Abstract
Purpose
The aim of the present study was to describe histopathologic characteristics of synchronous bilateral breast cancer (SBBC), and by comparing SBBC to unilateral breast cancer (UBC), identify possible etiological mechanisms of SBBC.
Methods
Patients with primary SBBC (diagnosed within 4 months) and UBC diagnosed in Denmark between 1999 and 2015 were included. Detailed data on histopathology were retrieved from the Danish Breast Cancer Group database and the Danish Pathology Register. Associations between bilateral disease and the different histopathologic characteristics were evaluated by odds ratios and estimated by multinomial regression models.
Results
1214 patients with SBBC and 59,221 with UBC were included. Patients with SBBC more often had invasive lobular carcinomas (OR 1.29; 95% CI 1.13–1.47), a clinically distinct subtype of breast cancer, than UBC patients. Further, they were older than UBC patients, more often had multifocal cancer (OR 1.13; 95% CI 1.01–1.26), and a less aggressive subtype than UBC patients. Invasive lobular carcinoma was associated with having multiple tumors in breast tissue—both in the form of bilateral disease and multifocal disease, and this association was independent of laterality. No similar pattern was observed for other tumor characteristics.
Conclusion
We identified two etiological mechanisms that could explain some of the occurrence of SBBC. The high proportion of less aggressive carcinomas and higher age of SBBC compared to UBC patients suggests that many are diagnosed at a subclinical stage as slow-growing tumors have a higher probability of simultaneous diagnosis. The high proportion of invasive lobular carcinoma observed in bilateral and multifocal disease, being independent of laterality, suggests that these patients have an increased propensity to malignant tumor formation in breast tissue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The distribution of certain subtypes of breast carcinomas among synchronous bilateral breast cancer (SBBC) patients differs from that of unilateral breast cancer (UBC) patients. Although conflicting results have been published, the majority of studies have found that SBBC patients more often have invasive lobular carcinomas (ILC) [1,2,3,4,5,6,7] and estrogen receptor (ER)-positive carcinomas than UBC patients [2, 4, 7]. There are several possible explanations for the differences in tumor biology between SBBC and UBC. The time interval from a preclinical but screen detectable stage to a clinically detectable stage (the sojourn time) differs by tumor characteristics [8], and the probability of diagnosing a subclinical contralateral breast cancer should be larger the longer the time interval. SBBC patients could also have a higher propensity for tumor formation of certain subtypes either due to germline mutations, exposure profile (e.g., exposure to hormones and lifestyle risk factors), or both. Some studies have found that SBBC more often than UBC present with multifocal disease [9, 10], and in UBC patients multifocal disease is observed more often in ILCs [10,11,12,13], which could suggest that there is a link between multifocal breast cancer, bilateral breast cancer, and ILC. Our hypothesis was that the higher proportion of ILCs observed among SBBC and multifocal breast cancer patients reflect that breast cancer patients with ILC have a higher propensity to malignant tumor formation in breast parenchyma.
The aim of the present study was to describe histopathologic characteristics of SBBC compared to UBC, and to identify possible etiological mechanisms of SBBC.
Methods
Registries
Data were retrieved from the Danish Breast Cancer Group (DBCG) database [14] and the Danish Pathology Register [15]. The DBCG is a nationwide Danish breast cancer database with data on demographics, disease characteristics, treatment, and clinical follow-up for patients treated for primary invasive early breast cancer. The database has a high completeness (around 95% since the mid-nineties) [14]. The Danish Pathology Register is another nationwide Danish database, collecting data on tissue samples examined by all pathological departments in Denmark [15]. In the DBCG, patients with bilateral breast cancer are registered with bilateral disease, but subsequently excluded from further registration. Therefore, data on disease characteristics for SBBC patients were retrieved from the Danish Pathology Register. For UBC patients, all data were retrieved from the DBCG database.
Study population
All patients registered in the DBCG database, diagnosed with a primary invasive breast cancer from 1999 to 2015, were screened for inclusion. If patients were diagnosed with bilateral breast cancer within 4 months of each other, they were characterized as SBBC patients. Exclusion criteria were patients with only ductal carcinoma in situ (DCIS), previous malignancy, disseminated cancer, locally advanced cancer (e.g., tumor growth into the chest wall or ulcerated cancer), patients who received neoadjuvant therapy, patients not receiving surgical treatment, and age < 18 years.
