systolic dysfunction may be found in SSc patients.
Previous studies showed that LA strain and strain analysis by 2D STE correlated with Doppler parameters that display LA functions [29]. Although deterioration in LA strain values have been shown by STE in several cardiac diseases, such as paroxysmal atrial fibrillation [30], hypertrophic cardiomyopathy [31], and dilated cardiomyopathy [32], RA strain data are limited. In our study, we showed that RA reservoir and conduit parameters were significantly lower in SSc patients compared with controls. To the best of our knowledge, this is the first study to evaluate RA strain parameters in patients with SSc. Although we do not know the exact mechanism, a higher sPAP of SSc patients may be a reason.
Study limitations
Our first limitation is the small sample size. This may explain why the differences in some echocardiographic parameters were not significant. Although 2D STE is a novel echocardiographic technique known to be an angle-independent quantitative method for evaluating the myocardial function, there are some difficulties in evaluating RA functions. For example, RA myocardium is thinner than RV; therefore, the thinness of the atrium represents a possible technical limitation when evaluating the myocardial deformation by 2D STE. Despite the fact that our study had a cross-sectional design, we were not able to evaluate the prognostic value of the RA and RV functions in SSc patients without PH. Further prospective studies are needed to evaluate the prognostic value of determining right heart functions in patients with SSc. Moreover, it would be better to follow-up the patients and explore the relationship between adverse cardiac events and right heart functions in these patients.
Conclusion
Two-dimensional STE might be useful in detecting impairment in RV and RA functions in SSc patients with normal PAP. Future large-scale prospective studies are needed to clarify the right heart functions in SSc patients.
References
Medsger TA Jr (2001) Systemic sclerosis (scleroderma): clinical aspects. In: Koopman WJ (ed) Arthritis and allied conditions: a textbook of rheumatology, 14th edn. Lippincott Williams & Wilkins, Philadelphia, pp 1590–1624
Komócsi A, Vorobcsuk A, Faludi R et al (2012) The impact of cardiopulmonary manifestations on the mortality of SSc: a systematic review and meta-analysis of observational studies. Rheumatology (Oxford) 51:1027–1036
Kahan A, Allanore Y (2006) Primary myocardial involvement in systemic sclerosis. Rheumatology (Oxford) 45(Suppl 4):iv14–iv17
Rudski LG, Lai WW, Afilalo J et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713
Meris A, Faletra F, Conca C et al (2010) Timing and magnitude of regional right ventricular function: a speckle tracking-derived strain study of normal subjects and patients with right ventricular dysfunction. J Am Soc Echocardiogr 23:823–831
Masi AT, Rodnan GP, Medsger TA et al (1980) Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Preliminary criteria for the classification of systemic sclerosis (scleroderma). Arthritis Rheum 23:581–590
Cheitlin MD, Armstrong WF, Aurigemma GP et al (2003) ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). J Am Soc Echocardiogr 16:1091–1110
Sunbul M, Kepez A, Kivrak T et al (2013) Right ventricular longitudinal deformation parameters and exercise capacity. Herz. doi:10.1007/s00059-013-3842-y
Padeletti M, Cameli M, Lisi M et al (2012) Reference values of right atrial longitudinal strain imaging by two-dimensional speckle tracking. Echocardiography 29:147–152
Mor-Avi V, Lang RM, Badano LP et al (2011) Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. Eur J Echocardiogr 12:167–205
Muangchan C, Canadian Scleroderma Research Group, Baron M, Pope J (2013) The 15 % rule in scleroderma: the frequency of severe organ complications in systemic sclerosis. A systematic review. J Rheumatol 40:1545–1556
Gelber AC, Manno RL, Shah AA et al (2013) Race and association with disease manifestations and mortality in scleroderma: a 20-year experience at the Johns Hopkins Scleroderma Center and review of the literature. Medicine (Baltimore) 92:191–205
Hsiao SH, Lee CY, Chang SM et al (2006) Right heart function in scleroderma: insights from myocardial Doppler tissue imaging. J Am Soc Echocardiogr 19:507–514
Pavlicek M, Wahl A, Rutz T et al (2011) Right ventricular systolic function assessment: rank of echocardiographic methods vs. cardiac magnetic resonance imaging. Eur J Echocardiogr 12:871–880
