Abstract
Objective
The objective of this study was to investigate the effects of fixed functional therapy on oropharyngeal airway dimensions and hyoid bone positions in Class II patients and make comparison with an untreated Class II group.
Materials and methods
Eighteen patients (8 girls, 10 boys; mean age 13.62 ± 1.92 years) who were treated with Forsus Fatique Resistant Device (FFRD) and 19 patients (11 girls, 8 boys; mean age 12.74 ± 0.91 years) who served as control were enrolled. Cephalograms were used to assess linear, angular, and area measurements. Intragroup comparisons were made by paired t and Wilcoxon tests and intergroup comparisons were performed by independent t test.
Results
With respect to controls, FFRD group showed increased airway dimensions at soft palate (P < 0.05) and more forward positioning of the hyoid bone (P < 0.05). Dentoalveolar changes exhibited mesial movement of lower incisors and molars and reduction in overjet (P < 0.001) in FFRD group.
Conclusions
Positive effects in oropharyngeal airway dimensions and increased values of hyoid bone displacement to a more forward position were found after fixed functional therapy.
Clinical Relevance
Treatment with fixed functional appliances is mostly based on mesial movement of mandibular dentition, which might influence changes in tongue posture. The present results might indicate that oropharyngeal airway dimensions may be affected by postural changes of the hyoid bone in consequence of dentoalveolar changes. Clinically, these may be considered especially in Class II cases with reduced airway dimensions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orthodontic malocclusions may have adverse effects on oral functions, esthetics, speech, and/or social behaviors of patients. In particular, Class II malocclusions, characterized by mandibular deficiency [1], may be one of the possible causes of upper airway disorders and oropharyngeal airway deficiencies [2, 3]. There is a variety of Class II treatment modalities, such as extraoral appliances, functional appliances, fixed appliances, or surgical treatments depending on the underlying cause and age at the beginning of treatment [4, 5]. Functional appliances have been the main treatment choices in mandibular deficiency cases during growth period, which are believed to stimulate growth by forward positioning of the mandible. As well as improving the skeletal pattern, they cause an increase in oropharyngeal dimensions by forcing the mandible, hyoid bone, tongue, and soft palate forward [6, 7]. In that respect, it has been stated that early orthodontic treatment of mandibular deficiencies by functional appliances would be beneficial to prevent airway problems [8, 9]. However, the need for patient cooperation limits the use of these removable devices [5, 10]. Compliance issues led the clinicians to develop intraoral techniques such as fixed functional appliances (FFA) which offer reliable mechanics that need no cooperation [5]. Studies reported that correction of Class II relationship with FFA is mainly due to dentoalveolar improvements with limited skeletal effects depending on the appliance, age, and remaining growth potential of the patient [11, 12].
The Forsus Fatique Resistant Device (FFRD) (3M Unitek, Monrovia, CA, USA) is a commonly used FFA in orthodontic practice. It is a semirigid telescoping system, which is designed to resist against breakage and claimed to produce continuous forces [13]. The device consists of two parts: a stainless steel coil spring and a rod, whose size is chosen according to the distance from the distal side of the buccal tube of the upper first molar band to the distal side of the lower canine bracket. Similar to other FFA, reports revealed that FFRD was mainly effective at the dentoalveolar correction of Class II malocclusions [4, 12, 14, 15], but some findings addressed skeletal effects as well [5, 16, 17]. Although treatment effects of FFA have been discussed briefly, evaluations concerning the airway dimensions are still lacking. From previous studies, it appears that dentoalveolar changes may alter airway dimensions [18, 19]; therefore, changes in airway dimensions can also be expected with FFA. However, only few studies have addressed the effects of FFA on the depth of pharyngeal airway [19–21].
Therefore, the aim of this study was to evaluate the effects of a commonly used FFA (FFRD) on pharyngeal airway dimensions and hyoid bone positions in Class II patients using cephalometric radiographs and compare it with that of an untreated Class II control group.
