Abstract
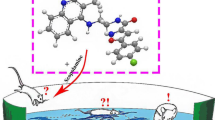
Tacrine is well-known drug for Alzheimer’s disease as an acetylcholinesterase inhibitor. Rember is a bright and promising AD drugs targeting tau protein, and it is currently in Phase III clinical trials. Phenothiazine, the key pharmacophore of Rember, can prevent tau filament formation. In this work, several tacrine-phenothiazine hybrids (T1–T26) were designed for inhibiting acetylcholinesterase and tau protein involved in Alzheimer’s disease. After initial screening with the help of computational chemistry software and Molegro Virtual Docker, three molecules (T5, T18, and T22) were selected for further synthesis and biological evaluation. Next, T5, T18, and T22 were synthesized and evaluated for their acetylcholinesterase and tau hyperphosphorylation inhibition. All the tested compounds had better acetylcholinesterase inhibitory activity compared with tacrine. Among them, compound T5 was found to be the most potent compound with IC50 89 nM. Meanwhile, T5 markedly prevented tau hyperphosphorylation induced by okadaic acid in N2α cell. Its P-tau level was decreased with 39.5 % inhibition when tested at 10−5 M, lower than that Rember (55.7 %). Besides acetylcholinesterase and tau hyperphosphorylation inhibition, T5 can also interact with fibrill beta amyloid using surface plasmon resonance, the data of KD were 5.51 × 10−8 M. All the above results indicated that tacrine-phenothiazine hybrids are potential multitarget directed ligands targeting acetylcholinesterase, tau protein, and beta amyloid.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD), the most common dementia in elderly people, is a complex neurodegenerative disorder of the central nervous system (CNS). It is characterized by the progressive deterioration of cognition and the emergence of behavioral and psychological symptoms. In AD brains, the cholinergic system is the most dramatically affected. Besides cholinergic deficiency, the abnormal formation of extracellular senile plaques (SP) consisting of aggregated beta amyloid (Aβ) peptide deposits and intracellular neurofibrillary tangles (NFTs) consisting of hyper-phosphorylated forms of the microtubule-associated tau protein is the most characteristic pathological hallmarks present in AD brain.
Current clinical therapy for AD is mainly palliative treatment targeting acetylcholinesterase (AChE) or N-methyl-D-aspartate (NMDA) receptor. AChE inhibitors (AChEIs) can increase the level of neurotransmitter in synaptic cleft, thereby improving cognition level of mild to moderate AD patients (Massoud and Guathier 2010). So far, four AChEIs (tacrine, donepezil, galamantine, and rivastigmine) and one NMDA receptor antagonist (memantine) have been approved by FDA. However, their role in the course of preventing AD is limited; none of them have proven effective against the progression of AD. Given that AChEIs and NMDA receptor antagonist have still been questioned and multifactorial nature of AD, the classic “one molecule, one target” solution may not be effective enough. Researchers are focusing on the development of new therapy strategies for arresting and reverting its progression. One general concept is multitarget directed ligand (MTDL) approach (Cavalli et al., 2008; Morphy and Rankovic, 2009), in which drugs are designed to address selected activities toward selected targets involved in the AD.
In line with MTDL paradigm, several multifunctional agents capable of hitting different biological targets have been developed and their biological profiles seem to be promising (Fernández-Bachiller et al., 2010; Bajda et al., 2011; Minarini et al., 2012; Rizzo et al., 2012).
It is the case of tacrine dimeric derivatives paved the way for the development of very interesting homodimer and heterodimer to prevent AD. An heptylene-tethered dimer of tacrine named bis (7)-tacrine (Fig. 1) is able to simultaneously contact the central anionic site (CAS) and the peripheral anionic site (PAS) (Pang et al., 1996), prevent glutamate-induced neuronal apoptosis by blocking NMDA receptor (Li et al., 2005; Luo et al., 2007), and reduce Aβ generation by directly inhibiting beta-site APP cleavage enzyme (BACE1) activity (Fu et al., 2008). As for the hybrid structure, it would reduce individual toxicity by special metabolic pathway compared with the combinational drugs. The recent studies following this strategy have led to the synthesis of several chemically diverse structures with dual or multiple biological profiles of AD, including AChE and monoamine oxidase B (MAO-B) dual inhibitors (Sterling et al., 2002); AChE and Aβ aggregation inhibitors (Kapkovά et al., 2006; Tumiatti et al., 2008; Ouberai et al., 2011); Aβ aggregation and peroxidase activity inhibitors (Ghadami et al., 2013); AChE and BACE1 dual inhibitors (Zhu et al., 2009); AChE, Aβ aggregation inhibiting, and antioxidant multiple functional compounds (Cavalli et al., 2007); and AChE, Aβ aggregation, and NMDA receptor inhibitor (Rosini et al., 2008). The biological activities of hybrids mentioned above have been improved by the introduction of the second or the third pharmacophores targeting Aβ, BACE1, NMDA, or some oxidases and others.
Nevertheless, many recent clinical studies showed that the treatment specially targeting Aβ had no effects on AD. Many drugs failed in phase III clinical trials, for example, Tarenflurbil developed by Myriad Genetics Company and Tramiprosate developed by Neurochem Company. On the other hand, the treatment targeting tau protein shows a bright future, a representative example is Rember developed by Taurx Company. 321 patients had participated in phase II clinical trials, it showed better efficacy. Phase III clinical trials are ongoing.
The aim of this study was to develop novel tacrine hybrids for their mainly inhibiting AChE and tau protein involved in the AD. It is reported that Rember (methylene blue, MB) can reduce soluble tau and regenerate cognition (O’Leary et al., 2010). Phenothiazine, the key pharmacophore of Rember also can prevent tau filament formation (Taniguchi et al., 2005). Herein, a series of tacrine-phenothiazine hybrids via an alkylenediamine-type spacer will be designed according to the principle of multitarget drugs design. These hybrids are expected to inhibit AChE and tau hyperphosphorylation and other targets involved in AD.
Results and discussion
Design and screen
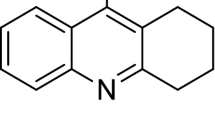
On the basis of tacrine and phenothiazine, two series of new hybrids (T1–T26) are designed, as shown in Fig. 2.
ADME properties of the designed 26 molecules were predicted using the web-based PreADMET (v2.0) (http://preadmet.bmdrc.org/) (Chitranshi et al., 2013; Lee et al., 2003). This gave an estimate of physiochemical properties and the bioavailability of the molecule. Fundamental physiochemical features of CNS drugs are related to their ability to penetrate the blood–brain barrier (BBB) and exhibit CNS activity. The molecule would regard as CNS penetrant with Cbrain/Cblood >0.1. The drug-likeness prediction of the 26 molecules is tabulated in Table 1. As could be seen from Table 1, all the molecules (T1–T26) exhibited general drug likeness. Their Cbrain/Cblood values are >0.1 besides T23 and T24, which reveal their potential BBB penetrability.