Disease characteristics
The histological diagnoses were divided into three groups: invasive ductal carcinoma (IDC), ILC, and other carcinomas, the latter containing all other invasive breast carcinomas. Final histological diagnosis was based on the resection specimen. Malignancy grading of IDC and ILC was performed according to the latest updated WHO classification, dividing tumors into grade I, II, and III [16]. In the multivariable analyses, other carcinomas were treated as malignancy grade I. Tumor size and nodal involvement were categorized according to breast cancer staging [17]. Tumor size was divided into three categories: 1–20 mm, 21–50 mm, and > 50 mm, and nodal involvement into four groups: 0 lymph node metastases, 1–3 metastases, 4–9 metastases and > 9 metastases. ER status was visualized by immunohistochemical (IHC) staining, and from April 2010 and onwards, the tumor was regarded as ER positive if > 0% of the cancer cells were stained, and before April 2010 if ≥ 10% were stained. HER2 expression was visualized using IHC staining. If IHC examination was equivocal, in situ hybridization was performed, and a HER2/CEN17 ratio of ≥ 2.0 was interpreted as positive genetic amplification of HER2. HER2 analysis was only performed consistently nationwide from 2007 and onwards [18]. Therefore, HER2 is only reported after this date. The breast cancer was regarded as multifocal if the breast had more than one focus of invasive disease with normal tissue between the foci. No distinction was made between multifocality (more than one focus in the same quadrant of the breast) and multicentricity (foci in different quadrants of the breast). For UBC patients, only data on the index tumor were available for multifocal breast cancers, and whether the cancer was regarded as multifocal or not. For SBBC patients, number of foci was registered, and if number of foci was not specified (e.g., ‘several foci’), the cancer was categorized as ‘unspecified amount.’ Characteristics of each focus were registered whenever possible.
Statistical analysis
Differences in histopathologic characteristics between SBBC and UBC patients were evaluated by Odds Ratios (OR), estimated by multinomial regression analyses (equal to logistic regression when the outcome is binary), treating bilaterality as exposure and the disease characteristic of interest as outcome. Correlation between the right and left tumor in the same SBBC patient was accounted for using a Generalized Estimating Equation (GEE) correlation structure. Adjustments were performed based on a priori judged potential causality (e.g., tumor subtype would not be adjusted for tumor size, as the tumor size would not have an influence on the subtype, but tumor subtype would have an influence on size; see Supplement 1). Thus, the analysis of histology was adjusted for age, in the analysis of ER status or combined HER2/ER status for age and histology, in the analysis of tumor grade for age, histology, and ER status, in the analysis of multifocality for age, histology, ER status, and tumor grade, and so forth. Concordance in tumor characteristics between the right and left tumor in SBBC patients was investigated using simple Kappa values, reported with 95% confidence intervals. For tumor size and nodal involvement, weighted Kappa values were used.
In additional analyses, we investigated the OR of nodal involvement and of multifocality according to histology, ER status, and tumor grading in unilateral breast cancer patients. Adjustments were performed based on the judged relationship between tumor characteristics, performing one analysis adjusting only for judged confounders, and subsequently performing an analysis including judged mediators.
In bilateral patients, the tumor characteristics of the largest tumor were used and the OR of multifocal disease of the contralateral breast investigated, adjusting for multifocal disease of the largest tumor and histopathology of the contralateral tumor. This approach was used to investigate if certain tumor characteristics were associated with having multiple tumors but eliminating the effect of local spreading (satellite tumors).
To further evaluate to what degree histopathologic differences could be ascribed to a propensity to tumor formation, two additional analyses were performed for histology, ER status, and tumor grade. For brevity, these analyses were performed using logistic regression with dichotomized outcomes. In the first approach, histology, ER status, and tumor grade of the largest (index) tumor were treated as outcome, and the exposure was the number of tumors in the contralateral breast (0: UBC; 1: SBBC with unifocal contralateral disease; 2: SBBC patient with multifocal (≤ 2) contralateral disease; 3: SBBC with multifocal (> 2 foci) contralateral disease)—the exposure being a measure of propensity to tumor formation, rather than local spreading. Multifocal cancer with ‘unspecified amount’ of foci was included in the more than two foci group, as these would usually represent multiple foci where the pathologist had not specified the exact number of foci. In the second approach, still investigating the histology, ER status, and tumor grade of the largest tumor, patients were categorized based on whether both the cancer with the largest tumor, and the contralateral cancer were multifocal, thereby dividing UBC and SBBC patients into six groups (see Fig. 2b). Models were adjusted for age, whether the largest tumor was multifocal, and for bilateral patients, concordance in tumor characteristics (e.g., in the analysis of tumor histology, bilateral patients were also adjusted for histology of the contralateral tumor).
