Abstract
Objective and design
The serial or dynamic changes of cytokine levels in severely septic patients, between shock and no shock, survivors and non-survivors are still unclear.
Methods
Seventy-six patients with severe sepsis were enrolled to our study. Plasma levels of interferon-γ, interleukin (IL)-6, IL-10, IL-12 and transforming growth factor-β1 from day 1 to day 7 were determined.
Results
IL-6 level in non-survivors was higher than that in survivors on day 1. IL-10 level in non-survivors was higher than that in survivors on day 1, 2, and 3. IL-6 level in shock patients was higher than that in non-shock patients on day 1, 2, 6 and 7. IL-10 level in shock patients was higher than that in non-shock patients from day 1 to day 7. Plasma time-course curves of IL-6 and IL-10 were different between survivors and non-survivors. Plasma time-course curve of IL-6 was different between patients with shock and without shock. Regression analysis found that IL-6 was correlated with IL-10 and shock. IL-10 was correlated with IL-6 and mortality.
Conclusion
IL-6 and IL-10 were the key cytokines in the pathogenesis of severe sepsis. IL-6 was comparatively more associated with septic shock and IL-10 was comparatively more associated with mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe sepsis is predominantly a problem in intensive care units (ICUs). Sepsis is a complicated syndrome in which pro-inflammatory and anti-inflammatory cytokines are expressed simultaneously [1]. Pro-inflammatory cytokines is regulated by anti-inflammatory cytokines. Early inflammatory response in sepsis is characterized by the release of a number of pro-inflammatory cytokines, including interferon (IFN)-γ, interleukin (IL)-6 and IL-12. Leptin and IL-6 were reported to be independent predictors of death [2]. Injection of IL-6 before lipopolysaccharide (LPS) protected against fatal outcome in mice [3]. In the PROWESS (Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis) study, the plasma IL-6 level in placebo-treated patients who had survived was significantly lower than that in those not survived [4]. These findings suggest that IL-6 is a key cytokine during sepsis. IFN-γ enhances macrophage function and plays an important role in the pathogenesis of sepsis. IFN-γ has antiviral activity, augments tumor necrosis factor (TNF) activity, and induces nitric oxide [5]. Further, animal model has identified elevated circulating IFN-γ levels in sepsis [6, 7]. Antigen-presenting cells, including monocytes and macrophages, dendritic cells and neutrophils, are the primary source of IL-12. IL-12 induces proliferation, IFN-γ production and increase cytotoxic activity of T and natural killer cells. Importantly, IL-12 induces the polarization of CD4+ T cells to the T helper 1 (Th1) phenotype that mediates immunity against intracellular pathogens [8]. Therapy to augment the production of Th1 cytokines by IL-12 might be beneficial in the treatment of experimental mice with severe sepsis after peritonitis [9].
The latter inflammatory response in sepsis has been referred to as compensatory anti-inflammatory response syndrome, including release of IL-10 and transforming growth factor-beta (TGF-β). In a murine model, the septic response substantially impaired lung immunity to Pseudomonas aeruginosa, and this effect was mediated primarily by endogenously produced IL-10 [10]. In a model of acute endotoxic shock, it was found that the lethal dose of LPS for IL-10-deficient mice was 20-fold lower than that for wild type mice [11]. It appears that depending on the experimental model, IL-10 may be beneficial or deleterious. Plasma TGF-β values were reported to be unable to provide any prognostic information [12, 13]. The level of TGF-β was higher in malaria children with severe disease than in those with mild disease [14]. The role of TGF-β in severe sepsis is still unclear.
Up to now, most studies only measured the cytokine levels for septic patients upon the admission, a follow-up study was either none or limited [15–17]. A study of Fernandez-Serrano ever showed the time course profiles of TNF-α, IL-6, IL-8 and IL-10 in patients with severe community-acquired pneumonia [18]. However, the patient number of Fernandez-Serrano’s work is small (N = 38). Thus, we designed a prospective study with a larger case number to examine the sequential plasma levels of IFN-γ, IL-6, IL-10, IL-12 and TGF-β1 from day 1 to day 7 in patients with severe sepsis. The purpose is to analyze the relationship between these cytokines and the outcome of severe sepsis.
