Abstract
Introduction
To three-dimensionally analyze the skeletal and pharyngeal airway changes induced by Twin Block (TWB) and Forsus Fatigue Resistance Device (FFRD) in skeletal Class II female patients compared with untreated controls.
Materials and methods
The study comprised 62 growing female patients with skeletal Class II malocclusion due to mandibular retrusion treated with either TWB (n = 23) or FFRD (n = 21), or neither (n = 18; controls). Pre- and posttreatment/observational cone beam computed tomography images were used to evaluate the treatment changes.
Results
TWB induced more obvious mandibular skeletal changes and caused significant retrusive effects on the maxilla. Similarly, the sagittal and vertical jaw relationships were affected more obviously with TWB (P <0.001) compared to FFRD. Changes in oropharyngeal volume and minimal axial area were more obvious with TWB.
Discussion
The TWB functional appliance induced significant skeletal and pharyngeal airway changes. These changes were more obvious relative to the slight changes induced by FFRD or by natural growth.
Zusammenfassung
Einführung
Dreidimensional untersucht werden sollten TWB(Twin Block)- und FFRD(Forsus Fatigue Resistance Device)-induzierte Veränderungen der skelettalen und der pharyngealen Luftwege bei weiblichen Klasse-II-Patienten im Vergleich zu unbehandelten Kontrollen.
Material und Methoden
Die Studie umfasste 62 heranwachsende weibliche Patienten mit skelettaler Klasse-II-Malokklusion bei mandibulärer Retrusion, die entweder mit TWB (n = 23) oder FFRD (n = 21) behandelt wurden. Eine weitere, nicht behandelte Gruppe (n = 18) diente der Kontrolle. Zur Beurteilung der therapiebedingten Veränderungen wurden DVT(digitale Volumentomographie)-Aufnahmen vor und nach der Behandlung bzw. während der Beobachtungsphase analysiert.
Ergebnisse
Der TWB führte zu deutlicheren skelettalen Veränderungen der Mandibula und es kam zu signifikanten retrusiven Effekten auf die Maxilla. Auch die sagittalen und vertikalen Kieferrelationen wurden durch den TWB stärker verändert (<0,001) im Vergleich zum FFRD. Änderungen des oropharyngealen Volumens und der maximalen Engstelle des Atemweges waren bei TWB deutlicher zu erkennen.
Diskussion
Das TWB-Funktionsgerät führte zu signifikanten skelettalen Veränderungen und zu Veränderungen der pharyngealen Atemwege. Diese Veränderungen waren offensichtlicher im Vergleich zu den leichten Veränderungen, die durch die FFRD oder das natürliche Wachstum hervorgerufen wurden. .
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Class II malocclusion is one of the most common problems in orthodontic practice accounting for approximately one-third of the patients seeking orthodontic treatment [1]. Like other types of malocclusion, Class II malocclusion causes esthetic, functional, and psychological problems, the severity of which depends on the amount of anteroposterior discrepancy and its interaction with the surrounding soft tissue structures. Various factors contribute to the development of Class II malocclusion, but mandibular retrognathism is the most common factor [2]. This mandibular positioning pattern can be corrected during the growth period using functional appliances that can aid in enhancing and/or redirecting mandibular growth in a favorable direction [3].
In this context, the Twin Block (TWB) is the most popular functional appliance during the last few decades [4]. Recent systematic reviews concluded that TWB is the most efficient removable functional appliance in producing skeletal changes [5, 6]. In contrast, other systematic reviews reviewed the effects of fixed functional appliances (e.g. Forsus Fatigue Resistance Device [FFRD]) and concluded that though the appliances cause dentoalveolar changes, there is no or minimal skeletal effect [7, 8]. Interestingly, a recent systematic review evaluated the skeletal effects of removable and fixed functional appliances and concluded that there was little evidence concerning the comparative effectiveness of the two types of appliances [9].