We performed two sensitivity analyses. In the first, it was examined whether multifocal disease in ILC could be explained primarily by a long sojourn time, increasing the probability of simultaneous diagnosis of multiple foci. The proportion of index tumors of low malignancy (ER positive, HER2 negative, grade I, and invasive ductal) according to number of tumor foci in the contralateral breast was investigated under the hypothesis that if no association was found among these low malignant and slow-growing tumors and multifocal disease, this would argue against ILC having a higher probability of multifocality merely because of a long sojourn time. In the second sensitivity analysis, it was investigated whether our results changed if multifocal tumors in SBBC patients were defined as IDC if just one focus was an IDC, which is the usual registration procedure in the DBCG database for UBC, instead of using the histology of the largest focus. See Supplement 2: sensitivity analyses.
Data were analyzed using SAS version 9.4 (SAS institute Inc., Cary, USA).
Results
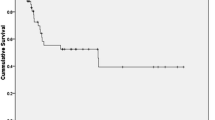
A total of 1214 patients with SBBC and 59,221 patients with UBC were included (see Fig. 1). The median age of SBBC and UBC patients was 67 years (IQR: 59–74) and 62 years (IQR: 53–70), respectively (p < 0.01), and hence 13.5% of SBBC patients were premenopausal, compared to 24.3% among UBC patients (p < 0.01).
For patient and disease characteristics see Table 1. In SBBC patients, there were no concordance to moderate concordance in histologic diagnosis (κ = 0.24; 95% CI 0.18 to 0.29), ER status (κ = 0.27; 95% CI 0.18 to 0.36), combined HER2 and ER status (κ = 0.11; 95% CI 0.03 to 0.19), malignancy grade (κ = 0.23; 95% CI 0.18 to 0.28), multifocality (κ = 0.07; 95% CI 0.01 to 0.13), nodal involvement (κ = 0.07; 95% CI 0.02 to 0.12), and tumor size (κ = 0.02; 95% CI − 0.03 to 0.08) between right and left tumors.
Table 2 shows the ORs of disease characteristics in SBBC patients compared with UBC patients. SBBC patients significantly more often had ILC, and more often cancer that was ER positive, HER2 negative, multifocal, and of lower malignancy grade. Patients with SBBC further had smaller tumors and less nodal involvement than UBC patients.
To investigate whether multifocal and bilateral breast cancer to some extent could represent the same underlying phenomenon, the association between multifocal and bilateral breast cancer and disease characteristics was investigated. In SBBC patients, the largest index tumor was more often an ILC if the contralateral breast had multifocal disease (OR = 1.84; 95% CI 1.27–2.68; see Table 3). Further, there was a statistically significant trend for an increasing OR of ILC with an increasing number of tumors in the contralateral breast (Fig. 2a). These associations were not attenuated when adjusting for age or multifocality of the index tumor, or when further adjusting for histology of the contralateral tumor. When stratifying patients on both bilaterality and multifocality, among SBBC patients, 14% of unifocal carcinomas (265/1953) vs. 19% (87/462) of multifocal cancers were ILC. Likewise, among UBC patients, 10% (4556/47,806) of unifocal vs. 17% of multifocal cancers were ILC (1778/10,582). When further stratifying SBBC patients on whether both the largest breast cancer and the contralateral breast cancer were multifocal, 40% (23/58) of the largest tumors were lobular if both breasts were multifocal, 21% (42/198) if the largest was multifocal, and 18% (26/148) if the contralateral was multifocal (Fig. 2b). In UBC patients, ILC was also associated with multifocal disease (OR = 1.92; 95% CI 1.80–2.03), but not with nodal involvement (OR = 0.99; 95% CI 0. 93 to 1.04; see Table 4). In the sensitivity analysis of the proportion of index tumors being grade I, invasive ductal, ER positive, and HER2 negative (proxy for slow-growing ‘luminal A’ cancer) according to number of tumors in the contralateral breast, we found no association between the two (see supplement 2).
Proportion of tumors being invasive lobular carcinomas according to multifocal and bilateral disease. a Proportion of the largest tumors being invasive lobular carcinomas according to number of tumors in the contralateral breast. Adj: adjusted for age and multifocal disease of the largest tumor; Adj2: Only patients with bilateral breast cancer. Adjusted for age, multifocal disease of the largest tumor, and histologic diagnosis of the contralateral tumor. b Proportion of the largest tumors being invasive lobular carcinomas according to whether the cancer in the breast with the largest tumor is multifocal and whether the contralateral breast cancer is multifocal. Adj: adjusted for age; Adj2: Only patients with bilateral breast cancer. Adjusted for age and histologic diagnosis of the contralateral tumor. 95% CI 95% confidence interval of the estimate, Adj adjustment, Adj2 adjustment 2, Unadj unadjusted
Among bilateral patients, being ER positive was not significantly associated with number of tumors in the contralateral breast (Supplement 3: Fig. 1a) or having multifocal disease in the contralateral breast (Table 3 and Supplement 3: Fig. 1b). Among unilateral patients, being ER positive was significantly associated with multifocal cancer (adj. OR = 1.14; 95% CI 1.07–1.21), with associations statistically similar to the associations observed in bilateral patients (see Tables 3 and 4). ER status was among UBC patients inversely associated with nodal involvement (OR = 0.89; 95% CI 0.85 to 0.93, Table 4).