After initial ADME screening, the molecular docking technique was undertaken for the best tacrine-phenothiazine hybrids inhibiting AChE and tau hyperphosphorylation among 26 molecules. In addition to AChE as a target protein in the process of molecular docking, another target protein which affects tau hyperphosphorylation must be found. It has been recognized that an imbalanced regulation between protein kinases and protein phosphatases is a direct result of AD-like tau hyperphosphorylation (Hanger et al., 2009a). Among various kinases and phosphatases, glycogen synthase kinase-3β (GSK-3β) is the most implicated (Hanger et al., 2009b; Takashima, 2006). Herein, GSK-3β was selected as another target protein in the present work.
Once the two mainly target protein was established, MolegroVirtual Docker (MVD) 2009 trial was applied for further molecular docking studies. Docking procedures basically aim to identify the correct conformation of the molecule ligands in the binding pocket of the protein and to predict the affinity between the molecule ligand and the protein (Su, 2011).
The crystal structure of AChE complex with donepezil (Aricept) was retrieved from the Protein Data Bank (PDB ID: 1EVE). Aricept and water molecule were firstly removed followed with enzyme optimization. Similarly, the crystal structure of GSK-3β (PDB ID: 3GB2) was also retrieved. Finally, the minimized poses were recorded using MVD scoring function. Only top scoring molecule ligand was taken for further synthesis and biological evaluation.
The molecular docking studies of the 26 ligands are illustrated as representative case in Table 2. The present molecular docking studies showed relatively low MolDock Score (−82.259 kJ/mol) for tacrine, which indicates low affinity toward AChE. In general, the affinity of the ligands (T1–T26) toward AChE or GSK-3β was better than tacrine or donepezil. Among the 26 molecules, T5 had a significant affinity toward GSK-3β and a moderate affinity toward AChE. The MolDock Score of T5 toward GSK-3β was −148.821 kJ/mol; also its MolDock Score toward AChE (−183.585 kJ/mol) was slightly lower than bis (7)-tacrine (−190.66 kJ/mol). It was reported that bis (7)-tacrine had much better AChE inhibitory activity (IC50 = 1.5 nM) than tacrine (IC50 = 223 nM) (Carlier et al., 1997). Meanwhile, T18 was also found as a potential molecule, which had a significant affinity toward AChE (−202.166 kJ/mol) and good affinity toward GSK-3β. As for the affinity with GSK-3β, the MolDock Score of T18 (−143.581 kJ/mol) was slightly lower than the best T5 (−148.821 kJ/mol).
On the other hand, it is also found from Table 2 that the affinity of the hybrid molecules via piperazine connection (T22–T26) was generally worse than those of molecules via diamine connection (T1–T21). For example, T22 binded to AChE and GSK-3β with lower MolDock Score (−170.388 and −126.538 kJ/mol); even so, its MolDock Score was greater than tacrine or donepezil. Therefore, T5, T18, and T22 were selected as representative case for further synthesis and biological evaluation.
Chemistry
The synthesis route of T5 or T18 is shown in Scheme 1. Intermediates A, B, and C were prepared according to the literature (Hu et al., 2002; Tang et al., 2011; Darvesh et al., 2005) and slightly modified, respectively. Once the intermediate was available, the resulting diamine (B1 or B2) was reacted with C1 or C2 in the presence of base (K2CO3 or Et3N) to yield the desired T5 and T18. However, another new product (T5-B or T18-B) was also obtained, respectively, when we use CH2Cl2 or CH3COCH3 as reaction solvent under reflux condition. The two new products (T5/T5-B, T18/T18-B) were characterized as one or two molar amine displacement with slightly difference in molar ratio. Subsequently, the reactant ratio of B and C, reaction temperature, and reaction time were investigated for the optimal conditions of T5 or T18. Reducing temperature or shortening time was negative on the conversion of reactant and product yields. With the reaction processing and reactant consuming, the amount of T5-B or T18-B was on the increase and the proportion of the two new products was gradually reduced. T5 or T18 was not finally realized as unique product or main product even if the ratio of B and C was also changed. In addition, the type of solvents and bases had certain impact on the composition of the products. There are other by-products in the reaction mixture when we use triethylamine and CH3COCH3 instead of CH2Cl2 and K2CO3.
The synthesis procedure of T22 is outlined in Scheme 2. Chloroacetyl phenothiazine (C1) was reacted with excessive piperazine in the presence of K2CO3/KI, 1-(10H-phenothiazin-10-yl)-2-(piperazin-1-yl) ethanone (D) was obtained as the unique product. Next, the intermediate D was converted to the desired T22 using similar synthesis method of B1 or B2.
Biological evaluation
The preliminary anti-acetylcholinesterase activity for the synthesized tacrine derivatives (T5, T5-B, T18, T18-B, T22) was performed according to AChE enzyme-linked immunosorbent assay (ELISA) Kit using tacrine and donepezil as reference compound. AChE was obtained from homogenates of rat brain. Results of anti-AChE activity of the compounds are illustrated in Table 3. It is easily seen that all the tacrine derivatives exhibited better inhibitory activity against AChE than tacrine. From the biological activity studies, we also found that T5-B and T18-B demonstrated weaker AChE inhibition as compared to T5 or T18. Their bulk structure (T5-B, T18-B) was partially responsible for the lower AChE inhibition, which cannot efficiently enter into binding pocket of AChE. And as for the three desired tacrine hybrids (T5, T18, and T22), T5 was found to be the most potent compounds with IC50 89 nM, lower than donepezil with IC50 33 nM. T22 showed the lowest activity in the three compounds, its IC50 was 217 nM, slightly greater than tacrine (275 nM). The above-mentioned AChE inhibition results are consistent with the inhibition sequence (Table 2) predicted by MVD.
The effect of the tacrine hybrids (T5, T18, T22) on OA-induced P-Tau accumulation is shown in Table 4. The results were given by measuring the sum of P-Tau in OA-treated N2α cells with an ELISA assay. 12 h exposure of N2α cells to OA resulted in a significant increase in intracellular P-Tau generation, the P-Tau level reached to 68.6 ng/L compared with control group (22.8 ng/L). As shown in Table 4, a treatment with tacrine hybrids obviously prevented OA induced increase in the P-Tau level, which displayed inhibition higher than 25 % when tested at 10−5 M. Among the three hybrids, T5 was the most potent, which inhibited P-tau level by 39.5 % at 10−5 M. Even if the concentration of T5 was reduced to 10−7concentration of T5 wasM, the P-Tau inhibition (25.8 %) was almost equal to that of T22 at 10−5 M. At the same conditions, Rember displayed a percentage of inhibition ranged from 22.2 to 55.7 % when tested at 10−8 M–10−5 M.