Moss and Simon [10] developed the functional matrix theory which states that “most of the growth and development of the craniofacial region is under the control of functional activity of the surrounding soft tissues.” Hence, a direct relationship does exist between pharyngeal airway spaces and craniofacial configuration; any abnormality in these spaces might affect the position of the surrounding skeleton and vice versa. Indeed, it is argued that skeletal Class II malocclusion may play a role in the development of obstructive sleep apnea syndrome owing to the reduced oropharyngeal dimensions [11, 12].
Many studies have evaluated the effects of removable and fixed functional appliances on the pharyngeal airway spaces with conflicting results [13,14,15,16,17,18]. These studies relied upon two-dimensional evaluation using lateral cephalometry with its inherent limitations, such as distorted images, enlarged images in some areas and reduced in others, superimposition, and inaccurate landmark localization [19]. Two recently published systematic reviews [20, 21] retrieved and analyzed five studies that used cone beam computed tomography (CBCT) [22,23,24,25,26]. Of these, two studies used two-dimensional cephalometry extracted from CBCT images for measurements [23, 25], one had no control group [26], another one included samples with both males and females [22], and the last one [24] did not compare the effects of both types of appliances. Hence, no single study so far has compared both types of appliances with each other and with a control group using three-dimensional (3D) measurements of CBCT images.
Based on the above argument, the aim of this study was to evaluate the 3D treatment effects, in term of skeletal and pharyngeal airways changes, in skeletal Class II female patients treated by either TWB or FFRD in comparison with untreated controls.
Materials and methods
This was a controlled clinical study conducted at the outpatient clinics, Department of Orthodontics, Faculty of Oral and Dental Medicine, Cairo University, Egypt, and it was approved by the relevant Research Ethics Committee (1/13-8-2011), Faculty of Oral and Dental Medicine, Cairo University, Egypt. All parents were informed about the study procedure and written informed consents were obtained.
Patients were included if they fulfilled the following criteria: (1) growing females in stage 3–4 as assessed using the cervical vertebrae maturational indicators (CVMI) [27], (2) mandibular deficiency (convex profile with retruded mandible), (3) normal or protruded maxilla, (4) overjet: ≥5 mm, (5) buccal segment relationship: ≥½ unit Class II molar and canine relationship. All participants in the control group were treated using FFRD after completion of the observation period, upon achieving their turns in the waiting list.
The sample size was calculated with an alpha value of 0.05 and a power of 80% based on the study conducted by Rizk et al. [25], in which the mean treatment difference in airway volume was 5537.38 ± 4849.72 mm3 in the fixed functional appliance group and 2220.47 ± 1310.07 mm3 in the control group. The resultant sample size was 20 in each group. For the TWB group, the sample size was calculated based on the above criteria and the study by Elfeky et al. [24], in which the mean treatment difference in oropharyngeal airway space was 3052.45 ± 1281.2 mm3 in the TWB group and 738.17 ± 507.11 mm3 in the control group. The resultant sample size was 5 in each group. Accordingly, it was decided that 20 participants would be included in each of the groups accounting for a total sample size of 60 participants. This number was increased to 74 participants to compensate for any potential dropouts. Of the 52 patients allocated to the treatment groups, 31 were treated with TWB and 21 with FFRD, while 22 patients were observed as untreated controls (Fig. 1).
CBCT images were obtained using the i‑Cat CBCT machine (Imaging Sciences International, Hatfield, PA, USA). The source to detector distance was 67.5 cm. The voxel dimension selected was 0.3 mm and slice thickness was 2.00 mm. The image detector was a flat panel measuring 20 × 25 cm; images were acquired at 14 bits in a single 360° rotation [28]. These images were used for pretreatment/observational measurements (T1).