Materials and methods
The study material for this retrospective study were selected from the archives of the Department of Orthodontics, Gazi University, and consisted of pre- and post-treatment radiographs of patients treated with FFRD. Sample size was calculated with a statistical power of 0.80, and the number of patients per group was required to be minimum 17. Ethical approval was obtained from the Ethical Committee Board of Gazi University (77082166-604.01.02-12555). Written informed consents of all patients were present in their files as a regular procedure.
Sample collection
The first computer search of patient files between 2008 and 2014 revealed that 94 patients were treated with FFRD in our clinic. From those records, only the ones that fulfilled the following inclusion criteria were considered for evaluation:
-
1.
Skeletal (ANB > 4°) and dental Class II malocclusion with mandibular retrusion (SNB < 80°) and increased overjet (>5 mm)
-
2.
Optimal mandibular plane angle (SN/GoGn 32 ± 6°)
-
3.
Patients who were after the pubertal growth spurt or during the late stages of puberty
-
4.
No functional shift or dual bite
-
5.
No congenital anomalies causing changes in airway dimensions
-
6.
No medical history about a respiratory problem or an upper airway surgery
-
7.
Presence of good quality lateral cephalograms and hand and wrist radiographs at the beginning (after alignment) and at the end of FFRD phase (after Class I molar and canine relationships were achieved)
Clinical considerations
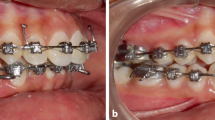
To be able to establish a comparable set of data, treatment records of each patient were re-examined to identify the FFRD procedures and only the ones who were treated with the same procedure were analyzed: fixed orthodontic treatment with Roth metal brackets (0.018″ slot size prescription); rods of FFRD placed from buccal tubes of the upper first molar bands to the arch wire between lower canines and first premolars (Fig. 1); no modifications during FFRD appliance (mini-implants, rapid maxillary expansion, lingual fixed appliances, extra root torque to lower incisors); FFRD was applied after alignment of teeth; and 0.017 × 0.025 in. stainless steel wires were inserted passively to both arches and cinched distal to the lower molars. Force is generated via the compression of the coil spring, and the force acts on both dental arches in opposite directions (distal force in maxilla and mesial force in the mandible) (Fig.1b).
The final study group (FFRD group) consisted of 18 patients (8 girls, 10 boys, mean age 13.62 ± 1.92 years) with a mean treatment time of 8.74 ± 3.46 months. The treatment was completed successfully in all cases when Angle Class I relationship was achieved. An untreated control group was formed to distinguish changes due to FFRD and growth. Groups were matched according to their chronological ages and sagittal (ANB°) and vertical (SN/GoGn°) skeletal patterns (Table 1). The control group consisted of 19 patients (11 girls, 8 boys, mean age 12.74 ± 0.91 years), who were observed for adequate oral hygiene before starting fixed orthodontic treatment, after a mean observation period of 11.89 ± 1.37 months.
Cephalometric evaluation
All cephalometric radiographs were taken with the same instrument under standard conditions (Trophy Instrumentarium Cephalometer, OP 100, Instrumentarium Imaging Co., Tuusula, Finland) at 70 kVp, 16 mA/s, in centric occlusion according to the natural head position (NHP) and after a usual swallow, by a single technician. The distance from the focus of the device to the mid-sagittal plane of the patient was 150 cm, and the distance from the film to the mid-sagittal plane of the patient was 20 cm. All linear measurements were corrected for the 10 % magnification. Cephalograms were manually traced and evaluated by the same researcher at the beginning and end of FFRD application/observation periods. Linear and angular measurements performed on the tracings were given in Fig. 2. Upper and lower dental measurements were performed in relation to the reference planes Ptm-Ver (perpendicular to palatal line from the posterior border of pterygomaxillary fissure) and T┴GoMe (perpendicular to GoMe from the intersection point of the anterior wall of sella turcica and tuberculum sella), respectively (Fig. 3a, b).