On the basis of these promising results, T5 was also tested for its ability to bind with Aβ fibril (fAβ). Interaction of T5 with fAβ(1–40) was investigated by surface plasmon resonance (SPR) in grade concentrations at 0.625–40 μM for generation of binding curves. As shown in Fig. 3, distinct association and dissociation reactions were observed after the addition of freshly prepared T5 to immobilized fAβ(1–40), indicating that T5 could react with the immobilized fAβ. The responses of T5 reached equilibrium (Req) quickly and returned to baseline rapidly after dissociation. The binding response was calculated as the Req value divided by the molecular weight. The dose–response curve for T5 appeared to be monophasic, and it reached a saturation level at higher concentrations. The dissociation constant (KD) was calculated from data at dose ranging from 0.625 to 40 μM by steady-state analysis using BIA evaluation software (version 4.1). The KD of T5 to fAβ(1–40) was 5.51 × 10−8 M, lower than Congo Red (CR, positive control) with KD 6.78 × 10−7 M, while tacrine have no binding with fAβ(1–40) under the same condition.
Conclusion
The tacrine-phenothiazine hybrid has already been successful in the design of MTDL for combating the multifactorial nature of AD. In addition to its classic anti-AChE effects, tacrine-phenothiazine hybrid has been proven to be effective in inhibiting P-Tau and binding with Aβ fibrils when presenting in a multimeric form. These results expand the pharmacological profile of tacrine hybrids and may also help to design new chemical entities targeting tau protein.
Experimental section
Chemistry
The reagents used in the synthesis were purchased from Sinopharm Chemical Reagent Co. Ltd., and were used without further purification unless otherwise indicated. All the reactions were monitored using TLC. Column chromatography was performed using silica gel (200–300 mesh). All yields of the products refer to isolated yield.
Melting points were determined on YRT-3 apparatus and uncorrected. IR spectra were obtained on a Thermo Scientific Nicolet 8700 system. 1H NMR spectra were obtained on a Bruker Avance 300 (300 MHz) spectra or Agilent VNMRS 600 (600 MHz) with TMS as the internal standard, and chemical shifts were recorded in ppm along with coupling constants (J values) in Hz. Multiplicities were designated as singlet (s), broad singlet (br), doublet (d), triplet (t), and multiplet (m). Mass spectra (MS) were obtained by electrospray ionization (ESI) at 70 eV in a Finnigan LCQAdvantage MAX spectrometer with direct insertion probe. Elemental analysis (EA) was performed on an Elementar Analysensysteme GmbH Vario EL.
Synthesis of staring materials (compound A, B, C in Scheme 1 and compound D in Scheme 2)
9-chloro-1, 2, 3, 4-tetrahydroacridine (A, Scheme 1): pale yellow solid (This compound was prepared as follows: To a mixture of o-aminobenzoic acid (22 mmol, 3 g) and cyclohexanone (20 mmol, 2 g) 15 ml POCl3 at ice bath was carefully added. The mixture was heated under reflux for 4 h, then cooled to room temperature, and concentrated to give the slurry. The residue was diluted with ethyl acetate, neutralized with aqueous K2CO3, and washed with brine. The organic layer was dried over anhydrous K2CO3 and evaporated. The crude product was purified by flash chromatography to give the desired product. It was obtained as pale yellow solid, 3.4 g, 78 % yield); mp 69.0–69.8 °C; IR (KBr) υmax 2,936.1, 1,577.7, 1,552.6, 1,481.2, 754.0 cm−1; 1H NMR (CDCl3, 300 MHz): δ = 8.16 (1H, d, J = 8.4 Hz, H-8), 7.97 (1H, d, J = 8.4 Hz, H-5), 7.66 (1H, dd, J = 8.4, 9.6 Hz, H-6), 7.53 (1H, dd, J = 8.3, 9.6 Hz, H-7), 3.13 (2H, t, J = 6.0 Hz, H-4), 3.02 (2H, t, J = 5.4 Hz, H-1), 1.92–1.97 (4H, m, H-2 and H-3); 13C (CDCl3, 75 MHz): δ = 159.4 (C, C-12), 146.6 (C, C-13), 141.4 (C, C-9), 129.2 (C, C-11), 128.8 (CH, C-6), 128.5 (CH, C-5), 126.4 (CH, C-7), 125.3 (C, C-14), 123.6 (CH, C-8), 34.1 (CH2, C-4), 27.4 (CH2, C-1), 22.6 (CH2, C-3, C-2). ESI–MS: m/z [M + 1]+ 218.25.
N-(1, 2, 3, 4-tetrahyoacridin-9-yl) hexane-1, 6-diamine (B1, Scheme 1): brown oily liquid (This compound was prepared as follows: In a round-bottomed flask (100 ml) equipped with a magnetic stirrer, 9-chloro-1, 2, 3, 4-tetrahydroacridine (9 mmol, 1.95 g), sodium iodine (1.8 mmol, 300 mg), and phenol (54 mmol, 5.1 g) were stirred at 90 °C for 2 h and then hexane-1, 6-diamine (63 mmol, 7.32 g) was added. The reaction temperature was raised to 120 °C and maintained 4 h. The mixture was cooled to room temperature and diluted with CHCl3 and made basic with 10 % NaOH solution. The organic layer was washed with water and brine and dried over anhydrous MgSO4. The filtrate was evaporated and the residue was purified on silica gel column chromatography (CH2Cl2/MeOH/NH3·H2O = 9:1:0.1) to give the brown oily product, 1.86 g, 70 % yield); IR (film) υmax 3,359.0, 2,929.6, 1,563.3, 1,131.8, 764.4 cm−1; 1H NMR (CDCl3, 300 MHz): δ = 7.90–7.97 (2H, m, H-5, H-8), 7.52–7.58 (1H, m, H-6), 7.32–7.37 (1H, m, H-7), 3.98 (2H, br, NH2), 3.45–3.52 (2H, m, CH 2 NH), 3.07 (2H, m, H-4), 2.66–2.72 (4H, m, H-1, CH 2 NH2), 1.91–1.95 (4H, m, H-2, H-3), 1.62–1.72 (2H, m, CH 2 CH2NH2), 1.48–1.69 (6H, m, (CH 2 )3CH2CH2NH2); 13C (CDCl3, 75 MHz): δ = 158.4 (C, C-12), 150.7 (C, C-9), 147.1 (C, C-13), 128.6 (CH, C-6), 128.3 (CH, C-5), 123.6 (CH, C-7), 122.7 (CH, C-8), 120.1 (C, C-14), 115.9 (C, C-11), 51.8 (CH2, CH2NH), 49.1 (CH2, CH2NH2), 33.9 (CH2, C-4), 32.1 (CH2, CH2CH2NH2), 31.2 (CH2, CH2CH2NH), 26.8 (CH2, CH2CH2CH2NH2), 25.6 (CH2, CH2CH2CH2NH), 24.5 (CH2, C-1), 22.9 (CH2, C-3, C-2).