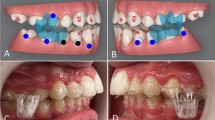
Participants in the TWB group were treated using a standard TWB appliance according to the procedure described by Clark ([4]; Fig. 2). The patients were instructed to wear the appliance continuously (24 h/day), including at mealtimes, and were followed up once every 4 weeks. The anteroposterior dental arch relationship was assessed, with and without the appliance, at each appointment. The active treatment period was complete when there was no difference, with and without the appliance, and the mandible could not be retruded. Retention period with the appliance continued for another 3 months.
Participants in the FFRD group were treated with fixed appliances as follows: MBT prescription brackets (3M Unitek, St. Paul, MN, USA) with 0.022 inch slot were bonded to the upper and lower teeth. A soldered passive transpalatal arch (TPA) was fitted to the maxillary first molars. Alignment and leveling proceeded until 0.019 × 0.025 inch stainless-steel arch wires were engaged. The FFRD was fitted according to the manufacturer’s instructions (3M Unitek). Follow-up visits were scheduled every 4 weeks for assessing the changes, provisioning maintenance, and activation (Fig. 3). The active phase continued until Class II occlusion was overcorrected to an edge-to-edge incisal relationship. Thereafter, the fixed appliance was retained to finalize the occlusion. Upon completion of the treatment period, the second CBCT image was obtained for each participant and used for posttreatment/observational measurements (T2).
Three-dimensional skeletal measurements were performed using Anatomage 5.02 software (Anatomage, San Jose, CA, USA), while 3D pharyngeal airway measurements were obtained using Dolphin 11.5 software (Dolphin Imaging and Management Solutions, Chatsworth, CA, USA) with a saturation level of 72 [24, 29, 30]. Descriptions of these measurements are listed in Table 1.
The three-dimensional (3D) upper pharyngeal airway measurements included: (1) nasopharyngeal airway volume (Fig. 4), (2) oropharyngeal airway volume (Fig. 5), and (3) minimal axial area (Fig. 6).
Fourteen pre- and posttreatment/observation CBCT images were selected randomly and measured independently by two examiners on two occasions with a 2-week interval to assure reliability of the measurements.
Statistical analysis
Data were input and analysed using the statistical package for social sciences (SPSS) software, Version 21 (IBM Corp., Armonk, NY, USA) for windows. Intraclass correlation coefficients (ICCs) were calculated to assess the reliability and reproducibility of the measurements. Descriptive statistics, including mean and standard deviation for each variable, were calculated and presented. Data were checked for normal distribution using Kolmogorov–Smirnov test. Comparison of pre- and posttreatment/observational measurements was accomplished using the paired t‑test (or Wilcoxon signed-rank test). Between the groups, both pre- and posttreatment/observational comparisons were conducted using one way analysis of variance (ANOVA) (or Kruskal–Wallis test) followed by Bonferroni correction (or Mann–Whitney U test) whenever one way ANOVA (or Kruskal–Wallis test) revealed a statistical significance. A P value of <0.05 was considered statistically significant.
Results
Out of the 74 patients included in this study, 62 patients completed the treatment (23 TWB patients, 21 FFRD patients, and 18 controls). Most of the patients who dropped out were in the TWB group (Fig. 1).
Intraclass correlation coefficients with regard to intra- and interexaminer measurements ranged from 0.789 and 0.984 for nasopharyngeal volume and ANB, respectively, to 0.788 and 0.995 for oropharyngeal volume and B‑NV, respectively, indicating a high degree of reliability.
With regard to T1 measurements, there were statistically significant differences between the TWB and FFRD groups in many mandibular skeletal linear measurements, sagittal jaw relationships, and mandibular plane inclinations. The mandibular plane inclination and naso-pharyngeal airway volume were significantly different between the control group and the FFRD and TWB groups (Table 2).
Differences between T1 and T2 were more obvious in the TWB group. These differences were in terms of mandibular skeletal measurements, sagittal and vertical jaw relationships, and pharyngeal airway spaces. Although to a very small extent, the second obvious difference was seen in the control group, more specifically in the vertical skeletal jaw relationship. There was no difference between the T1 and T2 measurements in the FFRD group (Table 3).