Cephalometric points and planes. 1 SNA; 2 SNB; 3 ANB; 4 SN-PP (the angle between SN plane and palatal plane constructed from ANS to PNS); 5 SN-GoGn; 6 SN-OP (the angle between SN plane and occlusal plane); 7 S-ANS; 8 S-PNS; 9 N-ANS; 10 N-PNS; 11 S-Go; 12 N-Me; 13 PP projection (the distance between PNS and the posterior pharynx wall through palatal plane; 14 SPS (the distance of the midpoint of the line from PNS to tip of soft palate to the horizontal counterpart on the posterior pharyngeal wall along the parallel line to Frankfurt horizontal plane); 15 MPS (the distance of the tip of the soft palate to the horizontal counterpart on the posterior pharyngeal wall along the parallel line to Frankfurt horizontal plane); 16 Cv2 projection (the distance of the intersection points on anterior and posterior pharyngeal wall through Cv2ai along the parallel line to Frankfurt horizontal plane); 17 Cv3 projection (the distance of the intersection points on anterior and posterior pharyngeal wall through Cv3ai along the parallel line to Frankfurt horizontal plane); 18 H-MP (the perpendicular distance from hyoid bone to mandibular plane); 19 H-SN (the perpendicular distance from hyoid bone to SN plane); 20 C3-H (the distance from the anterior-inferior point of the third cervical vertebra to point H)
Dental measurements. a PtmVer (reference plane for upper jaw): perpendicular line to palatal plane (ANS-PNS) from the posterior border of pterygomaxillary fissure; (1) U1-PtmVer (the perpendicular distance of the tip of the upper incisor to PtmVer); (2) U6-PtmVer (the perpendicular distance of the mesio-buccal tubercule of the upper first molar to PtmVer); b T┴GoMe (reference plane for lower jaw): Perpendicular line to mandibular plane (GoMe) from the intersection point of anterior wall of sella turcica and tuberculum sella; (3) L1-T┴GoMe (the perpendicular distance of the tip of the lower incisor to T┴GoMe); (4) L6-T┴GoMe (the perpendicular distance of the mesio-buccal tubercule of the lower first molar to T┴GoMe)
The area measurements were performed by an engineering drawing software that is used for topographic studies (NETCAD for Windows, 5.1.0.962 Software; Ulusal Co., Ankara, Turkey). The palatal line through ANS-PNS and the base of epiglottis were accepted as the upper and lower borders of the oropharyngeal airway (OA) on cephalometric tracings, and they were all scanned (EPSON Perfection, V700 Photo, Japan) at standard conditions. OA was digitized according to the specified points by two different researchers to obtain maximum reliability and agreement (Fig. 4). The software calculated the numerical values of areas, and derived numbers were designated as units.
To evaluate the error in tracings and examiner reliability, randomly selected 15 radiographs among all groups were re-traced and re-measured 15 days after the first evaluation. Intraclass correlation coefficients (ICCs) were calculated to determine the intraexaminer and interexaminer reliability of each landmark. Overall, the ICC values indicated good reliability for the measurements assessed. The ICC values were greater than 0.94 for 95 % of intraexaminer and 88 % of interexaminer assessments.
Statistical analysis
All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) Version 20.0 (SPSS Inc., Chicago, IL, USA). Normal Gaussian distribution was applied through the Shapiro-Wilk goodness-of-fit test to evaluate the normality of data distribution. Homogeneity of variances was checked using Levene’s test, and Welch-Satterthwaite adjustment was considered in case Test of Equality of Variances failed. For parametric distributions, Paired sample t test was used to compare differences in the mean values of variables between pre- and post-treatment/observation groups. Independent samples t test was used to compare differences in the mean values of variables between FFRD and control groups. For non-parametric distributions, the Wilcoxon signed-rank test was used to compare differences in the mean values of variables between pre- and post-treatment/observation groups and Mann-Whitney U test was used to compare differences in the mean values of variables between FFRD and control groups. Bonferroni correction was made for all comparisons. Bivariate correlation coefficients (r) were calculated using the Pearson product moment formula or Spearman’s rank test, dependent on normality of distribution or not. A P value of <0.05 was considered statistically significant.
Results
No significant pre-treatment and observation differences were found between two groups for the variables used for matching (ANB, SN-GoGn angles, and age) (Table 1).
The pre- and post-treatment and pre- and post-observation cephalometric descriptive values and comparison of the changes within each group are presented in Table 2.