Lee CY, Chang SM, Hsiao SH et al (2007) Right heart function and scleroderma: insights from tricuspid annular plane systolic excursion. Echocardiography 24:118–125
Hardegree EL, Sachdev A, Fenstad ER et al (2013) Impaired left ventricular mechanics in pulmonary arterial hypertension: identification of a cohort at high risk. Circ Heart Fail 6:748–755
Cusmà Piccione M, Zito C, Bagnato G et al (2013) Role of 2D strain in the early identification of left ventricular dysfunction and in the risk stratification of systemic sclerosis patients. Cardiovasc Ultrasound 11:6
Spethmann S, Dreger H, Schattke S et al (2012) Two-dimensional speckle tracking of the left ventricle in patients with systemic sclerosis for an early detection of myocardial involvement. Eur Heart J Cardiovasc Imaging 13:863–870
Sunbul M, Durmus E, Kıvrak T et al (2013) Left ventricular strain and strain rate by two-dimensional speckle tracking echocardiography in patients with subclinical hypothyroidism. Eur Rev Med Pharmacol Sci 17:3323–3328
Tanboğa IH, Işık T, Kaya A et al (2012) Two-dimensional strain imaging to predict the localization of an accessory pathway. Turk Kardiyol Dern Ars 40:108
Stefani L, Pedrizzetti G, De Luca A et al (2009) Real-time evaluation of longitudinal peak systolic strain (speckle tracking measurement) in left and right ventricles of athletes. Cardiovasc Ultrasound 7:17
Simsek Z, Tas MH, Gunay E et al (2013) Speckle-tracking echocardiographic imaging of the right ventricular systolic and diastolic parameters in chronic exercise. Int J Cardiovasc Imaging 29:1265–1271
Altekin RE, Karakas MS, Yanikoglu A et al (2012) Determination of right ventricular dysfunction using the speckle tracking echocardiography method in patients with obstructive sleep apnea. Cardiol J 19:130–139
Padeletti M, Cameli M, Lisi M et al (2011) Right atrial speckle tracking analysis as a novel noninvasive method for pulmonary hemodynamics assessment in patients with chronic systolic heart failure. Echocardiography 28:658–664
Matias C, Isla LP, Vasconcelos M et al (2009) Speckle-tracking-derived strain and strain-rate analysis: a technique for the evaluation of early alterations in right ventricle systolic function in patients with systemic sclerosis and normal pulmonary artery pressure. J Cardiovasc Med (Hagerstown) 10:129–134
Schattke S, Knebel F, Grohmann A et al (2010) Early right ventricular systolic dysfunction in patients with systemic sclerosis without pulmonary hypertension: a Doppler tissue and speckle tracking echocardiography study. Cardiovasc Ultrasound 8:3. doi:10.1186/1476-7120-8-3
Kepez A, Sunbul M, Kivrak T et al (2014) Evaluation of improvement in exercise capacity after pulmonary endarterectomy in patients with chronic thromboembolic pulmonary hypertension: correlation with echocardiographic parameters. Thorac Cardiovasc Surg 62:60–65
Tedford RJ, Mudd JO, Girgis RE et al (2013) Right ventricular dysfunction in systemic sclerosis associated pulmonary arterial hypertension. Circ Heart Fail 6:953–963
Saraiva RM, Demirkol S, Buakhamsri A et al (2010) Left atrial strain measured by two-dimensional speckle tracking represents a new tool to evaluate left atrial function. J Am Soc Echocardiogr 2:172–180
Tsai WC, Lee CH, Lin CC et al (2009) Association of left atrial strain and strain rate assessed by speckle tracking echocardiography with paroxysmal atrial fibrillation. Echocardiography 26:1188–1194
Rosça M, Popescu BA, Beladan CC et al (2010) Left atrial dysfunction as a correlate of heart failure symptoms in hypertrophic cardiomyopathy. J Am Soc Echocardiogr 23:1090–1098
D’Andrea A, Caso P, Romano S et al (2009) Association between left atrial myocardial function and exercise capacity in patients with either idiopathic or ischemic dilated cardiomyopathy: a two-dimensional speckle strain study. Int J Cardiol 132:354–363
Compliance with ethical guidelines
Conflict of interest. E. Durmus, M. Sunbul, K. Tigen, T. Kivrak, G. Ozen, I. Sari, H. Direskeneli, and Y. Basaran state that there are no conflicts of interest. All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Durmus, E., Sunbul, M., Tigen, K. et al. Right ventricular and atrial functions in systemic sclerosis patients without pulmonary hypertension. Herz 40, 709–715 (2015). https://doi.org/10.1007/s00059-014-4113-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-014-4113-2