The changes induced by treatment/growth are presented in Table 4. No differences were recorded in all the maxillary skeletal measurements, neither between the TWB and FFRD groups nor between the FFRD group and control group. Only change of the maxillary base position (SNA) was significantly higher in the TWB group than the control group. For all other measurements, the TWB group demonstrated more significant posttreatment changes compared to the FFRD and control groups. Changes in the FFRD and control groups were not significantly different.
Table 5 presents the correlations between the changes of measurements in skeletal and pharyngeal airways. There were significant direct correlations between the oropharyngeal airway and SNA, and Po-NV and SNB (r = 0.481, 0.490 and 0.712, respectively) in the TWB group. There was also an inverse correlation between the minimal axial area and ANB in that group (r = −0.422). The minimal axial area in the control group showed a significant inverse correlation with SNA (r = −0.612) and a significant direct correlation with Pg-NV (r = −0.602). No single correlation was found in the FFRD group.
Discussion
In this study, use of TWB revealed the most obvious skeletal treatment effects in terms of maxillary, mandibular, sagittal, vertical, and pharyngeal airway 3D measurements compared to natural growth in controls and even to the skeletal treatment effects induced by FFRD. The latter is known to induce camouflage dentoalveolar effects and since those measurements were not included in this study, its real effects were not evident. In other words, the current study revealed no obvious skeletal effects with FFRD, when the changes induced by this appliance were compared with the natural growth effects in controls.
All the subjects who participated in the study were females. This was to rule out the gender effect, as mandibular growth is sex- and age-dependent [31].
The results of randomized and controlled clinical trials (RCT, CCT) [32,33,34,35,36] were analysed in a recent systematic review [9] that compared the efficacy of fixed versus removable functional appliances in children with Class II malocclusion. Of the reviewed studies, one reported soft tissue changes [33], two compared the TWB and the Herbst appliances [32, 35], and two compared the activator with FFRD [34] and Twin Force appliances [36]. Although these studies used two-dimensional imaging techniques, the review indicated that these studies currently represent the highest available level of evidence [9].
It is well recognized that orthopaedic/orthodontic therapy using functional appliances has maximum effects when performed during the mandibular growth spurt period. The greatest skeletal effects have been found in patients treated within the peak pubertal growth period [27]. Hence, in this study, participants in the TWB and control groups were selected in pubertal growth stage 3, based on CVMI [27], as it is the optimum treatment period to achieve maximum skeletal effects, either through natural growth or induction by therapeutic functional intervention. In the FFRD group, however, participants were selected in the later stage of growth so as to minimize the time before installation of the fixed functional appliance.
With regard to skeletal changes in the maxilla, neither appliance induced noticeable effects. When their effects were compared separately with the growth effect in the controls, TWB showed a significantly greater net retrusive effect than FFRD. The effective maxillary length was not affected by normal growth or any of the functional appliances. Accordingly, it can be concluded that TWB is effective in inhibiting forward growth of the maxilla. This finding is similar to that in the study by Bilgic et al. [34]. A recent systematic review concluded that “removable functional appliances in Class II growing patients have a slight inhibitory effect on the sagittal growth of the maxilla in the short term” [37]. In contrast to this study’s results, Dalci et al. [36] found an insignificant effect of TWB on the maxillary base. Otherwise, effective maxillary length was not affected in all the groups in this study; this implies that neither these appliances nor normal growth has an effect on the anterioposterior maxillary position (point A) or vertical growth of the condyle (Co).
Besides the restricting effects on the maxilla, TWB revealed growth-enhancing effects on the mandible compared with both FFRD and controls. Otherwise, the skeletal effects of FFRD on the mandible were not different compared to the natural growth increments reported in controls. These findings were similar to those reported by Bilgic et al. [34], Dacli et al. [36] and many recent systematic reviews [5, 7, 9]. This can be attributed to the mechanism of action of the TWB which relies on skeletal and dentoalveolar anchorage unlike the FFRD which relies only on dentoalveolar anchorage.