Among bilateral patients, having a grade III carcinoma was not associated with number of tumors in the contralateral breast (Supplement 3: Fig. 2a). A trend for an inverse association between high malignancy grade and multifocal disease of the contralateral breast was however observed (Table 3). In unilateral patients, there was a positive association between malignancy grade and multifocal disease (grade II: OR = 1.30; 95% CI 1.24–1.38; grade III: OR = 1.42; 95% CI 1.33–1.52), and a positive association with nodal involvement (Table 4).
Tumor size and nodal involvement was highly dependent on mode of comparison (i.e., whether comparing both tumors or the largest tumor in the SBBC patient to the UBC patient). SBBC tumors were smaller and had fewer axillary metastases than UBC tumors when using both tumors in the bilateral patient for comparison. However, when comparing only the largest tumor, SBBC patients had larger tumors (54% vs 38% of tumors being > 20 mm) and more nodal involvement than UBC patients (53% vs. 44% with nodal involvement). Larger tumor size and more nodal involvement were also associated with multifocal cancer in both unilateral and bilateral breast cancer.
Discussion
In this nationwide cohort study, we found that patients with SBBC more often have ILC, and multifocal breast cancer, and more often have tumors that are ER positive, HER2 negative, and of malignancy grade I compared to patients with UBC. Further, the association between ILC and the presentation of multiple tumors—both in the form of bilateral and multifocal disease—was independent of laterality. No similar association was observed for other tumor characteristics.
Patients with SBBC have consistently been shown to have ILC more often than UBC patients [1,2,3,4,5,6,7]. Although UBC patients with ILC are slightly older than patients with IDC [19, 20], and SBBC patients older than UBC patients, the association was still observed when adjusting for age. ILC has a different growth pattern than IDC, infiltrating the surrounding breast tissue without destroying the anatomic structure, making it more difficult to diagnose clinically [21, 22]. The higher proportion of SBBC patients having ILC could thus potentially be explained by a longer sojourn time for ILC compared to IDC, increasing the likelihood of simultaneous diagnosis of bilateral cancer. Previous studies have shown that one of the most consistent risk factors for metachronous contralateral breast cancer is if the first cancer is an ILC [23], and in our sensitivity analysis, low-grade IDC was not associated with number of tumors in the contralateral breast. All these observations contradict ILC being more prevalent among bilateral and multifocal breast cancer patients merely because of slower growth.
Breast cancer presenting with multiple tumors was associated with ILC, and this association was observed irrespective of in which breast the tumors were diagnosed. Adjusting for both concordance of histology and multifocality between breasts did not change this association. The association between multifocal cancer and ILC could be explained by the loss of e-cadherin, resulting in loss of cell to cell adhesion, which facilitates tumor cell migration [22], but this does not explain the trend of increasing lobular histology with increasing multifocality of the contralateral breast. In a study examining the genetic predispositions for ILC and lobular carcinoma in situ, a distinct predisposition polymorphism was identified for ILC [24]. Further, they found that there were many overlapping predisposition polymorphisms between ILC and ER-positive IDC, but that some import differences suggest distinct etiological pathways between the subgroups [24]. Maybe the explanation for the propensity to multiple tumors observed in ILC can be found in the distinct etiological pathways for this carcinoma subtype.
Multifocal breast cancer can both occur due to local spreading with satellite metastases of a primary tumor, concurrent presentation of independent primary tumors, several invasive foci within a ‘bed’ of in situ carcinoma, after treatment with neoadjuvant chemotherapy, or due to irregular growth resulting in the misclassification of the carcinoma [25]. It has especially been debated whether multifocal breast cancer primarily represents local metastatic spread or multiple primary tumors [25]. In UBC patients with multifocal disease, up to 40% of patients have been reported to have tumor foci with discordant histopathology [26,27,28]. Studies analyzing the clonal origin of tumor foci in multifocal breast cancer have shown that in at least 50–75% of cases the different foci are genomic related, [29,30,31,32] arguing that the majority of multifocal breast cancers in UBC patients are derived from the same ancestral cancer cell and therefore represent intramammary metastatic spread of cancer or in situ carcinoma with several invasive foci [25, 30]. In a study by Norton et al. focusing on multifocal ILC, on the one hand, gene copy numbers were highly consistent between foci, suggesting foci were clonally related, but on the other hand, substantial within patient, between foci, genomic heterogeneity was observed [33].
