Abstract
Objective
This study aimed to determine whether an anti-inflammatory profile in meningococcal disease is associated with an increased risk of severe disease or septic shock.
Design and setting
Prospective observational study in a tertiary care children’s hospital.
Patients and participants
63 children with confirmed meningococcal disease.
Interventions
Plasma concentrations of interleukin-1 receptor antagonist (IL-1Ra), interleukin-6 (IL-6), interleukin-8 (IL-8) and tumour necrosis factor-α (TNF) were assayed on admission. Receiver operator characteristic curve analysis was used to determine optimum thresholds for IL-1Ra:TNF, IL-1Ra:IL-6 and IL-1Ra:IL-8 ratios.
Measurements and results
Median IL-1Ra:TNF and IL-1Ra:IL-6 ratios were significantly higher in severe disease with septic shock than in severe disease without septic shock and in non severe disease (IL-1Ra:TNF 263 vs. 185 vs. 108; IL-1Ra:IL-6 139 vs. 23 vs. 17). Median IL-1Ra:IL-8 ratios were not significantly different in the three groups. A significantly larger proportion of children with high IL-1Ra:TNF-α and IL-1Ra:IL-6 ratios developed severe disease with septic shock than those with a low ratios (95.2% vs. 4.8%; 76.2% vs. 23.8%).
Conclusions
An anti-inflammatory profile appears to be associated with the development of severe disease and septic shock in meningococcal sepsis. This may imply that experimental new therapies of pro-inflammatory cytokine inhibition and anti-inflammatory cytokines in meningococcal disease could be detrimental.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In meningococcal sepsis the inflammatory cascade is activated on release of endotoxin (lipopolysaccharide, LPS), resulting in the release of cytokines. These cytokines are produced principally by monocytes, macrophages and endothelial cells. The pro-inflammatory cytokines tumour necrosis factor-α (TNF), interleukin (IL) 1β, IL-6 and IL-8 increase rapidly, and their levels are correlated with severity of disease [1]. This is rapidly followed by a peak of anti-inflammatory cytokines IL-1 receptor antagonist (IL-1Ra), IL-10 and soluble TNF receptors (sTNFr) [2, 3].
Van Deuren et al. [4] have demonstrated in vitro suppression of LPS-stimulated pro-inflammatory cytokine (TNF, IL-1β, and IL-6) production during the acute stage of meningococcal infection, with production being restored during convalescence. Conversely, LPS-stimulated IL-1Ra production was maximal during the acute stage, and stabilised after 2 days. They concluded that this indicates a protective regulatory mechanism.In a study of 464 febrile adults with community acquired infection van Dissel et al. [5] demonstrated that the ratio of IL-10 to TNF-α was significantly higher in non-survivors than in survivors. The ratio was highest in patients who died without underlying disease. The authors state that an anti-inflammatory profile is an innate host characteristic that may contribute to fatal meningococcal disease, and caution against the use of pro-inflammatory cytokine inhibition therapy in patients with sepsis. In a study of 65 patients with severe sepsis elevated serum IL-10 and TNF-α and a high IL-10 to TNF-α ratio were associated with death. They conclude the sustained overproduction of the anti-inflammatory cytokine IL-10 is the main predictor of severity and fatal outcome [6].
There is a wealth of data in the literature on the correlation of serum and plasma levels of various cytokines and disease severity, but it seems that it is the balance between pro- and anti-inflammatory cytokines that determines the severity of infection. Several recent studies have investigated the ratio of pro- to anti-inflammatory cytokines in various disease states, as opposed to absolute levels per se [6, 7, 8, 9]. The aim of this study was to determine whether a predominantly anti-inflammatory cytokine profile is associated with more severe disease (and thus septic shock and death) in children with meningococcal disease.