Materials and methods
Subjects
From October 2003 to September 2005, 76 patients who were admitted to emergency department and soon transferred to ICU at Chang Gung Memorial Hospital due to severe sepsis were enrolled to this study with informed consent provided by their families. The ICU is a medical and closed unit in our hospital. This study was approved by Institutional Review Board at Chang Gung Memorial Hospital (IRB/CGMH). The following patient’s data was recorded within the first 3 days after admission: age, gender, medical history, infection source, Acute Physiology and Chronic Health Evaluation (APACHE) II score, and co-morbidity. Standard treatment, including fluid resuscitation, broad-spectrum antibiotics, drainage and basic support, were provided to all patients. Antibiotics and fluid resuscitation were started as soon as possible after the sepsis was diagnosed [19]. Pneumonia was diagnosed based on abnormal infiltration shown on the chest radiography. Urinary tract infection was diagnosed based on the presence of pyuria and positive bacteria culture. Acute renal failure was diagnosed as a rapidly rising serum creatine level ≥0.5 mg/dl over the base-line value [20].
Severe sepsis and septic shock were defined according to the criteria made in the Consensus Conference [21]. Systemic inflammatory response syndrome (SIRS) was defined as two or more of the following criteria: (1) body temperature >38°C or <36°C; (2) respiratory rate >24 breaths/min; (3) heart rate >90 beats/min; and, (4) white blood count >12,000/μl or <4,000/μl or >10% bands. Sepsis was defined as SIRS according to a confirmed or suspected microbial etiology. Severe sepsis was defined as sepsis with one or more of organ dysfunction or hypotension. Septic shock was defined as sepsis with hypotension unresponsive to fluid resuscitation, which further requires vasopressors to maintain blood pressure on the emergency department admission day. Disease severity was assessed with the APACHE II score [22]. The survivors were defined as patients, who were alive 28 days after hospital admission.
Cytokine measurement
Patient’s plasma samples in day 1 were obtained as soon as their arrival at admission to emergency department. Their plasma samples from day 2 to day 7 were obtained at 12:30 A.M. For the reference data, plasma samples of eight healthy men and one healthy woman were obtained at 08:30 A.M. All plasma samples were stored at –80°C until use. Plasma levels of IFN-γ, IL-6, IL-10, IL-12 and TGF-β1 were measured by human IFN-γ, IL-6, IL-10 and IL-12 enzyme-linked immunosorbent assay (ELISA) kits (Pierce Biotechnology, Illinois, USA) and TGF-β1 ELISA kit (R&D Systems, Minnesota, USA) according to the manufacturer’s instructions. Measurement data were average of two readings.
Statistical analysis
Statistical analysis was performed with Statistical Package for the Social Sciences (SPSS) V11.0.1 for Windows (SPSS Inc., Illinois, USA). Differences for age and APACHE II score between survivors and non-survivors, and the presence and absence of septic shock at initial presentation were analyzed by Mann–Whitney test. Differences for cytokine level among healthy controls, survivors and non-survivors, and the presence and absence of septic shock at initial presentation were analyzed by Kruskal–Wallis test with post hoc comparisons by Mann–Whitney test. Difference for categorical variables between survivors and non-survivors were compared by the Chi-square test or Fisher’s exact test. The differences of sequential data of cytokines between survivors and non-survivors, and the presence and absence of septic shock at initial presentation are compared by repeated measure analysis of variance. Lineal enter regression models were analyzed to determine the independent factors associated with IL-6 and IL-10 levels. Cytokine level and APACHE II score on day 1, mortality, shock and gastrointestinal bleeding were served as cofactors. A P value of <0.05 was considered statistically significant.
Results
Seventy-six patients were enrolled to this study. The demographic data was shown in Table 1. The mean of APACHE II score in non-survivors was significantly higher than that in survivors. There were no significant differences in history and infection source between survivor and non-survivor. The incidences for septic shock and gastrointestinal bleeding in non-survivors were significantly higher than that in survivors. Six patients died on day 2. Four patients died on day 3. Only 9 non-survivors were alive till day 7.