SBBC patients were also found to be older than UBC patients and to have less aggressive tumor characteristics. In a study by Intra et al. SBBC tumors also had lower Ki-67 index and less often lymphovascular invasion [2]. All these findings underline that SBBC patients often have slow-growing and low-grade carcinomas [8]. It is likely that the contralateral cancer in a large proportion of SBBC patients is a consequence of the routine clinical examination, mammography, and ultrasound of both breasts in breast cancer patients, where the probability of finding a subclinical contralateral tumor increases the slower the subclinical tumor is growing. At screening mammography, the probability of simultaneous diagnosis would also increase the slower growing both tumors are. In a study by Hartman et al. on the incidence of bilateral breast cancer in Sweden, the authors argued that the incidence of SBBC was around 100 times higher than what could be explained by chance, and they therefore concluded that this could most likely be explained by accumulation of exposure to exogenous carcinogens [34]. In their calculation they did however not take into consideration that breast cancer patients routinely get a clinical examination and mammography of the contralateral breast at time of the diagnosis of the first cancer. As estimated sojourn times for breast cancer ranges from a little less than a year for the most aggressive cancers to more than 5 years for slow-growing tumors [8], the choice of a quarter of a year (their definition of SBBC) for the calculation of expected cancers due to chance would only be correct if just the breast giving clinical symptoms would be examined, and in a country without screening programs for breast cancer.
Although there was a tendency of a higher number of ER-positive tumors with multifocal disease, both among UBC and SBBC patients, the trend was not clear cut, and it was not statistically significant among bilateral patients. For malignancy grade, there was a tendency to an inverse association with multifocal disease among SBBC patients, but in UBC patients, malignancy grade II and III were positively associated with multifocal disease. Interestingly, in a study by Alexander et al. dividing multifocal disease based on whether foci were identical and without adjacent DCIS (indication for satellite metastasis), the multifocal cancers with identical foci and no DCIS were strongly associated with being grade III [35], and in a study by Brommesson et al. the multifocal cancers where foci were clustering—showing genomic similarities—were all grade III [31]. This could indicate that multifocal cancer in UBC patients to a higher degree represent local spreading than multifocal cancer in SBBC patients.
Limitations to this study primarily relates to the registration of histopathologic characteristics of tumors. Information on histopathology of SBBC and UBC was obtained from different sources, potentially introducing bias. As the registration practice of histology in multifocal UBC could vary in the DBCG database, although usually registering IDC if one focus is an IDC, we performed sensitivity analyses using different criteria for selecting histology in multifocal SBBC patients (see Supplement 2). These did not change the results. In a study by Kiaer et al. it was demonstrated that even among trained breast pathologists the interobserver variation in histological diagnosis was with a kappa value of 0.7 [36]. However, this potential misclassification is most likely not associated with laterality and therefore not a plausible explanation for the observed differences. This is one of the largest studies on the histopathologic characteristics of SBBC, including nationwide coverage and detailed histopathologic information from both cancers in the bilateral patient, giving us the opportunity to use the unique setting of patients with simultaneous cancers in a paired organ. However, we still had power issues in the analyses stratifying patients on both bilateral and multifocal status.
Conclusions
With the present study we have identified two patterns possibly reflecting two different etiological mechanisms for SBBC. The majority of SBBC tumors are low malignant tumors with ER-positive and HER2-negative status, and malignancy grade I in primarily older patients, reflecting carcinomas with slow growth that would increase the probability of simultaneous diagnosis. The other possible mechanism was identified in a subgroup of patients with ILC. Although it is well known that ILC is observed more often in multifocal and bilateral breast cancer [37], the findings of this study suggest that the association potentially reflects a propensity to tumor formation among these patients, as neither longer sojourn times nor a tendency to local spreading could seemingly explain the association.
Data availability
The data that support the findings of this study are archived at governmental institutions in Denmark and can be obtained through application to the relevant data agencies.