N-(1, 2, 3, 4-tetrahyoacridin-9-yl) butane-1, 4-diamine (B2, Scheme 1): brown oily liquid (Prepared following the general procedure of B1 and starting from butane-1, 4-diamine (63 mmol, 5.55 g). The brown oily product B2 was obtained by chromatography (CH2Cl2/MeOH/NH3·H2O = 10:1:0.1), 1.62 g, 67 % yield); IR (film) υmax 3,358.1, 2,931.2, 1,561.5, 1,129.8, 768.4 cm−1; 1H NMR (CDCl3, 300 MHz): δ = 7.89–7.96 (2H, m, H-5, H-8), 7.53–7.57 (1H, m, H-6), 7.32–7.36 (1H, m, H-7), 4.01 (2H, br, NH2), 3.46–3.50 (2H, m, CH 2 NH), 3.11 (2H, m, H-4), 2.73–2.79 (4H, m, H-1, CH 2 NH2), 1.97–1.99 (4H, m, H-2, H-3), 1.39–1.63 (4H, m, (CH 2 )2CH2NH2); 13C (CDCl3, 75 MHz): δ = 158.0 (C, C-12), 150.1 (C, C-9), 147.1 (C, C-13), 128.7 (CH, C-6), 128.1 (CH, C-5), 123.6 (CH, C-7), 122.3 (CH, C-8), 120.1 (C, C-14), 115.9 (C, C-11), 51.5 (CH2, CH2NH), 48.9 (CH2, CH2NH2), 33.6 (CH2, C-4), 31.0 (CH2, CH2CH2NH2), 29.8 (CH2, CH2CH2NH), 24.8 (CH2, C-1), 22.8 (CH2, C-3, C-2).
2-chloro-1-(10H-phenothiazin-10-yl) ethanone (C1, Scheme 1): off-white solid (This compound was prepared as follows: A solution containing phenothiazine (26 mmol, 5.248 g), 2-chloroacetyl chloride (66 mmol, 7.45 g, 5.5 ml), and triethylamine (26 mmol, 4 ml) in dichloromethane (100 ml) was refluxed with stirring. After about 2–3 h reflux period, TLC analysis revealed that all phenothiazine were consumed. The reaction mixture was cooled to room temperature and then washed successively with 5 % aqueous sodium bicarbonate, 5 % hydrochloric acid, and water. The solution was dried over MgSO4, filtered, and evaporated. The crude product was purified by flash column chromatography with dichloromethane as elute and recrystallized from petroleum ether/dichloromethane (2:1). Finally, the desired product C1 was obtained as off-white solid, 3.6 g, 50 % yield.); mp 110.3-111.0 °C; IR (KBr) υmax 1,693.1, 1,671.7, 1,335.1, 1,247.9, 1,170.3, 1,125.6, 761.6 cm−1; 1H NMR (CDCl3, 300 MHz): δ = 7.60 (2H, d, J = 7.8 Hz, H-1, H-9), 7.48 (2H, d, J = 7.8 Hz, H-4, H-6), 7.33-7.38 (2H, m, H-2, H-8), 7.24–7.30 (2H, m, H-3, H-7), 4.18 (2H, s, CH 2Cl); 13C (CDCl3, 75 MHz): δ = 165.4 (C, CON), 137.8 (C, CH, C-11, C-14, C-4, C-6), 128.1 (CH, C-2, C-8), 127.3 (CH, C-1, C-9, C-3, C-7), 126.5 (C, C-12, C-13), 41.8 (CH2, CH2Cl).
4-chloro-1-(10H-phenothiazin-10-yl) butan-1-one (C2, Scheme 1): off-white solid (Prepared following the general procedure of C1 and starting from 4-chlorobutanoyl chloride (66 mmol, 9.3 g). The crude product was purified by column chromatography with petroleum ether/ethyl acetate (4:1) as elute, C2 was obtained as off-white solid, 3.3 g, 42 % yield); mp 118.0–118.8 °C; IR (KBr) υmax 1,693.4, 1,672.0, 1,336.1, 1,248.5, 1,170.3, 1,126.8, 762.0 cm−1; 1H NMR (CDCl3, 300 MHz): δ = 7.58 (2H, d, J = 7.6 Hz, H-1, H-9), 7.47 (2H, d, J = 7.6 Hz, H-4, H-6), 7.36–7.38 (2H, m, H-2, H-8), 7.26–7.30 (2H, m, H-3, H-7), 3.43 (2H, t, J = 7.5 Hz, CH 2 Cl), 2.26 (2H, t, J = 4.8 Hz, COCH2), 2.01 (2H, m, CH 2 CH2Cl); 13C (CDCl3, 75 MHz): δ = 172.5 (C, CON), 135.9 (C, CH, C-11, C-14, C-4, C-6), 128.2 (CH, C-2, C-8), 126.1 (CH, C-1, C-9, C-3, C-7), 124.9 (C, C-12, C-13), 42.9 (CH2, CH2Cl), 31.3(CH2, COCH2), 27.3 (CH2, CH2CH2Cl).
1-(10H-phenothiazin-10-yl)-2-(piperazin-1-yl) ethanone (D, Scheme 2): white solid (This compound was prepared as followings: To a solution containing chloroacetyl phenothiazine (7.2 mmol, 2.0 g), piperazine (36 mmol, 3.1 g), and potassium iodine (7.2 mmol, 1.2 g) in N, N-dimethyl formamide (100 ml) was carefully added anhydrous K2CO3 (7.2 mmol, 0.995 g) at room temperature. After about 10 h reaction period with stirring, TLC analysis revealed that chloroacetyl phenothiazine was consumed. N, N-dimethyl formamide and excess piperazine were removed under vacuum condition. The residue was poured into water and extracted with ethyl acetate; the organic layer was combined and washed with water and brine, dried over anhydrous Na2SO4, filtered, and evaporated. The desired product D was obtained as white solid, 1.99 g, 85 % yield); mp 140.8–141.5 °C; IR (KBr) υmax 3,316.6, 1,668.6, 1,460.0, 1,325.1, 1,261.2, 1,132.3, 773.7 cm−1; 1H NMR (CDCl3, 300 MHz): δ = 7.51–7.56 (2H, m, H-1′, H-9′), 7.41–7.46 (2H, m, H-4′, H-6′), 7.19–7.34 (4H, m, H-2′, H-3′, H-7′, H-8′), 3.29(2H, s, CH 2 CO), 2.71–2.74 (4H, m, CH 2 NCH 2 ), 2.39–2.32 (4H, m, CH 2 NHCH 2 ), 1.99 (1H, br, NH); 13C NMR (CDCl3, 75 MHz): δ = 168.6 (C, CON), 138.7 (C, CH, C-11′, C-14′, C-4′, C-6′), 127.8 (CH, C-2′, C-8′, C-1′, C-9′), 126.9 (CH, C-3′, C-7′), 126.7 (C, C-12′, C-13′), 60.9 (CH2, COCH2), 54.0 (CH2, NCH2), 45.9 (CH2, NHCH2). ESI–MS: m/z [M + 1]+ 326.1. Anal. Calcd. for C18H19N3OS: C, 66.43; H, 5.88; N, 12.91. Found: C, 66.40; H, 5.78; N, 12.87.