Comparison of cytokine level among subjects
Interferon-γ level in non-survivors was significantly higher than that in survivors from day 5 to day 6 (Table 2). There was no difference in IFN-γ level from day 1 to day 7 between patients with shock and without shock at initial presentation. IL-6 level in non-survivors was significantly higher than that in survivors on day 1 (Table 3). IL-6 level in patients with shock was significantly higher than that in patients without shock at initial presentation on day 1, 2, 6, and 7. Serial IL-6 levels from day 1 to day 7 in patients with severe sepsis were significantly higher than that in healthy controls. IL-10 level in non-survivors was significantly higher than that in survivors on day 1, 2, and 3 (Table 4). IL-10 level in patients with shock was significantly higher than that in patients without shock from day 1 to day 7. IL-10 level in survivors was significantly higher than that in controls on day 1. IL-10 level in non-survivors was significantly higher than that in controls on day 1, 2, and 3. IL-10 level in patients with shock at initial presentation was significantly higher than that in controls on day 1 and 2.
Interleukin-12 level in non-survivors was not significantly higher than that in survivors from day 1 to day 7 (Table 5). There was no difference in IL-12 level from day 1 to day 7 between patients with shock and without shock at initial presentation. IL-12 level in survivors was significantly lower than that in controls. IL-12 level between healthy controls and non-survivors was similar. TGF-β1 level in non-survivors was significantly higher than that in survivors on day 1, day 2, and day 5 (Table 6). TGF-β1 level in survivors was significantly lower than that in healthy controls on day 1, day 2, and day 4. TGF-β1 level in patients without shock at initial presentation was significantly lower than that in healthy controls on day 1 and day 2. TGF-β1 level in non-survivors or patients with shock at initial presentation was similar to that in healthy controls from day 1 to day 7.
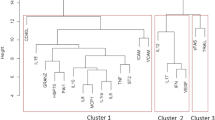
Comparison of serial cytokine level between patients
Serial plasma IL-6 levels from day 1 to day 7 were different between survivors and non-survivors (P = 0.012). Also, serial plasma IL-10 levels from day 1 to day 7 were different between survivors and non-survivors (P = 0.048). Serial plasma IL-6 and IL-10 levels in non-survivors were significantly higher than that in survivors. There were no differences in serial plasma IFN-γ, IL-12, and TGF-β1 levels from day 1 to day 7 between survivors and non-survivors. Serial plasma IL-6 levels from day 1 to day 7 were different between patients with shock and without shock at initial presentation (P = 0.003). Serial plasma IL-6 levels in patients with shock at initial presentation were significantly higher than that without shock at initial presentation. There were no differences in serial plasma IFN-γ, IL-10, IL-12, and TGF-β1 levels from day 1 to day 7 betweens patients with shock and without shock at initial presentation.
Association of IL-6 and IL-10 with clinical characteristics
After regression analysis, IL-10 level on day 1 and presence of septic shock were shown to be independent factors associated with IL-6 level on day 1 (Table 7). Patient’s mortality was not independent factor associated with IL-6 level on day 1. IL-6 level on day 1 and patient’s mortality were independent factors associated with IL-10 level on day 1 (Table 8). The presence of septic shock was not independent factor associated with IL-10 level on day 1.
Discussion
The immune system plays a crucial role in the pathogenesis of sepsis. Innate immune system such as macrophages, natural killer cells and neutrophils with aid of T cells, B cells and cytokines is important in eradicating pathogens. During the treatment, these cytokines showed different changes between survivors and non-survivors, and the presence and absence of septic shock.
This work confirmed that IL-6 was an important cytokine in the pathogenesis of severe sepsis, as reflected by the different time-course curves between survivors and non-survivors, and the presence and absence of septic shock. The time-course curve for IL-6 in non-survivors and patients with septic shock showed a declining pattern at the beginning, however, which had became an ascending slope since day 6. This suggested that a dynamic increase in plasma IL-6 level was associated with poor outcome and more severe disease. Previous report showed that the IL-6 gene polymorphism in −174 G/C promoter area was associated with shock in patients with sepsis [23]. In patients with septic shock, the frequency of mutated C-allele in the IL-6 promoter was significantly higher than that in individuals without shock. A large cohort study (n = 228) found no association of −174 G or C alleles with 28-day mortality in critically ill SIRS patients [24]. However, the single-nucleotide polymorphism in IL-6 promoter region was functional in vivo, which showed an increased IL-6 response with G allele [25]. Due to the conflict reports, the influence of −174 G/C polymorphism in IL-6 promoter is still unclear. The plasma IL-6 level may have more contribution to the outcome of severe sepsis than the polymorphism does.