Changes in FFRD group (T2-T1)
Vertical skeletal changes indicated an increase in SN-OP angle by 1.11° (P < 0.001). Maxilla (S-ANS, P < 0.01; S-PNS, P < 0.05; N-ANS, P < 0.001; N-PNS, P < 0.05) and the mandible (S-Go, P < 0.01; N-Me, P < 0.001) moved downward significantly. The dentoalveolar changes showed that upper first molars moved slightly distally by 0.31 mm (P < 0.05) while lower incisors were protruded by 2.81 mm (P < 0.001) and lower first molars moved mesially by 1.33 mm (P < 0.001). Overjet was significantly decreased from 6.61 to 3.11 mm (P < 0.001).
Evaluation related to airway morphology showed significant increases at all levels (PP projection, SPS, MPS, Cv2 projection, P < 0.05, respectively; Cv3 projection, area, P < 0.01, respectively). Hyoid bone moved forward by 1.68 mm (C3-H, P < 0.05).
Changes in control group (O2-O1)
Vertically, maxilla and the mandible moved downward (P < 0.001). At the end of observation, upper incisors moved labially (P < 0.01).
Airway dimensions remained unchanged, except for the pharyngeal size at palatal plane level, which was increased by 1.33 mm (PP projection, P < 0.05). Hyoid bone moved downward by 1.53 mm in relation to the mandibular plane and 2.05 mm in relation to SN plane (H-MP, H-SN, P < 0.05, P < 0.001, respectively) and moved forward by 0.84 mm (C3-H, P < 0.05).
Comparison of the changes between groups
In Table 3, comparisons of mean differences between groups are presented. Increases in vertical maxillary and mandibular measurements were more prominent in the control group when compared with those in FFRD group (S-ANS, N-PNS, P < 0.01; S-PNS, P < 0.05; S-Go, P < 0.01; N-Me, P < 0.001). The FFRD group displayed 2.81 mm mesial movement of lower incisors, while control group displayed only 0.44 mm mesialization, declaring a significant difference at 0.001 level between groups. There was also more mesial movement of lower first molars in FFRD group by 1.33 mm, relative to controls (P < 0.001). Reduction in overjet by 3.5 mm was prominent in FFRD group, when compared with that in the control group (P < 0.001).
Pharyngeal airway measurements showed group differences at several levels. SPS increased 1.06 mm and MPS increased 1.28 mm, while there were reductions in the control group at these levels (P < 0.05, respectively). Increase in the vertical movement of the hyoid bone was significantly higher in the control group by 2.05 mm in relation to FFRD group (H-SN, P < 0.001). However, forward movement of the hyoid bone was more prominent in FFRD group (1.68 mm) than in the control group (0.84 mm) (C3-H, P < 0.05).
Correlations in FFRD group
Sagittal positions of lower incisors were positively correlated with MPS (r = 0.590, P < 0.05). Pharyngeal airway dimension at Cv2 cervical vertebral level was negatively correlated with the vertical position of the hyoid bone (H-MP; r = −0.501, P < 0.05) and positively correlated with the sagittal position of the hyoid bone (C3-H; r = 0.556, P < 0.05).
Correlations in control group
Pharyngeal airway dimensions at Cv2 and Cv3 cervical vertebral levels were negatively correlated with the vertical position of the hyoid bone (H-MP; r = −0.492, P < 0.05; H-SN; r = −0.604, P < 0.01).
Discussion
Literature knowledge revealed that treatment of skeletal Class II malocclusions with functional orthopedic appliances offers positive effects on pharyngeal airway passage [22]. Fixed functional appliances have provided an alternative choice of Class II treatment, especially for non-compliant patients; however, there is limited knowledge about their effects on airway dimensions. For this reason, the aim of this study was to evaluate the effects of one of these devices (FFRD) on pharyngeal airway dimensions and hyoid bone positions in comparison with those in an untreated Class II group. In order to evaluate the real effects of the appliance, the second phase of orthodontic treatment (finishing fixed orthodontic treatment) was not included. Patients who were after the pubertal growth spurt or at the late stages of puberty were included, because while conventional functional appliances can be used during active growth spurt, it is suitable to use FFA after the pubertal growth spurt. Lateral cephalograms were used since they provide attainable, reliable, reproducible measurements as an inexpensive and routine method still used in orthodontic practice [23, 24]. Although several reports suggested using three dimensional (3-D) analysis of airway structures [25, 26], there are studies indicating the acceptance of using cephalograms [23, 24].