Abbreviations
- DCIS:
-
Ductal carcinoma in situ
- ER:
-
Estrogen receptor
- GEE:
-
Generalized estimating equations
- HER2:
-
Human epidermal growth factor receptor 2
- IDC:
-
Invasive ductal carcinoma
- ILC:
-
Invasive lobular carcinoma
- OR:
-
Odds ratio
- SBBC:
-
Synchronous bilateral breast cancer
- UBC:
-
Unilateral breast cancer
References
Verkooijen HM, Chatelain V, Fioretta G, Vlastos G, Rapiti E, Sappino AP, Bouchardy C, Chappuis PO (2007) Survival after bilateral breast cancer: results from a population-based study. Breast Cancer Res Treat 105(3):347–357. https://doi.org/10.1007/s10549-006-9455-x
Intra M, Rotmensz N, Viale G, Mariani L, Bonanni B, Mastropasqua MG, Galimberti V, Gennari R, Veronesi P, Colleoni M, Tousimis E, Galli A, Goldhirsch A, Veronesi U (2004) Clinicopathologic characteristics of 143 patients with synchronous bilateral invasive breast carcinomas treated in a single institution. Cancer 101(5):905–912. https://doi.org/10.1002/cncr.20452
Beckmann KR, Buckingham J, Craft P, Dahlstrom JE, Zhang Y, Roder D, Stuart-Harris R (2011) Clinical characteristics and outcomes of bilateral breast cancer in an Australian cohort. Breast 20(2):158–164. https://doi.org/10.1016/j.breast.2010.10.004
Matsuo K, Fukutomi T, Akashi-Tanaka S, Hasegawa T, Tsuda H (2002) Histological grade, p53, HER2 and hormone receptor status of synchronous bilateral breast carcinoma. Breast Cancer 9(2):127–133
Schmid SM, Pfefferkorn C, Myrick ME, Viehl CT, Obermann E, Schotzau A, Guth U (2011) Prognosis of early-stage synchronous bilateral invasive breast cancer. Eur J Surg Oncol 37(7):623–628. https://doi.org/10.1016/j.ejso.2011.05.006
Polednak AP (2003) Bilateral synchronous breast cancer: a population-based study of characteristics, method of detection, and survival. Surgery 133(4):383–389. https://doi.org/10.1067/msy.2003.110
Roder D, de Silva P, Zorbas H, Kollias J, Malycha P, Pyke C, Campbell I, Webster F (2012) Survival from synchronous bilateral breast cancer: the experience of surgeons participating in the breast audit of the society of breast surgeons of Australia and New Zealand. Asian Pac J Cancer Prev 13(4):1413–1418
Wu YY, Yen MF, Yu CP, Chen HH (2014) Risk assessment of multistate progression of breast tumor with state-dependent genetic and environmental covariates. Risk Anal 34(2):367–379. https://doi.org/10.1111/risa.12116
Newman LA, Sahin AA, Cunningham JE, Bondy ML, Mirza NQ, Vlastos GS, Whitman GJ, Brown H, Buchholz TA, Lee MH, Singletary SE (2001) A case-control study of unilateral and bilateral breast carcinoma patients. Cancer 91(10):1845–1853
Lesser ML, Rosen PP, Kinne DW (1982) Multicentricity and bilaterality in invasive breast carcinoma. Surgery 91(2):234–240
Kanumuri P, Hayse B, Killelea BK, Chagpar AB, Horowitz NR, Lannin DR (2015) Characteristics of multifocal and multicentric breast cancers. Ann Surg Oncol 22(8):2475–2482. https://doi.org/10.1245/s10434-015-4430-6
Yerushalmi R, Kennecke H, Woods R, Olivotto IA, Speers C, Gelmon KA (2009) Does multicentric/multifocal breast cancer differ from unifocal breast cancer? An analysis of survival and contralateral breast cancer incidence. Breast Cancer Res Treat 117(2):365–370. https://doi.org/10.1007/s10549-008-0265-1
Aalders KC, Kuijer A, Straver ME, Slaets L, Litiere S, Viale G, Van't Veer LJ, Glas AM, Delorenzi M, van Dalen T, Tryfonidis K, Piccart MJ, Cardoso F, Rutgers EJ, Consortium T, the MI (2017) Characterisation of multifocal breast cancer using the 70-gene signature in clinical low-risk patients enrolled in the EORTC 10041/BIG 03–04 MINDACT trial. Eur J Cancer 79:98–105. https://doi.org/10.1016/j.ejca.2017.03.034
Christiansen P, Ejlertsen B, Jensen MB, Mouridsen H (2016) Danish breast cancer cooperative group. Clin Epidemiol 8:445–449. https://doi.org/10.2147/CLEP.S99457
Bjerregaard B, Larsen OB (2011) The danish pathology register. Scand J Public Health 39(7 Suppl):72–74. https://doi.org/10.1177/1403494810393563
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19(5):403–410
Giuliano AE, Connolly JL, Edge SB, Mittendorf EA, Rugo HS, Solin LJ, Weaver DL, Winchester DJ, Hortobagyi GN (2017) Breast cancer-major changes in the American joint committee on cancer eighth edition cancer staging manual. CA Cancer J Clin 67(4): 290–303.