Plasma IL-10 levels of non-survivors and patients with septic shock on the first 3 days were significantly higher than that of survivors and patients without septic shock. Most of IL-10 is released from monocytes, macrophages and T cells. IL-10 inhibits cell immunity and Th1 differentiation, but enhances B cell and mast cell function. The plasma IL-10 level in septic patients may indicate the relative anti-inflammatory status. Our work supports the hypothesis that over production of IL-10 may result in failure of immune system, leading to disease progression in patients with severe sepsis. This hypothesis can also be supported by two reports, which showed that anti-inflammatory strategies might worsen the outcomes [26, 27]. Also, the IL-10 promoter polymorphism at −1082A/G might be associated with the pathogenesis of sepsis. The AA homozygous genotype was found more frequently in patients with sepsis compared with controls. The G allele was associated with higher IL-10 production and mortality in patients with severe sepsis [28]. In another study, either the genotype frequency between septic patients and controls or the mortality between survivors and non-survivors, none of them showed IL-10−1082A or G genotypes-related differences [29]. As the same conclusion as the IL-6 polymorphism, the plasma IL-10 level might be more important in determining the consequence of sepsis.
The source of IFN-γ is activated CD8+ T lymphocytes, Th1 lymphocytes and natural killer cells. Antigen-presenting cells secret IL-12 after pathogen stimulation. In this work, non-survivors with severe sepsis generally had relatively higher plasma IFN-γ and IL-12 in the first 7 days after admission compared with survivors. Persistent higher plasma IFN-γ and IL-12 might represent persistent infection and no eradication of pathogens. Our findings support the hypothesis that persistent infection and prolonged poor immune response resulted in death for septic patients [1].
Sepsis can induce host immunosuppression and lymphocyte apoptosis [30, 31]. TGF-β1 is thought as an anti-inflammatory cytokine with potent immunoregulatory property. TGF-β1 suppresses IL-1β and TNF-α production from monocytes. Moreover, TGF-β1 down regulates macrophage and granulocyte responses. However, recent animal experiments demonstrated that naïve CD4+ T cells can develop into T helper 17 (Th17) cells with presence of IL-6 and TGF-β1, and regulatory T (T reg) cells with presence of TGF-β1 [32]. T reg cells that modify and suppress the immune responses to pathogenic organisms counteract Th17 cells, which induce inflammation [33, 34]. Thus, the role of TGF-β1 is complex in the pathogenesis of sepsis. Septic non-survivors had sustained TGF-β1 and declined IL-6 during the 7-days study. Also, T reg percentage of CD4+ cells in non-survivors of septic shock after 7 days was significantly higher than that in survivors [35]. These findings suggest that CD4+ cells have skewed towards T reg cells formation and immune suppression in septic non-survivors despite of the treatments. Emerging data regarding the roles of Th17 and T reg cells suggest an important function for T cell subset in immunity and disease. However, no human study investigates the role of Th17 in patients with severe sepsis. Increased percentage of T reg cells in patients with septic shock was due to the loss of non-Treg CD4+ T cells [36]. Although there are abundant animal-model-related articles investigating T reg in infection, the human-model studies are few. More works are needed to determine the role and interaction among the four T help cell subsets (Th1, Th2, Th17 and T reg).
The results of this work were of the same to many studies reporting that IL-6 and IL-10 levels in patients with severe sepsis were different between survivor and non-survivor [13, 37–39]. However, this work was the first to show that rather than mortality, IL-6 level was more related with septic shock. Compared with septic shock, IL-10 level was more related with mortality. More studies are needed to confirm these two observations.
There are two limitations in this work. First, the time of blood sampling may be a factor influencing cytokine levels especially after fluid resuscitation. Because this was an observing study under the standard treatment, investigators could not delay the essential resuscitation just for blood sampling. All patients received fluid replacement before blood sampling on day 1. Compared with healthy controls, fluid resuscitation might also lower IL-12 and TGF-β1 levels in certain patient sub-groups. Second, the treatment of severe sepsis might not be adequate and equal. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock were first brought up in 2004 March [40]. The treatment protocol of severe sepsis in our ICU had been set up with consensus since 2006. These two limitations might influence the results to a certain degree.
In conclusion, we successfully demonstrated and confirmed that IL-6 and IL-10 were two important cytokines in severe sepsis by a time-course model. From the results of regression analysis, IL-6 was relatively more associated with septic shock and IL-10 was relatively more associated with mortality.