When skeletal parameters were considered, no pronounced skeletal effect of the appliance was found, similar to the literature [4, 12, 14, 15]. There was no significant increase in mandibular plane angle with the application of FFRD, which may be interpreted as no significant posterior rotation of the mandible, in accordance with previous studies [4, 5, 12, 14, 15]. There were increases in vertical maxillary and mandibular dimensions in both groups, and the increase was prominent in the control group when compared to the treatment group. This may reveal that the increases were due to growth rather than the treatment procedure and agree with those of Stahl et al. [27], who reported comparable millimetric vertical changes in the maxilla and the mandible in untreated skeletal Class II subjects.
Basic dentoalveolar changes after FFRD were reported as retrusion and extrusion of maxillary incisors, distalization of maxillary molars, mesial movement of mandibular molars, and labial flaring of mandibular incisors [4, 11–14]. Our results are consistent with these findings. FFRD group displayed prominent dentoalveolar changes especially at lower dentition relative to control group, declaring the effect of the device rather than the effect of growth. Mesial movement of lower molars by 1.33 mm and distal movement of upper molars by 0.31 mm contributed in improvement of Class II malocclusion. Protrusion of lower incisors by 2.81 mm was also evident when compared to control group, in accordance with previous reports [5, 12, 14]. The FFRD group achieved a 3.5-mm reduction of overjet than did the controls. Current changes in lower incisor and upper molar positions can also be held responsible for the significant increase in occlusal plane angle (SN/OP) in FFRD group. However, in their article evaluating the effects of FFRD treatment until the debonding of fixed orthodontic appliances, Cacciatore et al. [15] mentioned that the rotation in occlusal plane with FFRD insertion is transitory and that no significant changes occur at the end of treatment.
Present results revealed increased dimensions of the pharyngeal airway at soft palate level by 1.06 and 1.28 mm in FFRD group when compared to the control group, which was supported by reports emphasizing the positive influences of functional Class II treatments on airway dimensions [6, 8, 9, 20]. Jena et al. [19] declared that Class II functional orthopedic appliances provide more pronounced improvements in airway dimensions than do fixed functional appliances. This discrepancy might be attributed to the different treatment effects of functional and fixed functional appliances on skeletal and dentoalveolar structures [17]. A previous report indicated that palatopharynx and glossopharynx, where soft palate and tongue is situated, could adapt easily to the changes in oral cavity [28]. Within this framework, we found a positive correlation between the oropharyngeal airway dimensions and sagittal positions of lower incisors. From a clinical point of view, the protrusion of lower incisors achieved in the FFRD group might have caused a change in anterior border of the oral cavity occupied by the tongue. Correspondingly, mesialization of mandibular dentition might have provided more space to the tongue, revealing a postural change [21]. A previous report declared that in subjects with mandibular retrognathism, the tongue position is more backward with contact to the soft palate, resulting with the narrowing of the oropharyngeal airway [29]. Based on the results of Jena et al. [19], FFA appliances provide an anterior traction of the tongue away from the soft palate and reduced the pressure and caused an increase in airway dimensions. Germec-Cakan et al. [18] also found an increase in upper airway dimensions after molar mesialization and related this change with the possible increase in posterior tongue space. On the other hand, Kinzinger et al. [20] associated the increases in upper airway width to increases in the anterior facial height caused by fixed functional appliance. Our findings related to the significant differences in vertical maxillary and mandibular heights in FFRD group may also support this finding. In contrast to our results, Ozdemir et al. [21] reported no significant changes in oropharyngeal airway dimensions after fixed functional appliance treatment, although they found a significant increase in tongue space. The differences between these results could depend on the differences in ages, mean treatment times, and/or amount of mesial movement caused by the appliance.