Synthesis of the desired products (T5, T5-B, T18, T18-B in Scheme 1 and T22 in Scheme 2)
1-(10H-phenothiazin-10-yl)-2-(6-(5, 6, 7, 8-tetrahydroacridin-9-ylamino) hexylamino) ethanone (T5, Scheme 1): yellow foam (This compound was prepared as follows: To a solution of B1 (3 mmol, 891 mg) in dry dichloromethane, potassium carbonate (3 mmol, 416 mg) and potassium iodine (0.3 mmol, 50 mg) were added, the resulting mixture was stirred at room temperature for 1 h. Then, C1 (3 mmol, 828 mg) was added and the reaction mixture was refluxed for 10–12 h. Then, the mixture was cooled to room temperature and water was poured, the organic layer was combined and washed with water and brine, dried over Na2SO4, filtered, and evaporated. The crude product was purified by column chromatography (CH2Cl2/MeOH/NH3·H2O = 15:1:0.1). The desired product T5 was obtained as yellow foam, 338 mg, 21 % yield); IR (KBr) υmax 3,352.9, 3,061.3, 1,679.8, 1,457.8, 763.1 cm−1; 1H NMR (CDCl3, 300 MHz): δ = 8.09–8.21 (1H, m, H-5), 7.93–7.96 (1H, m, H-8), 7.54–7.63 (1H, m, H-6), 7.14–7.48 (9H, m, H-7, Ar–H in phenothiazine), 4.30 (1H, br, NH), 3.63 (2H, s, COCH 2 ), 3.45–3.49 (2H, m, CH 2 NHAr), 3.11 (2H, m, H-4), 2.53–2.64 (4H, m, H-1, CH 2 NH), 1.89–1.91 (4H, m, H-2, H-3), 1.62–1.73 (2H, m, CH 2 CH2NH), 1.18–1.26 (6H, m, (CH 2 )3CH2CH2NH); 13C NMR (CDCl3, 75 MHz): δ = 164.7 (C, C-12), 163.5 (C, CON), 148.3 (C, C-9), 145.2 (C, C-13), 133.1 (C, C-11′, C-14′), 132.0 (CH, C-4′, C6′) 128.1 (C, Ar), 124.3 (C, Ar), 118.5 (C, Ar), 114.9 (C, Ar), 50.9 (CH2, COCH2), 48.6 (CH2, CH2NHAr), 45.7 (CH2, CH2NH), 35.2 (CH2, C-4), 31.2 (CH2, CH2CH2NHAr), 30.3 (CH2, CH2CH2NH), 26.9 (CH2, CH2 CH2CH2CH2NH), 24.0 (CH2, C-1), 22.5 (CH2, C-2, C-3); ESI–MS: m/z [M + 1]+ 537.3; Anal. Calcd. for C33H36N4OS: C, 73.85; H, 6.76; N, 10.44. Found C, 73.80; H, 6.65; N, 10.43.
2,2′-(6-(5,6,7,8-tetrahydroacridin-9-ylamino)hexylazanediyl)bis(1-(10H-phenothiazin-10-yl)ethanone) (T5-B, Scheme 1): yellow foam (In the preparation process of T5, another product T5-B was obtained as a yellow foam by column chromatography, 628 mg, 27 % yield); IR (KBr) υmax 3,356.9, 3,059.7, 2,929.7, 1,678.3, 1,460.6, 760.8 cm−1; 1H NMR (CDCl3, 600 MHz): δ = 8.63 (1H, d, J = 8.5 Hz, H-5), 8.11 (1H, d, J = 8.6 Hz, H-8), 7.68–7.72 (1H, m, H-6), 7.37–7.47 (9H, m, H-7, Ar–H in phenothiazine), 7.16–7.29 (8H, m, Ar–H in phenothiazine), 5.57 (1H, m, NHAr), 3.61–3.75 (6H, m, COCH 2 , COCH 2 , CH 2 NH), 3.26–3.38 (2H, m, H-4), 2.48–2.60 (4H, m, H-1, CH 2 N), 1.86–1.89 (4H, m, H-2, H-3), 1.66–1.70 (2H, m, CH 2 CH2NH), 1.29–1.35 (2H, m, CH 2 CH2N), 1.17–1.22 (4H, m, CH 2 CH 2 CH2CH2NH); 13C NMR (CDCl3, 150 MHz): δ = 169.8 (C, C-12, CON), 138.3 (C, Ar), 127.9 (C, Ar), 126.9 (C, Ar), 126.8 (C, Ar), 124.0 (C, Ar), 123.4 (C, Ar), 55.0 (CH2, COCH2), 53.9 (CH2, NCH2), 48.9 (CH2, NHCH2), 31.2 (CH2, C-4), 29.6 (CH2, NHCH2 CH2), 28.9 (CH2, NHCH2CH2 CH2), 27.6 (CH2, NCH2 CH2), 26.6 (CH2, NCH2CH2 CH2), 24.3 (CH2, C-1), 22.5 (CH2, C-3), 21.9 (CH2, C-2); ESI–MS: m/z [M + 1]+ 776.4; Anal. Calcd. for C47H45N5O2S2: C, 72.74; H, 5.84; N, 9.02. Found C, 72.70; H, 5.73; N, 9.00.