These minor restricting changes of the maxilla and major growth enhancing changes of the mandible were probably responsible for the evident reduction of sagittal jaw discrepancy, more specifically in the TWB group. Such sagittal changes have been reported in many CCTs [34, 36]. It is worth noting that both appliances successfully corrected the Class II molar relationship, overjet, and overbite malocclusion with varying degrees of skeletal changes. This correction can be attributed to the inhibiting effect on the maxilla and the growth-stimulating effect on the mandible in the TWB group, and to maxillary incisor retrusion and mandibular incisor protrusion in the FFRD group.
With regard to the vertical jaw relationship, inclination of the mandibular plane was not affected significantly in all groups unlike the posterior to anterior facial height, which was significantly increased in the TWB group compared to both the FFRD and control groups. Similar findings were reported by Bilgic et al. [34] and Dacli et al. [36]. Although the increase in the posterior to anterior facial height was statistically significant in the TWB group, it seems to be insignificant from a clinical point of view.
So far, to the best of available knowledge, no single study has compared the effect of removable versus fixed functional appliances on oropharyngeal airways. Furthermore, the studies that evaluated oropharyngeal airways in Class II patients using a single functional appliance did so based on two-dimensional images of CBCT scans [23, 25], included participants of both sexes [22], or did not consider the effect of natural growth [26] (no controls included).
The findings in this study indicated a significant increase in the nasopharyngeal airway in the TWB group compared to both the FFRD and control groups. These changes might be attributed to the maxillary skeletal changes produced by TWB relative to FFRD and natural growth amongst controls. This contradicts the results of Li et al. [22] who did not report a significant change in the nasopharyngeal volume; however, it is also similar to the conclusions of many systematic reviews and meta-analyses [20, 21].
The major changes were observed in the oropharyngeal airway in the TWB group compared to both FFRD and control groups. The anteroposterior positional changes of the mandible, and possibly, a forward movement of the hyoid bone owing to the direct connection between them, may be responsible for such a volumetric increase of the oropharyngeal airway. This finding is in line with that reported by Li et al. [22] and other systematic reviews [20, 21]. In the current study, FFRD had no skeletal effect on the mandible, and subsequently, on the oropharyngeal volume. Such a result contradicts the findings of Temani et al. [26] who evaluated the effect of FFRD on the oropharyngeal airway; however, natural growth changes were not considered in that study (no control group).
In the TWB group, the more obvious the changes exerted on the mandible and sagittal jaw relationship, the more obvious were the changes in oropharyngeal airway volume. This correlation was mostly due to the increased distance between the posterior limits of the maxillary and mandibular bases and the posterior pharyngeal wall. Erbas and Kocadereli [23] concluded that anterior repositioning of the mandible with the Xbow appliance resulted in an increased oropharyngeal airway volume. This correlation was not found in the FFRD group owing to the lack of skeletal effects, as the effects of FFRD are purely dentoalveolar [7].
Generally, the changes in the naso- and oro-pharyngeal airways and in the minimal axial areas were observed after short term evaluation. The long-term effects (after 2–3 years following treatment) need to be addressed. Moreover, growth has its own effects on these airway measurements, irrespective of being positive or negative. Once those two factors are considered, a more obvious conclusion can be drawn.
Conclusions
The Twin Block functional appliance induced significant skeletal and pharyngeal airway changes compared to the effects induced by FFRD or by natural growth.