The changes in hyoid bone position reflect the adaptation of the changes in tongue and the mandible. Post-treatment with FFRD therapy showed that the hyoid bone shifted significantly forward by 1.68 mm relative to controls, but no significant change in the vertical direction was found. This may have been achieved by the effect of the device because the hyoid bone shifted vertically in a lower position in the control group. Results of correlation analysis showed a positive correlation between airway dimensions at Cv2 cervical vertebral level with the sagittal position of the hyoid bone. Additionally, a negative correlation existed between airway dimensions at this level and the vertical position of the hyoid bone. Increased values of hyoid bone displacement to a more forward position and relatively stable vertical position might be linked with the adaptation of the tongue posture to the dentoalveolar mesialization achieved by the device. In contrast, situations where incisors were retracted and space of the tongue were restricted; the hyoid bone moved backward and downward to prevent the encroachment of the tongue into the pharyngeal airway [29, 30]. Thus, it can be reasonable to hypothesize that significant dental movements may cause dimensional changes in the airway track, especially at the level of soft palate and tongue.
In conclusion, findings of this study demonstrated prominent mesialization of the lower incisors and molars, forward positioning of the hyoid bone, and increased airway dimensions with the usage of FFRD appliance. In a clinical perspective, beneficial effects of these appliances on pharyngeal airway dimensions should be considered in Class II patients, especially for the ones with respiratory problems. However, since these findings represent the early effects of the appliance, studies are still needed to evaluate the long-term effects of fixed functional appliances on pharyngeal airway morphology.
References
McNamara Jr JA (1981) Components of class II malocclusion in children 8–10 years of age. Angle Orthod 51:177–202
Claudino LV, Mattos CT, Ruellas AC, Sant’ Anna EF (2013) Pharyngeal airway characterization in adolescents related to facial skeletal pattern: a preliminary study. Am J Orthod Dentofac Orthop 143:799–809
El H, Palomo JM (2013) An airway study of different maxillary and mandibular sagittal positions. Eur J Orthod 35:262–270
Gunay EA, Arun T, Nalbantgil D (2011) Evaluation of the immediate dentofacial changes in late adolescent patients treated with the Forsus(™) FRD. Eur J Dent 5:423–432
Franchi L, Alvetro L, Giuntini V, Masucci C, Defraia E, Baccetti T (2011) Effectiveness of comprehensive fixed appliance treatment used with the Forsus Fatigue Resistant Device in class II patients. Angle Orthod 81:678–683
Restrepo C, Santamaria A, Pelaez S, Tapias A (2011) Oropharyngeal airway dimensions after treatment with functional appliances in class II retrognathic children. J Oral Rehabil 38:588–594
Zhou L, Zhao Z, Lu D (2000) The analysis of the changes of tongue shape and position, hyoid position in class II, division 1 malocclusion treated with functional appliances (FR-I). Hua Xi Kou Qiang Yi Xue Za Zhi 18:123–125
Hanggi MP, Teuscher UM, Roos M, Peltomaki TA (2008) Long-term changes in pharyngeal airway dimensions following activator-headgear and fixed appliance treatment. Eur J Orthod 30:598–605
Ozbek MM, Memikoglu TU, Gögen H, Lowe AA, Baspinar E (1998) Oropharyngeal airway dimensions and functional-orthopedic treatment in skeletal class II cases. Angle Orthod 68:327–336
O’Brien K, Wright J, Conboy F, Sanjie Y, Mandall N, Chadwick S, et al. (2003) Effectiveness of treatment for class II malocclusion with the Herbst or twin-block appliances: a randomized, controlled trial. Am J Orthod Dentofac Orthop 124:128–137
Karacay S, Akin E, Olmez H, Gurton AU, Sagdic D (2006) Forsus nitinol flat spring and jasper jumper corrections of class II division 1 malocclusions. Angle Orthod 76:666–672