1-(10H-phenothiazin-10-yl)-4-(4-(5, 6, 7, 8-tetrahydroacridin-9-ylamino) butylamino)butan-1-one (T18, Scheme 1): yellow foam (Prepared following the general procedure of T5 and starting from B2 (3 mmol, 807 mg) and C2 (3 mmol, 914 mg). The crude products were purified by column chromatography (CH2Cl2/MeOH/NH3·H2O = 15:1:0.1), the desired product T18 was obtained as yellow foam, 306 mg, 19 % yield); IR (KBr) υmax 3,357.7, 3,058.2, 1,680.7, 1,460.0, 760.1 cm−1; 1H NMR (CDCl3, 600 MHz): δ = 8.07–8.15 (1H, m, H-5), 7.95–7.99 (1H, m, H-8), 7.60–7.68 (2H, m, H-6, H-7), 7.11–7.51 (8H, m, Ar–H in phenothiazine), 4.36 (1H, br, ArNH), 3.35–3.43 (2H, m, CH 2 NHAr), 2.98–3.11 (2H, m, H-4), 2.54–2.63 (6H, m, CH 2 NHCH 2 , H-1), 2.21–2.35 (2H, m, COCH 2 ), 1.75–1.91 (6H, m, H-2, H-3, CH 2 CH2CO), 1.42–1.61 (4H, m, CH 2 CH 2 CH2NHAr); 13C NMR (CDCl3, 150 MHz): δ = 174.5 (C, CON), 164.0 (C, C-12), 147.0 (C, C-9), 145.2 (C, C-13), 133.1 (C, C-11′, C-14′), 132.1 (CH, C-4′, C-6′), 128.1 (C, Ar), 124.5 (C, Ar), 118.9 (C, Ar), 115.3 (C, Ar), 50.9 (CH2, NHCH2), 49.3 (CH2, CH2NH), 45.0 (CH2, CH2NHAr), 36.9 (CH2, C-4), 31.7 (CH2, COCH2), 27.9 (COCH2 CH2 CH2NHCH2 CH2 CH2), 24.9 (CH2, C-1), 23.0 (CH2, C-2, C-3); ESI–MS: m/z [M + H]+ 537.3. Anal. Calcd. for C33H36N4OS: C, 73.85; H, 6.76; N, 10.44. Found C, 73.83; H, 6.71; N, 10.39.
4,4′-(4-(5,6,7,8-tetrahydroacridin-9-ylamino)butylazanediyl)bis(1-(10H-phenothiazin-10-yl)butan-1-one) (T18-B, Scheme 1): yellow foam (In the preparation process of T18, another product T18-B was obtained as yellow foam by column chromatography, 675 mg, 28 % yield); IR (KBr) υmax 3,360.5, 3,058.2, 1,675.7, 1,463.5, 765.1 cm−1; 1H NMR (CDCl3, 600 MHz): δ = 8.58 (1H, d, J = 8.5 Hz, H-5), 8.09 (1H, d, J = 8.6 Hz, H-8), 7.68–7.72 (1H, m, H-6), 7.33-7.48 (9H, m, H-7, Ar–H in phenothiazine), 7.16–7.28 (8H, m, Ar–H in phenothiazine), 5.48 (1H, m, NHAr), 3.45–3.60 (2H, m, CH 2 NHAr), 3.11-3.19 (2H, m, H-4), 2.48–2.60 (8H, m, H-1, (CH 2 )3N), 2.25–2.34 (4H, m, CH 2 CO), 1.66–1.70 (8H, m, H-2, H-3, CH 2 CH2CO), 1.35–1.57 (m, 4H, CH 2 CH 2 CH2NH); 13C NMR (CDCl3, 150 MHz): δ = 175.0 (C, CON), 164.9 (C, C-12), 146.3 (C, C-9, C-13), 130.9 (C, Ar), 129.1 (C, Ar), 125.3 (C, Ar), 119.5 (C, Ar), 54.9 (CH2, CH2N), 53.1 (CH2, CH2N), 46.8 (CH2, CH2NH), 34.2 (CH2, C-4), 30.8 (CH2, CH2CO), 27.6 (CH2, CH2CH2NHAr), 25.9 (CH2, CH2CH2N), 24.3 (CH2, C-1), 21.9 (CH2, C-2, C-3); ESI–MS: m/z [M + 1]+ 804.3. Anal. Calcd. for C49H49N5O2S2: C, 73.19; H, 6.14; N, 8.71. Found C, 73.15; H, 6.11; N, 8.70.
1-(10H-phenothiazin-10-yl)-2-(4-(5, 6, 7, 8-tetrahydroacridin-9-yl) piperazin-1-yl) ethanone (T22, Scheme 2): brown oily liquid (Prepared following the general procedure for the synthesis of B1 or B2. The starting material of the reaction included 9-chloro-1, 2, 3, 4-tetrahydroacridine (2 mmol, 435 mg), sodium iodine (0.3 mmol, 45 mg), phenol (8 mmol, 752 mg), and Compound D (2.5 mmol, 814 mg). The brown oily product T22 was obtained by column chromatography (CH2Cl2/MeOH/NH3·H2O = 15:1:0.1), 679 mg, 67 % yield); IR (KBr) υmax 2,925.6, 1,682.6, 1,460.1, 1,262.6, 1,126.6, 761.3 cm−1; 1H NMR (CDCl3, 600 MHz): δ = 8.05–8.09 (1H, m, H-5), 7.93-7.99 (1H, m, H-8), 7.48–7.60 (6H, m, Ar–H), 7.25–7.38 (4H, m, Ar–H in phenothiazine), 3.47 (2H, s, CH 2 CO), 3.19–3.27 (4H, m, CH 2 NAr), 3.09–3.11 (2H, t, J = 6.6 Hz, H-4), 2.86–2.89 (2H, t, J = 6.6 Hz, H-1), 2.58–2.69 (4H, m, CH2N), 1.91–1.93 (2H, m, H-2), 1.82–1.85 (2H, m, H-3); 13C NMR (CDCl3, 150 MHz): δ = 168.9 (C, C-12), 160.5 (C, CON), 153.0 (C, C-9), 147.9 (C, C-13), 138.9 (C, C-11′, C-14′), 128.8 (C, Ar), 128.5 (C, Ar), 128.1 (C, Ar), 127.9 (C, Ar), 127.2 (C, Ar), 127.0 (C, Ar), 126.0 (C, Ar), 125.0 (C, Ar), 124.1 (C, Ar), 60.8(CH2, CH2CO), 53.9 (CH2, CH2N), 50.5 (CH2, CH2N), 34.2 (CH2, C-4), 32.1 (CH2, C-1), 22.9 (CH2, C-2, C-3); ESI–MS: m/z [M + 1]+ 507.3. Anal. Calcd. for C31H30N4OS: C, 73.49; H, 5.97; N, 11.06. Found: C, 73.40; H, 5.86; N,11.05.
Biological evaluation
In vitro estimation of acetylcholinesterase inhibitory activity
The preliminary anti-acetylcholinesterase activity for the synthesized compounds was performed according to AChE enzyme-linked immunosorbent assay (ELISA) Kit (96T, R&D system) using tacrine and donepezil as reference compound. AChE was obtained from homogenates of rat brain. Test compounds (T5, T5-B, T18, T18-B, T22) were dissolved in DMSO and diluted with DMSO-H2O and rat brain homogenates, the final concentration ranged from 0.01 to 100 μM. Blank was prepared using rat brain homogenates instead of the test sample, and all other procedures were similar to those used in the case of the sample mixture. Absorbance (OD) was measured at 450 nm using microplate reader (DG5033A, Nanjing Huadong Electronics Group Co. Ltd.,). The AChE content in sample is positively correlated with OD. AChE content in the negative control hole as 100 %, the reduction of AChE content in test samples hole is the enzyme inhibition rate. Experiments were done in triplate. Data are expressed as mean ± standard deviation (SD) and were analyzed using SPSS 19.0 statistical software.