References
Proffit WR, Fields HW Jr., Moray LJ (1998) Prevalence of malocclusion and orthodontic treatment need in the United States: Estimates from the NHANES III survey. Int J Adult Orthodon Orthognath Surg 13(2):97–106
McNamara JA Jr. (1981) Components of class II malocclusion in children 8–10 years of age. Angle Orthod 51(3):177–202
Barnett GA, Higgins DW, Major PW, Flores-Mir C (2008) Immediate skeletal and dentoalveolar effects of the crown- or banded type Herbst appliance on Class II division 1 malocclusion. Angle Orthod 78(2):361–369
Clark W (2014) Twin block functional therapy
Ehsani S, Nebbe B, Normando D, Lagravere MO, Flores-Mir C (2015) Short-term treatment effects produced by the Twin-block appliance: A systematic review and meta-analysis. Eur J Orthod 37(2):170–176
Perinetti G, Primožič J, Franchi L, Contardo L (2015) Treatment effects of removable functional appliances in pre-pubertal and pubertal class II patients: A systematic review and meta-analysis of controlled studies. PLoS ONE 10(10):e141198
Ishaq RA, AlHammadi MS, Fayed MM, El-Ezz AA, Mostafa Y (2016) Fixed functional appliances with multibracket appliances have no skeletal effect on the mandible: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 149(5):612–624
Zymperdikas VF, Koretsi V, Papageorgiou SN, Papadopoulos MA (2016) Treatment effects of fixed functional appliances in patients with Class II malocclusion: A systematic review and meta-analysis. Eur J Orthod 38(2):113–126
Pacha MM, Fleming PS, Johal A (2015) A comparison of the efficacy of fixed versus removable functional appliances in children with Class II malocclusion: A systematic review. Eur J Orthod 38(6):621–630
Moss ML, Simon MR (1968) Growth of the human mandibular angular process: A functional cranial analysis. Am J Phys Anthropol 28(2):127–138
El H, Palomo JM (2011) Airway volume for different dentofacial skeletal patterns. Am J Orthod Dentofacial Orthop 139(6):e511–e521
Katyal V, Pamula Y, Martin AJ, Daynes CN, Kennedy JD, Sampson WJ (2013) Craniofacial and upper airway morphology in pediatric sleep-disordered breathing: Systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 143(1):20–30.e23
Ghodke S, Utreja AK, Singh SP, Jena AK (2014) Effects of twin-block appliance on the anatomy of pharyngeal airway passage (PAP) in class II malocclusion subjects. Prog Orthod 15:68
Jena AK, Singh SP, Utreja AK (2013) Effectiveness of twin-block and Mandibular Protraction Appliance-IV in the improvement of pharyngeal airway passage dimensions in Class II malocclusion subjects with a retrognathic mandible. Angle Orthod 83(4):728–734
Vinoth SK, Thomas AV, Nethravathy R (2013) Cephalomteric changes in airway dimensions with twin block therapy in growing Class II patients. J Pharm Bioallied Sci 5(Suppl 1):S25–S29
Verma G, Tandon P, Nagar A, Singh GP, Singh A (2012) Cephalometric evaluation of hyoid bone position and pharyngeal spaces following treatment with Twin block appliance. J Orthod Sci 1(3):77–82
Ozdemir F, Ulkur F, Nalbantgil D (2014) Effects of fixed functional therapy on tongue and hyoid positions and posterior airway. Angle Orthod 84(2):260–264
Bavbek NC, Tuncer BB, Turkoz C, Ulusoy C, Tuncer C (2016) Changes in airway dimensions and hyoid bone position following class II correction with forsus fatigue resistant device. Clin Oral Investig 20(7):1747–1755
Gribel BF, Gribel MN, Frazão DC, McNamara JA Jr, Manzi FR (2011) Accuracy and reliability of craniometric measurements on lateral cephalometry and 3D measurements on CBCT scans. Angle Orthod 81(1):26–35
Kannan A, Sathyanarayana HP, Padmanabhan S (2017) Effect of functional appliances on the airway dimensions in patients with skeletal class II malocclusion: A systematic review. J Orthod Sci 6(2):54–64