Methods and materials
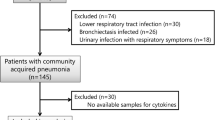
A prospective observational study was carried out between December 1997 and March 1999 on children admitted to Royal Liverpool Children’s Hospital (Alder Hey) between the ages of 3 months and 16 years. This is a large tertiary children’s hospital that provides primary and secondary care in addition. All children with a suspected diagnosis of meningoccoccal disease were recruited (n=165), but only the 63 with confirmed disease and a complete set of results of final IL-1Ra determinations after dilution were included in this study (median age 3.3 years, range 0.1–15.9; 36 boys, 27 girls). Ethical approval for this study was obtained from the local research ethics committee, and written informed consent was obtained from parents before children were recruited into the study. Children were included if they presented with a petechial or purpuric rash and features of sepsis or signs of meningitis or both, and if the diagnosis was confirmed microbiologically by culture, antigen testing or PCR. Clinical and laboratory data were recorded throughout their hospital admission. Severity of disease was assessed using the Glasgow Meningococcal Septicaemia Prognostic Score (GMSPS) [10]. Severe disease was defined as a GMSPS of 8 or higher. Septic shock was defined as confirmed infection with clinical signs of decreased perfusion despite adequate volume replacement, and one or more signs of impaired perfusion (lactate >2 mmol/l, capillary refill greater than 2 s, base deficit >−5, decreased mental status or decreased urine output) [11, 12]. Severe disease without septic shock refers to children with a GMSPS of 8 or higher but who did not have signs of septic shock. In addition, children were classified according to three disease types; meningitis alone, septicaemia alone, and mixed meningitis and septicaemia. A total of 36 (57%) children had severe disease, 21 (33%) children had septic shock and 6 (9%), children died. Clinical and laboratory variables in children with non-severe disease, severe disease without septic shock, and severe disease with septic shock are shown in Table 1.
Plasma concentrations of IL-1Ra, IL-6 and TNF-α, IL-8 and RANTES (regulated on activation normal T cell expressed and secreted) were determined on admission using an Enzyme Amplified Sensitivity Immunoassay (Medgenix, Biosource, Fleurus, Belgium). All samples were taken within 4 h of admission and first dose of antibiotic and were centrifuged and stored at −80°C until assayed. If cytokine concentrations were above the upper limit of the standard curve of the assay, additional dilutions were not performed for TNF, IL-8 and IL-6. Additional dilutions were performed for IL-1Ra because most of the values measured were above the upper limit of detection of the assay. The limited volume of plasma that was available on these critically ill children meant that there was insufficient plasma remaining to do additional dilutions on only 63 patients. Only one set of cytokine measurements were performed on each child, at admission. Full blood count and lactate were also measured on admission. No children received corticosteroid therapy prior to sampling.
Statistical analysis was performed using SPSS version 12.0 (Chicago, Ill., USA). Statistical differences were assessed using the Mann-Whitney test for independent groups where appropriate and correlations with Spearman’s correlation coefficient. The χ2 test was used to test the significance of associations, with Fisher’s exact test where necessary. Logistic regression analysis was used to determine odds ratios. Receiver operating characteristic (ROC) analysis to determine a cut-off point for optimum sensitivity and specificity for IL-1Ra:IL-6, IL-1Ra:TNF and IL-1Ra:IL-8 ratios was performed with StatsDirect (Cheshire, UK) software. Univariate analysis was performed to determine the influence of IL-1Ra:IL-6, IL-1Ra:TNF and IL-1Ra:IL-8 ratios on disease severity and septic shock as an outcome.
Results
IL-1Ra concentrations ranged from 302 to greater than 400,000 pg/ml (median 34,098), TNF concentrations from 16 to greater than 1520 pg/ml (median 124), IL-6 concentrations from 50 to greater than 1700 pg/ml (median 1475) and IL-8 concentrations from 10 to greater than 750 pg/ml (median 73). Median IL-Ra:TNF and IL-1Ra:IL-6 ratios were significantly higher in those with severe disease with septic shock vs. severe disease without septic shock vs. non-severe disease (Table 2). Median IL-1Ra:IL-8 ratios were not significantly different in the three groups. All three ratios were higher in non-survivors than survivors, but this difference was not significant. There was no significant difference in ratios between disease types; meningitis alone (n=2, 3.2%), septicaemia alone (n=20, 31.7%) and mixed meningitis/septicaemia (n=41, 65.1%), but this might be due to the small numbers in each group.
Using ROC analysis the cut-off points for optimum sensitivity and specificity for the ratios were as follows; IL-1Ra:TNF 109.77 for severe disease (sensitivity 83%, specificity 52%), and 109.77 for septic shock (sensitivity 95%, specificity 45%); IL-1Ra:IL-6:38.58 for severe disease (sensitivity 64%, specificity 93%) and 51.32 for septic shock (sensitivity 77%, specificity 88%); IL-1Ra:IL-8:211.45 for severe disease (sensitivity 78%, specificity 48%) and 219.6 for septic shock (sensitivity 86%, specificity 45%). Cut-off values higher than 110 for IL-1Ra:TNF ratio, higher than 50 for IL-1Ra:IL-6 ratio and higher than 220 for IL-1Ra:IL-8 ratio were therefore used to define a high ratio in each case.