References
Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. 2003;348:138–50.
Arnalich F, Lopez J, Codoceo R, Jim NM, Madero R, Montiel C. Relationship of plasma leptin to plasma cytokines and human survivalin sepsis and septic shock. J Infect Dis. 1999;180:908–11.
Yoshizawa K, Naruto M, Ida N. Injection time of interleukin-6 determines fatal outcome in experimental endotoxin shock. J Interferon Cytokine Res. 1996;16:995–1000.
Kinasewitz GT, Yan SB, Basson B, Comp P, Russell JA, Cariou A, et al. Universal changes in biomarkers of coagulation and inflammation occur in patients with severe sepsis, regardless of causative micro-organism [ISRCTN74215569]. Crit Care. 2004;8:R82–90.
Dinarello CA. Proinflammatory cytokines. Chest. 2000;118:503–8.
Maina N, Ngotho JM, Were T, Thuita JK, Mwangangi DM, Kagira JM, et al. Proinflammatory cytokine expression in the early phase of Trypanosoma brucei rhodesiense infection in vervet monkeys (Cercopithecus aethiops). Infect Immun. 2004;72:3063–5.
Rubins JB, Pomeroy C. Role of gamma interferon in the pathogenesis of bacteremic pneumococcal pneumonia. Infect Immun. 1997;65:2975–7.
Watford WT, Moriguchi M, Morinobu A, O’Shea JJ. The biology of IL-12: coordinating innate and adaptive immune responses. Cytokine Growth Factor Rev. 2003;14:361–8.
Ono S, Ueno C, Aosasa S, Tsujimoto H, Seki S, Mochizuki H. Severe sepsis induces deficient interferon-gamma and interleukin-12 production, but interleukin-12 therapy improves survival in peritonitis. Am J Surg. 2001;182:491–7.
Steinhauser ML, Hogaboam CM, Kunkel SL, Lukacs NW, Strieter RM, Standiford TJ. IL-10 is a major mediator of sepsis-induced impairment in lung antibacterial host defense. J Immunol. 1999;162:392–9.
Berg DJ, Kuhn R, Rajewsky K, Muller W, Menon S, Davidson N, et al. Interleukin-10 is a central regulator of the response to LPS in murine models of endotoxic shock and the Shwartzman reaction but not endotoxin tolerance. J Clin Invest. 1995;96:2339–47.
Sablotzki A, Dehne MG, Friedrich I, Grond S, Zickmann B, Muhling J, et al. Different expression of cytokines in survivors and non-survivors from MODS following cardiovascular surgery. Eur J Med Res. 2003;8:71–6.
Monneret G, Finck ME, Venet F, Debard AL, Bohe J, Bienvenu J, et al. The anti-inflammatory response dominates after septic shock: association of low monocyte HLA-DR expression and high interleukin-10 concentration. Immunol Lett. 2004;95:193–8.
Malaguarnera L, Pignatelli S, Simpore J, Malaguarnera M, Musumeci S. Plasma levels of interleukin-12 (IL-12), interleukin-18 (IL-18) and transforming growth factor beta (TGF-beta) in Plasmodium falciparum malaria. Eur Cytokine Netw. 2002;13:425–30.
Lekkou A, Karakantza M, Mouzaki A, Kalfarentzos F, Gogos CA. Cytokine production and monocyte HLA-DR expression as predictors of outcome for patients with community-acquired severe infections. Clin Diagn Lab Immunol. 2004;11:161–7.
Carrol ED, Thomson AP, Jones AP, Jeffers G, Hart CA. A predominantly anti-inflammatory cytokine profile is associated with disease severity in meningococcal sepsis. Intensive Care Med. 2005;31:1415–9.
Groeneveld PH, Kwappenberg KM, Langermans JA, Nibbering PH, Curtis L. Relation between pro- and anti-inflammatory cytokines and the production of nitric oxide (NO) in severe sepsis. Cytokine. 1997;9:138–42.
Fernandez-Serrano S, Dorca J, Coromines M, Carratala J, Gudiol F, Manresa F. Molecular inflammatory responses measured in blood of patients with severe community-acquired pneumonia. Clin Diagn Lab Immunol. 2003;10:813–20.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–12.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med. 2003;31:1250–6.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29.