Xiang M, Hu B, Liu Y, Sun J, Song J (2017) Changes in airway dimensions following functional appliances in growing patients with skeletal class II malocclusion: A systematic review and meta-analysis. Int J Pediatr Otorhinolaryngol 97:170–180
Li L, Liu H, Cheng H et al (2014) CBCT evaluation of the upper airway morphological changes in growing patients of class II division 1 malocclusion with mandibular retrusion using twin block appliance: A comparative research. PLoS ONE 9(4):e94378
Erbas B, Kocadereli I (2014) Upper airway changes after Xbow appliance therapy evaluated with cone beam computed tomography. Angle Orthod 84(4):693–700
Elfeky HY, Fayed MM (2015) Three-dimensional effects of twin block therapy on pharyngeal airway parameters in Class II malocclusion patients. J World Fed Orthod 4(3):114–119
Rizk S, Kulbersh VP, Al-Qawasmi R (2016) Changes in the oropharyngeal airway of Class II patients treated with the mandibular anterior repositioning appliance. Angle Orthod 86(6):955–961
Temani P, Jain P, Rathee P, Temani R (2016) Volumetric changes in pharyngeal airway in Class II division 1 patients treated with Forsus-fixed functional appliance: A three-dimensional cone-beam computed tomography study. Contemp Clin Dent 7(1):31–35
Baccetti T, Franchi L, Toth LR, McNamara JA Jr (2000) Treatment timing for Twin-block therapy. Am J Orthod Dentofacial Orthop 118(2):159–170
De Vos W, Casselman J, Swennen GR (2009) Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: A systematic review of the literature. Int J Oral Maxillofac Surg 38(6):609–625
Alves M, Baratieri C, Mattos CT et al (2012) Is the airway volume being correctly analyzed? Am J Orthod Dentofacial Orthop 141(5):657–661
Zimmerman JN, Lee J, Pliska BT (2017) Reliability of upper pharyngeal airway assessment using dental CBCT. Eur J Orthod 39(5):489–496. https://doi.org/10.1093/ejo/cjw07
Ruf S, Baltromejus S, Pancherz H (2001) Effective condylar growth and chin position changes in activator treatment: a cephalometric roentgenographic study. Angle Orthod 71(1):4–11
O’Brien K, Wright J, Conboy F et al (2003) Effectiveness of treatment for Class II malocclusion with the Herbst or twin-block appliances: A randomized, controlled trial. Am J Orthod Dentofacial Orthop 124(2):128–137
Baysal A, Uysal T (2011) Soft tissue effects of Twin block and Herbst appliances in patients with Class II division 1 mandibular retrognathy. Eur J Orthod 35(1):71–81
Bilgic F, Hamamci O, Basaran G (2011) Comparison of the effects of fixed and removable functional appliances on the skeletal and dentoalveolar structures. Aust Orthod J 27(2):110–116
Baysal A, Uysal T (2013) Dentoskeletal effects of Twin block and Herbst appliances in patients with Class II division 1 mandibular retrognathy. Eur J Orthod 36(2):164–172
Dalci O, Altug AT, Memikoglu UT (2014) Treatment effects of a twin-force bite corrector versus an activator in comparison with an untreated Class II sample: A preliminary report. Aust Orthod J 30(1):45–53
Nucera R, Lo Giudice A, Rustico L, Matarese G, Papadopoulos MA, Cordasco G (2016) Effectiveness of orthodontic treatment with functional appliances on maxillary growth in the short term: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop 149(5):600–611.e603
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.S. Alhammadi, H.Y. Elfeky, M.S. Fayed, R.A.R. Ishaq, E. Halboub and A.A. Al-mashraqi declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Alhammadi, M.S., Elfeky, H.Y., Fayed, M.S. et al. Three-dimensional skeletal and pharyngeal airway changes following therapy with functional appliances in growing skeletal Class II malocclusion patients. J Orofac Orthop 80, 254–265 (2019). https://doi.org/10.1007/s00056-019-00185-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-019-00185-7
Keywords
- Twin Block
- Pharyngeal airway
- Cone-beam computed tomography
- Functional appliance
- Mandibular skeletal changes