Rasmussen BB, Andersson M, Christensen IJ, Moller S (2008) Evaluation of and quality assurance in HER2 analysis in breast carcinomas from patients registered in Danish Breast Cancer Group (DBCG) in the period of 2002–2006. A nationwide study including correlation between HER-2 status and other prognostic variables. Acta Oncol 47(4):784–788. https://doi.org/10.1080/02841860801989779
Arpino G, Bardou VJ, Clark GM, Elledge RM (2004) Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res 6(3):R149–156. https://doi.org/10.1186/bcr767
Li CI, Uribe DJ, Daling JR (2005) Clinical characteristics of different histologic types of breast cancer. Br J Cancer 93(9):1046–1052. https://doi.org/10.1038/sj.bjc.6602787
Dedes KJ, Fink D (2008) Clinical presentation and surgical management of invasive lobular carcinoma of the breast. Breast Dis 30:31–37. https://doi.org/10.3233/BD-2009-0277
McCart Reed AE, Kutasovic JR, Lakhani SR, Simpson PT (2015) Invasive lobular carcinoma of the breast: morphology, biomarkers and 'omics. Breast Cancer Res 17:12. https://doi.org/10.1186/s13058-015-0519-x
Chen Y, Thompson W, Semenciw R, Mao Y (1999) Epidemiology of contralateral breast cancer. Cancer Epidemiol Biomarkers Prev 8(10):855–861
Sawyer E, Roylance R, Petridis C, Brook MN, Nowinski S, Papouli E, Fletcher O, Pinder S, Hanby A, Kohut K, Gorman P, Caneppele M, Peto J, Dos Santos SI, Johnson N, Swann R, Dwek M, Perkins KA, Gillett C, Houlston R, Ross G, De Ieso P, Southey MC, Hopper JL, Provenzano E, Apicella C, Wesseling J, Cornelissen S, Keeman R, Fasching PA, Jud SM, Ekici AB, Beckmann MW, Kerin MJ, Marme F, Schneeweiss A, Sohn C, Burwinkel B, Guenel P, Truong T, Laurent-Puig P, Kerbrat P, Bojesen SE, Nordestgaard BG, Nielsen SF, Flyger H, Milne RL, Perez JI, Menendez P, Benitez J, Brenner H, Dieffenbach AK, Arndt V, Stegmaier C, Meindl A, Lichtner P, Schmutzler RK, Lochmann M, Brauch H, Fischer HP, Ko YD, Network G, Nevanlinna H, Muranen TA, Aittomaki K, Blomqvist C, Bogdanova NV, Dork T, Lindblom A, Margolin S, Mannermaa A, Kataja V, Kosma VM, Hartikainen JM, Chenevix-Trench G, Investigators KC, Lambrechts D, Weltens C, Van Limbergen E, Hatse S, Chang-Claude J, Rudolph A, Seibold P, Flesch-Janys D, Radice P, Peterlongo P, Bonanni B, Volorio S, Giles GG, Severi G, Baglietto L, McLean CA, Haiman CA, Henderson BE, Schumacher F, Le Marchand L, Simard J, Goldberg MS, Labreche F, Dumont M, Kristensen V, Winqvist R, Pylkas K, Jukkola-Vuorinen A, Kauppila S, Andrulis IL, Knight JA, Glendon G, Mulligan AM, Devillee P, Tollenaar RA, Seynaeve CM, Kriege M, Figueroa J, Chanock SJ, Sherman ME, Hooning MJ, Hollestelle A, van den Ouweland AM, van Deurzen CH, Li J, Czene K, Humphreys K, Cox A, Cross SS, Reed MW, Shah M, Jakubowska A, Lubinski J, Jaworska-Bieniek K, Durda K, Swerdlow A, Ashworth A, Orr N, Schoemaker M, Couch FJ, Hallberg E, Gonzalez-Neira A, Pita G, Alonso MR, Tessier DC, Vincent D, Bacot F, Bolla MK, Wang Q, Dennis J, Michailidou K, Dunning AM, Hall P, Easton D, Pharoah P, Schmidt MK, Tomlinson I, Garcia-Closas M (2014) Genetic predisposition to in situ and invasive lobular carcinoma of the breast. PLoS Genet 10(4):e1004285. https://doi.org/10.1371/journal.pgen.1004285
Salgado R, Aftimos P, Sotiriou C, Desmedt C (2015) Evolving paradigms in multifocal breast cancer. Semin Cancer Biol 31:111–118. https://doi.org/10.1016/j.semcancer.2014.07.002
Buggi F, Folli S, Curcio A, Casadei-Giunchi D, Rocca A, Pietri E, Medri L, Serra L (2012) Multicentric/multifocal breast cancer with a single histotype: is the biological characterization of all individual foci justified? Ann Oncol 23(8):2042–2046. https://doi.org/10.1093/annonc/mdr570
Choi Y, Kim EJ, Seol H, Lee HE, Jang MJ, Kim SM, Kim JH, Kim SW, Choe G, Park SY (2012) The hormone receptor, human epidermal growth factor receptor 2, and molecular subtype status of individual tumor foci in multifocal/multicentric invasive ductal carcinoma of breast. Hum Pathol 43(1):48–55. https://doi.org/10.1016/j.humpath.2010.08.026