Tischendorf JJ, Yagmur E, Scholten D, Vidacek D, Koch A, Winograd R, et al. The interleukin-6 (IL6)−174 G/C promoter genotype is associated with the presence of septic shock and the ex vivo secretion of IL6. Int J Immunogenet. 2007;34:413–8.
Sutherland AM, Walley KR, Manocha S, Russell JA. The association of interleukin 6 haplotype clades with mortality in critically ill adults. Arch Intern Med. 2005;165:75–82.
Bennermo M, Held C, Stemme S, Ericsson CG, Silveira A, Green F, et al. Genetic predisposition of the interleukin-6 response to inflammation: implications for a variety of major diseases? Clin Chem. 2004;50:2136–40.
Fisher CJ Jr, Agosti JM, Opal SM, Lowry SF, Balk RA, Sadoff JC, et al. Treatment of septic shock with the tumor necrosis factor receptor: Fc fusion protein. The soluble TNF Receptor Sepsis Study Group. N Engl J Med. 1996;334:1697–702.
Oberholzer A, Oberholzer C, Moldawer LL. Sepsis syndromes: understanding the role of innate and acquired immunity. Shock. 2001;16:83–96.
Stanilova SA, Miteva LD, Karakolev ZT, Stefanov CS. Interleukin-10-1082 promoter polymorphism in association with cytokine production and sepsis susceptibility. Intensive Care Med. 2006;32:260–6.
Garnacho-Montero J, Bo-Pallas T, Garnacho-Montero C, Cayuela A, Jimenez R, Barroso S, et al. Timing of adequate antibiotic therapy is a greater determinant of outcome than are TNF and IL-10 polymorphisms in patients with sepsis. Crit Care. 2006;10:R111.
Russell JA. Management of sepsis. N Engl J Med. 2006;355:1699–713.
Hotchkiss RS, Tinsley KW, Swanson PE, Schmieg RE Jr, Hui JJ, Chang KC, et al. Sepsis-induced apoptosis causes progressive profound depletion of B and CD4+ T lymphocytes in humans. J Immunol. 2001;166:6952–63.
Afzali B, Lombardi G, Lechler RI, Lord GM. The role of T helper 17 (Th17) and regulatory T cells (Treg) in human organ transplantation and autoimmune disease. Clin Exp Immunol. 2007;148:32–46.
Bettelli E, Oukka M, Kuchroo VK. T(H)-17 cells in the circle of immunity and autoimmunity. Nat Immunol. 2007;8:345–50.
Rudge G, Gleeson PA, van DI. Control of immune responses by immunoregulatory T cells. Arch Immunol Ther Exp (Warsz). 2006;54:381–91.
Monneret G, Debard AL, Venet F, Bohe J, Hequet O, Bienvenu J, et al. Marked elevation of human circulating CD4+ CD25+ regulatory T cells in sepsis-induced immunoparalysis. Crit Care Med. 2003;31:2068–71.
Venet F, Pachot A, Debard AL, Bohe J, Bienvenu J, Lepape A, et al. Increased percentage of CD4+ CD25+ regulatory T cells during septic shock is due to the decrease of CD4+. Crit Care Med. 2004;32:2329–31.
Bozza FA, Salluh JI, Japiassu AM, Soares M, Assis EF, Gomes RN, et al. Cytokine profiles as markers of disease severity in sepsis: a multiplex analysis. Crit Care. 2007;11:R49.
Oberholzer A, Souza SM, Tschoeke SK, Oberholzer C, Abouhamze A, Pribble JP, et al. Plasma cytokine measurements augment prognostic scores as indicators of outcome in patients with severe sepsis. Shock. 2005;23:488–93.
Rodriguez-Gaspar M, Santolaria F, Jarque-Lopez A, Gonzalez-Reimers E, Milena A, de l, V et al. Prognostic value of cytokines in SIRS general medical patients. Cytokine 2001;15:232–6.
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32:858–73.
Acknowledgments
The authors thank all members of medical and emergent intensive care units for providing clinical assistance. This research was supported by Chang Gung Memorial Hospital under Contract #CMRPG240331.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: C. Kasserra.
Rights and permissions
About this article
Cite this article
Wu, HP., Chen, CK., Chung, K. et al. Serial cytokine levels in patients with severe sepsis. Inflamm. Res. 58, 385–393 (2009). https://doi.org/10.1007/s00011-009-0003-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-009-0003-0