In vitro estimation of P-Tau inhibitory activity
The N2α cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM) containing 10 % fetal bovine serum (GIBCO). Cells were grown in a 100 % humidified incubator at 37 °C with 5 % CO2 and passaged 2–3 days prior to use. Logarithmic phase’s N2α cells were seeded in 96-well plates at a density of 104 cells per well. After growing for 12 h, the cells were incubated in DMEM containing 60 nM okadaic acid (OA, Sigma Chemical Co.) for 12 h. Then, test compound (or other compound) with final concentration of 10−4 M, 10−5 M, 10−6 M, 10−7 M, or 20 μM methylene blue (Rember) were added to the culture medium and incubated with the cells for 24 h. Cells were washed twice with ice-cold PBS, homogenized in RIPA Lysis buffer (Solarbio Science & Technology Co.) for 5 min on ice, and the lysate was centrifugated at 14,000g for 5 min at 4 °C prior to ELISA detection. For quantitative analysis of P-Tau in cell lysates, the assay was performed as described in the instructions of the P-Tau ELISA Kit (Innogenetics NV Co.). Experiments were done in triplate. Data are expressed as mean ± standard deviation (SD) and were analyzed using SPSS 19.0 statistical software.
Aβ fibril (fAβ) binding study by surface plasmon resonance (SPR)
A BIAcore 3,000 (Biacore Inc., USA) equipped with four flow cell channels on sensor chip was used for real-time binding studies. Carboxymethylated dextran 5 (CM5) sensor chip was used in this experiment for fAβ(1–40). fAβ(1–40) stored at 4 °C was centrifuged at 4 °C for 2 h at 16,000 g. fAβ(1–40) precipitated completely, and the pellet was resuspended in water, sonicated, diluted with 10 mM sodium acetate (pH 4.0), and immobilized immediately on CM5 sensor chip by amine coupling. fAβ(1–40) was immobilized on the CM5 chip in the second channel, and the first channel was used as a reference(without immobilization of fAβ(1–40)). The carboxymethyl dextran surface was activated using 70μL of a mixture of 0.4 M N-ethyl-N′-[3-(dimethylamino)propyl] carbodiimide hydrochloride(EDC) and 0.1 M N-hydroxysuccinimide (NHS) at an injection rate of 10 μL/min, followed by the injection of fAβ(1–40) into channel 2 (70 μL of fAβ diluted with 600 μL of PH 4.0 sodium acetate buffer and injected at a rate of 5 μL/min).
After fAβ immobilization, the remaining activated groups were blocked with 70 μL of 1.0 M ethanolamine (pH 9.0). The reference cell was prepared by the above described amine coupling without the addition of fAβ. The running buffer solution contained 50 mM phosphate buffer (pH 7.5), 100 mM NaCl, 0.3 mM EDTA, and 0.05 % Tween 20, and the washing solvent contained 1 % DMSO.
After immobilization, test compounds with different concentrations were injected into the cell, and binding was observed. Each binding experiment was repeated three times, and the reaction was performed 25 °C using running buffer solution mentioned above. Test compound (T5) dissolved in DMSO was diluted with running buffer to a final concentration of 0.625–40 μM and injected over the reference and fAβ-immobilized flow cells at a flow rate of 30 μL/min. The surface of sensor chip immobilized with fAβ was regenerated with a mixture of 0.025 % sodium laurel sulfated (SDS) and 25 mM NaOH. Data from the reference cell without fAβ immobilization were subtracted from raw data. The running buffer injection using the same method was also subtracted as a double reference (Yan et al., 2007).
References
Bajda M, Guzior N, Ignasik M, Malawska B (2011) Multi-target-directed ligands in Alzheimer’s disease treatment. Curr Med Chem 18:4949–4975
Carlier PR, Han YF, Chow ES-H, Li CP-L, Wang H, Lieu TX, Wong HS, Pang Y-P (1997) Evaluation of short-tether bis-THA AChE inhibitors. A further test of the dual binding site hypothesis. Bioorg Med Chem 7:351–357
Cavalli A, Bolognesi ML, Capsoni S, Andrisano V, Bartolini M, Margotti E, Cattaneo A, Recanatini M, Melchiorre C (2007) A small molecule targeting the multifactorial nature of Alzheimer’s disease. Angew Chem Int Ed 46:3689–3692
Cavalli A, Bolognesi ML, Minarini A, Rosini M, Tumiatti V, Recanatini M, Melchiorre C (2008) Multi-target-directed ligands to combated neurodegenerative diseases. J Med Chem 51:347–370
Chitranshi N, Gupta S, Tripathi PK, Seth PK (2013) New molecular scaffolds for the design of Alzheimer’s acetylcholinesterase inhibitors identified using ligand and receptor-based virtual screening. Med Chem Res 22:2328–2345
Darvesh S, McDonald RS, Renwell A, Conrad S, Darvesh KV, Mataija D, Comez G, Caines A, Walsh R, Martin E (2005) Structure-activity relationships for inhibition of human cholinesterase’s by alkyl amide phenothiazine derivative. Bioorg Med Chem 13:211–222
Fernández-Bachiller MI, Pérez C, González-Muñoz GC, Conde S, López MG, Villarroya M, García AG, Rodríguez-Franco MI (2010) Novel tacrine-8-hydroxyquinoline hybrids as multifunctional agents for the treatment of Alzheimer’s diseases, with neuroprotective, cholinergic, antioxidant, and copper-complexing properties. J Med Chem 53:4927–4937
Fu HJ, Li WM, Luo JL, Lee NTK, Li MT, Tsim KWK, Pang YP, Youdim MBH, Han YF (2008) Promising anti-Alzheimer’s dimer bis(7)-tacrine reduces β-amyloid generation by directly inhibiting BACE-1 activity. Biochem Biophys Res Commun 366:631–636
Ghadami SA, Hossein-pour Z, Khodarahmi R, Ghobadi S, Adibi H (2013) Synthesis and in vitro characterization of some benzo thiazole and benzofuranone-derivatives for quantification of fibrillar aggregates and inhibition of amyloid-mediated peroxidase activity. Med Chem Res 22:115–126
Hanger DP, Anderton BH, Noble W (2009a) Tau phosphorylation: the therapeutic challenge for neurodegenerative disease. Trends Mol Med 15:112–119
Hanger DP, Seereeram A, Noble W (2009b) Mediators of Tau phosphorylation in the pathogenesis of Alzheimer’s disease. Exp Rev Neurother 9:1647–1666