Aras A, Ada E, Saracoğlu H, Gezer NS, Aras I (2011) Comparison of treatments with the Forsus fatigue resistant device in relation to skeletal maturity: a cephalometric and magnetic resonance imaging study. Am J Orthod Dentofac Orthop 140:616–625
Jones G, Buschang PH, Kim KB, Oliver DR (2008) Class II non-extraction patients treated with the Forsus Fatigue Resistant Device versus intermaxillary elastics. Angle Orthod 78:332–328
Aslan BI, Kucukkaraca E, Turkoz C, Dincer M (2014) Treatment effects of the Forsus Fatigue Resistant Device used with miniscrew anchorage. Angle Orthod 84:76–87
Cacciatore G, Ghislanzoni LT, Alvetro L, Giuntini V, Franchi L (2014) Treatment and posttreatment effects induced by the Forsus appliance: a controlled clinical study. Angle Orthod 84:1010–1017
Servello DF, Fallis DW, Alvetro L (2015) Analysis of class II patients, successfully treated with the straight-wire and forsus appliances, based on cervical vertebral maturation status. Angle Orthod 85:80–86
Bilgiç F, Başaran G, Hamamci O (2015) Comparison of Forsus FRD EZ and Andresen activator in the treatment of class II, division 1 malocclusions. Clin Oral Investig 19:445–451
Germec-Cakan D, Taner T, Akan S (2011) Uvulo-glossopharyngeal dimensions in non-extraction, extraction with minimum anchorage, and extraction with maximum anchorage. Eur J Orthod 33:515–520
Jena AK, Singh SP, Utreja AK (2013) Effectiveness of twin-block and mandibular protraction appliance-IV in the improvement of pharyngeal airway passage dimensions in class II malocclusion subjects with a retrognathic mandible. Angle Orthod 83:728–734
Kinzinger G, Czapka K, Ludwig B, Glasl B, Gross U, Lisson J (2011) Effects of fixed appliances in correcting angle class II on the depth of the posterior airway space: FMA vs. Herbst appliance—a retrospective cephalometric study. J Orofac Orthop 72:301–320
Ozdemir F, Ulkur F, Nalbantgil D (2014) Effects of fixed functional therapy on tongue and hyoid positions and posterior airway. Angle Orthod 84:260–264
Li Y (2009) Early orthodontic treatment of skeletal class II malocclusion may be effective to prevent the potential for OSAHS and snoring. Med Hypotheses 73:594–595
Vizzotto MB, Liedke GS, Delamare EL, Silveira HD, Dutra V, Silveira HE (2012) A comparative study of lateral cephalograms and cone-beam computed tomographic images in upper airway assessment. Eur J Orthod 34:390–393
Pirila-Parkkinen K, Löppönen H, Nieminen P, Tolonen U, Paakkö E, Pirttiniemi P (2011) Validity of upper airway assessment in children: a clinical, cephalometric, and MRI study. Angle Orthod 81:433–439
Oh KM, Hong JS, Kim YJ, Cevidanes LS, Park YH (2011) Three-dimensional analysis of pharyngeal airway form in children with anteroposterior facial patterns. Angle Orthod 81:1075–1082
Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D (2009) Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofac Orthop 135:468–479
Stahl F, Baccetti T, Franchi L, McNamara Jr JA (2008) Longitudinal growth changes in untreated subjects with class II division 1 malocclusion. Am J Orthod Dentofac Orthop 134:125–137
Chen Y, Hong L, Wang CL, Zhang SJ, Cao C, Wei F, et al. (2012) Effect of large incisor retraction on upper airway morphology in adult bimaxillary protrusion patients. Angle Orthod 82:964–970
Muto T, Yamasaki A, Takeda S (2008) A cephalometric evaluation of the pharyngeal airway space in patients with mandibular retrognathia and prognathia, and normal subjects. Int J Oral Maxillofac Surg 37:228–231
Wang Q, Jia P, Anderson NK, Wang L, Lin J (2012) Changes of pharyngeal airway size and hyoid bone position following orthodontic treatment of class I bimaxillary protrusion. Angle Orthod 82:115–121
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bavbek, N.C., Tuncer, B.B., Turkoz, C. et al. Changes in airway dimensions and hyoid bone position following class II correction with forsus fatigue resistant device. Clin Oral Invest 20, 1747–1755 (2016). https://doi.org/10.1007/s00784-015-1659-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1659-1