A significantly higher proportion of children with high IL-1Ra:TNF and a high IL-1Ra:IL-6 ratios developed severe disease with septic shock than those with a low ratio (Table 3). A high IL-1Ra:IL-6 ratio was significantly associated with severe disease with septic shock, compared to severe disease without septic shock. There was no statistically significant difference in IL-1Ra:TNF, IL-1Ra:IL-6 and IL-1Ra:IL-8 ratios between survivors and non-survivors. On univariate analysis a high IL-1Ra:TNF ratio (odds ratio 16.4, 95% confidence interval 2.0–134.0), a high IL-1Ra:IL-6 ratio (20.4, 5.4–76.3) and a high IL-1Ra:IL-8 ratio (5.0, 1.3–19.4) were significantly associated with septic shock.
Discussion
We conclude from these findings study that an anti-inflammatory profile with high IL-1Ra:TNF, high IL-1Ra:IL-6 and high IL-1Ra:IL-8 ratios is associated with more severe disease and septic shock. This anti-inflammatory profile was also associated with a higher risk of death, but as the number of non-survivors was small, this difference was not statistically significant.
The finding of elevated pro- and anti-inflammatory cytokines in meningococcal disease demonstrated in this study confirm those previously published [1, 2, 13]. Unfortunately, due to limited plasma volumes available, we were unable to measure IL-10, which has previously been shown to be an important mediator. The association of an anti-inflammatory profile with an unfavourable outcome has previously been described in febrile adults with community acquired infections [5]. An anti-inflammatory phenotype is recognised as a hallmark of the “immune paralysis” described in patients with severe sepsis and septic shock [14, 15] and more recently a lower basal TNF-α/IL-10 ratio has been demonstrated in patients with septic shock [16]. Our results are consistent with this.
We have previously shown lower concentrations of RANTES in children with more severe disease or septic shock and in non-survivors [17], and this has recently been confirmed by Moller et al. [18] who demonstrated significantly higher monocyte chemotactic peptide 1, macrophage inflammatory protein 1α and IL-8 and lower RANTES in fulminant meningococcal septicaemia. A recent study demonstrated IL-6 to be a major mediator of myocardial dysfunction in meningococcal septic shock [19], and it is interesting that in this study the IL-1Ra:IL-6 ratio was the most significant discriminator in the three disease groups (non-severe disease, severe disease without septic shock, severe disease with septic shock).
A complex interplay of mediators are responsible for determining severity of disease, and this study has limitations in trying to assess the state of the combined pro- and anti-inflammatory responses on a single sample in response to an ongoing systemic insult. A parameter such as HLA-DR expression might be a better guide, but we were unable to determine this in the present study.
Trials of anti-TNF therapy and IL-1Ra therapy in sepsis have failed to show significant benefit. It is likely that cytokine regulatory mechanisms are far more complex than we realise, and that a multi-directional approach administered early, as opposed to a single immunomodulatory strategy, is necessary. The results from our study suggest that pro-inflammatory cytokine inhibition is detrimental in severe meningococcal sepsis. More importantly, however, it is in patients with high IL-1Ra:TNF, IL-1Ra:IL-6 and IL-1Ra:IL-8 ratios that one needs to be more vigilant because of their increased likelihood of an unfavourable outcome. Perhaps it is to these patients that new therapies need to be targeted, and more aggressive management strategies directed.