Hu MK, Wu LJ, Hsiao G, Yen MH (2002) Homodimeric tacrine congener’s asacetylcholinesterase inhibitions. J Med Chem 45:2277–2282
Kapkovά P, Alptüzün V, Frey P, Erciyas E, Holzgrabe U (2006) Search for dual function inhibitors for Alzheimer’s disease: synthesis and biological activity of acetylcholinesterase inhibitors of pyridinium-type and their Aβ fibril formation inhibition capacity. Bioorg Med Chem 14:472–478
Lee SK, Lee IH, Kim HJ, Chang GS, Chung JE, No KT (2003) The PreADME approach: web-based program for rapid prediction of physic-chemical, drug absorption and drug-like properties, Euro QSAR 2002 Designing drugs and crop protectants: processes, problems and solutions. Blackwell, Boston, pp 418–420
Li WM, Pi RB, Chan HHN, Fu HJ, Lee NTK, Tsang HW, Pu YM, Chang DC, Li CC, Luo JL, Xiong KM, Li ZW, Xue H, Carlier PR, Pang YP, Tsim KWK, Li MT, Han YF (2005) Novel dimeric acetylcholinesterase inhibitor bis(7)-tarcrine, but not donepezil, prevents glutamate-induced neuronal apoptosis by blocking N-methyl-D-aspartate receptors. J Biol Chem 280:18179–18188
Luo JL, Li WM, Liu YW, Zhang W, Fu HJ, Lee NTK, Yu H, Pang YP, Huang PB, Xia J, Li ZW, Li CY, Han YF (2007) Novel dimer bis(7)-tacrine proton-dependently inhibits NMDA-activated currents. Biochem Biophys Res Commun 361:505–509
Massoud F, Guathier S (2010) Update on the pharmacological treatment of Alzheimer’s disease. Curr Neuropharmacol 8:69–80
Minarini A, Milelli A, Rumiatti V, Rosini M, Simoni E, Bolognesi ML, Andrisano V, Bartolini M, Motori E, Angeloni C, Hrelia S (2012) Cystamine-tacrine dimer: a new multi-target-directed ligand as potential therapeutic agent for Alzheimer’s disease treatment. Neuropharmacology 62:997–1003
Morphy R, Rankovic Z (2009) Designing multiple ligands-medicinal chemistry strategies and challenges. Curr Pharm Des 15:587–600
O’Leary JC, Li QY, Marinec P, Blair LJ, Congdon EE, Johnson AG, Jinwal UK, Koren J, Jones JR, Kraft C, Peters M, Abisambra JF, Duff KE, Weeber EJ, Gestwick JE, Dickey CA (2010) Phenothiazine-mediated rescue of cognition in tau transgenic mice requires neuroprotection and reduced soluble tau burden. Mol Neurodegener 5:45–55
Ouberai M, Brannstrom K, Vestling M, Olofsson A, Dumy P, Chierici S, Garcia J (2011) Clicked tacrine conjugates as acetylcholinesterase and β-amyloid directed compounds. Org Biomol Chem 9(4):1140–1147
Pang Y-P, Quiram P, Jelaric T, Hong F, Brimijoin S (1996) Highly potent, selective, and low cost bis-tetrahydroaminacrine inhibitors of acetylcholinesterase: steps toward novel drugs for treating Alzheimer’s disease. J Biol Chem 271:23646–23649
Rizzo S, Tarozzi A, Bartolini M, Costa GD, Bisi A, Gobbi S, Belluti F, Ligresti A, Allará M, Monti JP, Andrisano V, Marzo VD, Hrelia P, Rampa A (2012) 2-arylbenzofuran-based molecules as multipotent Alzheimer’s disease modifying agents. Eur J Med Chem 58:519–532
Rosini M, Simoni E, Bartolini M, Cavalli A, Ceccarini L, Pascu N, McClymont DW, Tarozzi A, Bolognesi ML, Minarini A, Tumiatti V, Andrisano V, Mellor IR, Melchiorre C (2008) Inhibition of acetylcholinesterase, β-amyloid aggregation, and NMDA acceptors in Alzheimer’s disease: a promising direction for the multi-target-directed ligands gold rush. J Med Chem 51:4381–4384
Sterling J, Herzig Y, Goren T, Finkelstein N, Lerner D, Goldenberg W, Miskolczi I, Molnar S, Rantal F, Tamas T, Toth G, Zagyva A, Zekany A, Lavian G, Gross A, Friedman R, Razin M, Huang W, Krais B, Chorev M, Youdim MB, Weinstock M (2002) Novel dual inhibitors of AChE and MAO derived from hydroxy aminoindan and phenethylamine as potential treatment for Alzheimer’s disease. J Med Chem 45:5260–5279
Su H (2011) Design and synthesis of dual-target-directed ligands as potential treatment for Alzheimer’s disease. M.S. Thesis, Hefei University of Technology
Takashima A (2006) GSK-3β is essential in the pathogenesis of Alzheimer’s disease. J Alzheimer Dis 9:309–317
Tang H, Zhao LZ, Zhao HT, Huang SL, Zhong SM, Qin JK, Chen ZF, Huang ZS, Liang H (2011) Hybrids of oxoisoaporphine-tacrine congener: novel acetylcholinesterase and acetylcholinesterase-induced β-amyloid aggregation inhibitors. Eur J Med Chem 46:4970–4979
Taniguchi S, Suzuki N, Masuda M, Hisanaga S, Iwatsubo T, Goedert M, Hasegawa M (2005) Inhibition of heparin-induced tau filament formation by phenothiazine, polyphenols, and porphyrins. J Biol Chem 280:7614–7623
Tumiatti V, Milelli A, Minarini A, Rosini M, Bolognesi ML, Micco M, Andeisano V, Bartolini M, Mancini F, Recanatini M, Cavalli A, Melchiorre C (2008) Structure-activity relationships of acetylcholinesterase noncovalent inhibitors based on a polyamine backbone 4. Further investigation on the inner spacer. J Med Chem 51:7308–7312
Yan Y, Liu Y, Sorci M, Belfort G, Lusthader JW, Yan SS, Wang C (2007) Surface Plasmon resonance and unclear magnetic resonance studies of ABAD-A beta interaction. Biochemistry 46:1724–1731
Zhu YP, Xiao K, Ma LP, Xiong B, Fu Y, Yu HP, Wang W, Wang X, Hu DY, Heng HL, Li JY, Gong Q, Chai Q, Tang XC, Zhang HY, Li J, Shen JK (2009) Design, synthesis and biological evaluation of novel dual inhibitors of acetylcholinesterase and β-secretase. Bioorg Med Chem 17:1600–1613
Acknowledgments
This research was financially supported by the Anhui Province Science and Technology Project (No. 1101041025) and Hefei University of Technology Major Pre-research Special Project (No. 2010HGZY0011).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hui, Al., Chen, Y., Zhu, Sj. et al. Design and synthesis of tacrine-phenothiazine hybrids as multitarget drugs for Alzheimer’s disease. Med Chem Res 23, 3546–3557 (2014). https://doi.org/10.1007/s00044-014-0931-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-014-0931-2