East EG, Pang JC, Kidwell KM, Jorns JM (2015) Utility of estrogen receptor, progesterone receptor, and HER-2/neu analysis of multiple foci in multifocal ipsilateral invasive breast carcinoma. Am J Clin Pathol 144(6):952–959. https://doi.org/10.1309/AJCPFWXP54OLILMU
Teixeira MR, Ribeiro FR, Torres L, Pandis N, Andersen JA, Lothe RA, Heim S (2004) Assessment of clonal relationships in ipsilateral and bilateral multiple breast carcinomas by comparative genomic hybridisation and hierarchical clustering analysis. Br J Cancer 91(4):775–782. https://doi.org/10.1038/sj.bjc.6602021
Desmedt C, Fumagalli D, Pietri E, Zoppoli G, Brown D, Nik-Zainal S, Gundem G, Rothe F, Majjaj S, Garuti A, Carminati E, Loi S, Van Brussel T, Boeckx B, Maetens M, Mudie L, Vincent D, Kheddoumi N, Serra L, Massa I, Ballestrero A, Amadori D, Salgado R, de Wind A, Lambrechts D, Piccart M, Larsimont D, Campbell PJ, Sotiriou C (2015) Uncovering the genomic heterogeneity of multifocal breast cancer. J Pathol 236(4):457–466. https://doi.org/10.1002/path.4540
Brommesson S, Jonsson G, Strand C, Grabau D, Malmstrom P, Ringner M, Ferno M, Hedenfalk I (2008) Tiling array-CGH for the assessment of genomic similarities among synchronous unilateral and bilateral invasive breast cancer tumor pairs. BMC Clin Pathol 8:6. https://doi.org/10.1186/1472-6890-8-6
Kim H, Kim CY, Park KH, Kim A (2018) Clonality analysis of multifocal ipsilateral breast carcinomas using X-chromosome inactivation patterns. Hum Pathol 78:106–114. https://doi.org/10.1016/j.humpath.2018.04.016
Norton N, Advani PP, Serie DJ, Geiger XJ, Necela BM, Axenfeld BC, Kachergus JM, Feathers RW, Carr JM, Crook JE, Moreno-Aspitia A, Anastasiadis PZ, Perez EA, Thompson EA (2016) Assessment of tumor heterogeneity, as evidenced by gene expression profiles, pathway activation, and gene copy number, in patients with multifocal invasive lobular breast tumors. PLoS ONE 11(4):e0153411. https://doi.org/10.1371/journal.pone.0153411
Hartman M, Czene K, Reilly M, Bergh J, Lagiou P, Trichopoulos D, Adami HO, Hall P (2005) Genetic implications of bilateral breast cancer: a population based cohort study. Lancet Oncol 6(6):377–382
Alexander M, Acosta Gonzalez G, Malerba S, Hochman T, Goldberg JD, Darvishian F (2017) Multifocal invasive ductal cancer: distinguishing independent tumor foci from multiple satellites. Int J Surg Pathol 25(4):298–303. https://doi.org/10.1177/1066896916676586
Kiaer H, Andersen JA, Rank F, Pedersen BV (1988) Quality control of patho-anatomical diagnosis of carcinoma of the breast. Acta Oncol 27(6A):745–747. https://doi.org/10.3109/02841868809091779
Christgen M, Steinemann D, Kuhnle E, Langer F, Gluz O, Harbeck N, Kreipe H (2016) Lobular breast cancer: clinical, molecular and morphological characteristics. Pathol Res Pract 212(7):583–597. https://doi.org/10.1016/j.prp.2016.05.002
Funding
This work was funded by a grant from the Danish Cancer Society (Grant Number: R124-A7440-15-S2).
Author information
Authors and Affiliations
Contributions
MKM, JW, MH, EB, ASK, AT, MM, and NK contributed to the conception and design of the study. Statistical analyses were performed by MKM and JW. First draft of the manuscript was written by MKM and JW, MH, EB, ASK, AT, MM, and NK revised the manuscript critically for scientific content.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to the present study.
Ethical approval
This study was approved by the Regional Research Ethics Committee of the Capital Region of Denmark (protocol number: H-16014553) and by the Regional Data Protection Agency (RH-2016-126).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mejdahl, M.K., Wohlfahrt, J., Holm, M. et al. Synchronous bilateral breast cancer: a nationwide study on histopathology and etiology. Breast Cancer Res Treat 182, 229–238 (2020). https://doi.org/10.1007/s10549-020-05689-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05689-0