References
Deuren M van, van der Ven-Jongekrijg J, Bartelink AK, van Dalen R, Sauerwein RW, van der Meer JW (1995) Correlation between proinflammatory cytokines and antiinflammatory mediators and the severity of disease in meningococcal infections. J Infect Dis 172:433–439
Riordan FA, Marzouk O, Thomson AP, Sills JA, Hart CA (1996) Proinflammatory and anti-inflammatory cytokines in meningococcal disease. Arch Dis Child 75:453–454
Van Zee KJ, Kohno T, Fischer E, Rock CS, Moldawer LL, Lowry SF (1992) Tumor necrosis factor soluble receptors circulate during experimental and clinical inflammation and can protect against excessive tumor necrosis factor alpha in vitro and in vivo. Proc Natl Acad Sci U S A 89:4845–4849
Deuren M van, van der Ven-Jongekrijg J, Demacker PN, Bartelink AK, van Dalen R, Sauerwein RW, Gallati H, Vannice JL, van der Meer JW (1994) Differential expression of proinflammatory cytokines and their inhibitors during the course of meningococcal infections. J Infect Dis 169:157–161
Dissel JT van, van Langevelde P, Westendorp RG, Kwappenberg K, Frolich M (1998) Anti-inflammatory cytokine profile and mortality in febrile patients. Lancet 351:950–953
Gogos CA, Drosou E, Bassaris HP, Skoutelis A (2000) Pro- versus anti-inflammatory cytokine profile in patients with severe sepsis: a marker for prognosis and future therapeutic options. J Infect Dis 181:176–180
Westerholt S, Pieper AK, Griebel M, Volk HD, Hartung T, Oberhoffer R (2003) Characterization of the cytokine immune response in children who have experienced an episode of typical hemolytic-uremic syndrome. Clin Diagn Lab Immunol 10:1090–1095
Thakur A, Xue M, Stapleton F, Lloyd AR, Wakefield D, Willcox MD (2002) Balance of pro- and anti-inflammatory cytokines correlates with outcome of acute experimental Pseudomonas aeruginosa keratitis. Infect Immun 70:2187–2197
Wamachi AN, Mayadev JS, Mungai PL, Magak PL, Ouma JH, Magambo JK, Muchiri EM, Koech DK, King CH, King CL (2004) Increased ratio of tumor necrosis factor-alpha to interleukin-10 production is associated with Schistosoma haematobium-induced urinary-tract morbidity. J Infect Dis 190:2020–2030
Thomson AP, Sills JA, Hart CA (1991) Validation of the Glasgow Meningococcal Septicemia Prognostic Score: a 10-year retrospective survey. Crit Care Med 19:26–30
Carcillo JA, Fields AI (2002) Clinical practice parameters for hemodynamic support of pediatric and neonatal patients in septic shock. Crit Care Med 30:1365–1378
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Halstensen A, Ceska M, Brandtzaeg P, Redl H, Naess A, Waage A (1993) Interleukin-8 in serum and cerebrospinal fluid from patients with meningococcal disease. J Infect Dis 167:471–475
Sfeir T, Saha DC, Astiz M, Rackow EC (2001) Role of interleukin-10 in monocyte hyporesponsiveness associated with septic shock. Crit Care Med 29:129–133
Fumeaux T, Pugin J (2002) Role of interleukin-10 in the intracellular sequestration of human leukocyte antigen-DR in monocytes during septic shock. Am J Respir Crit Care Med 166:1475–1482
Fumeaux T, Dufour J, Stern S, Pugin J (2004) Immune monitoring of patients with septic shock by measurement of intraleukocyte cytokines. Intensive Care Med 30:2028–2037
Carrol ED, Thomson AP, Mobbs KJ, Hart CA (2000) The role of RANTES in meningococcal disease. J Infect Dis 182:363–366
Moller AS, Bjerre A, Brusletto B, Joo GB, Brandtzaeg P, Kierulf P (2005) Chemokine patterns in meningococcal disease. J Infect Dis 191:768–775
Pathan N, Hemingway CA, Alizadeh AA, Stephens AC, Boldrick JC, Oragui EE, McCabe C, Welch SB, Whitney A, O’Gara P, Nadel S, Relman DA, Harding SE, Levin M (2004) Role of interleukin 6 in myocardial dysfunction of meningococcal septic shock. Lancet 363:203–209
Acknowledgements
We thank Dr. Jeremy Fellick, Institute of Child Health, Royal Liverpool Children’s Hospital NHS Trust, Alder Hey, for seeing some of the patients on admission, the nursing staff in the Accident and Emergency Department (Alder Hey) for their support with this study, and all the recruited children and their families. This work was supported by grants from the Johanne Holly Fund and Meningitis Merseyside. E.C. is currently funded by a Wellcome Trust Fellowship (grant no. GR068026MA).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carrol, E.D., Thomson, A.P.J., Jones, A.P. et al. A predominantly anti-inflammatory cytokine profile is associated with disease severity in meningococcal sepsis. Intensive Care Med 31, 1415–1419 (2005). https://doi.org/10.1007/s00134-005-2787-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2787-x