Abstract
Background
Synchronous bilateral breast cancers (SBBCs) are rare and are defined as occurrence of tumor in the contralateral breast within 6 months of diagnosis of the primary breast tumor. The present study was conducted to look at the clinical and pathological profile and outcomes of patients with SBBC at our center.
Materials and Methods
All SBBC patients treated at our center between 2001 and 2015 were enrolled in the study. Data were retrospectively extracted from the patient case record.
Results
The study included 55 patients with SBBC with a median age of 52 years. Mammographically detected contralateral breast tumor constituted 7% of the cases. The maximum stage in either breast was stage II in 8/55 (15%) patients, stage III in 37/55 (67%) and stage IV in 10/55 (18%). Infiltrating ductal adenocarcinoma (IDC) was the most common pathology and was concordant in both the breasts in 53/55 (96%) patients. Concordance for estrogen receptor (ER), progesterone receptor (PR) and Her2 receptor was seen in 85, 89 and 92%, respectively. The 3-year event-free survival and overall survival for stages II, III and IV were 100, 61 and 0% (P < 0.001) and 100, 64.5 and 0% (P < 0.001), respectively.
Conclusion
SBBC patients at our center present in advanced stage. The maximum stage of either breast tumor determines the outcome. There is heterogeneity in the clinical features, pathological features and survival outcome of SBBC reported from India and rest of the world.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Synchronous bilateral breast cancer (SBBC) constitutes 1–2% of all breast cancer [1]. Various definitions have been used to define SBBC, the most widely accepted being the detection of a contralateral breast cancer within 6 months of diagnosis of primary breast cancer [2]. Breast cancer is the most common cancer among females in the various population-based cancer registries in India [3, 4]. However, there is a paucity of published literature on SBBC from India. The present study was conducted to analyze the clinical features, pathological features and outcome of patients with SBBC at our center.
Patients and Methods
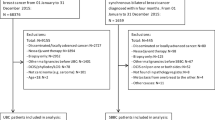
We retrospectively analyzed all consecutive SBBC patients who were treated at our center between 2001 and 2015. Patient details were obtained from the hospital records. Diagnosis of breast cancer was established with either core needle biopsy or fine-needle aspiration cytology (FNAC) of the primary breast tumor. Prognostic markers like estrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor type 2 (Her2) were analyzed on the biopsy specimen using immunohistochemistry (IHC). Patients were considered to be positive for Her2 if their IHC showed 3+ staining. Staging workup done for all patients included chest X-ray, ultrasound of abdomen and pelvis and bone scan. Additional imaging like computed tomography (CT) or magnetic resonance imaging (MRI) was done if there was suspicion of organ involvement by metastasis. Staging was done per the American Joint Committee of Cancer Staging (AJCC). Patients with stage I and II disease were classified as early breast cancer, stage III as locally advanced breast cancer (LABC) and stage IV as metastatic breast cancer. Treatment decisions for patients were taken by the hospital multi-disciplinary breast cancer tumor board. Planned treatment for patients with early breast cancer included modified radical mastectomy (MRM) or breast conservation surgery (BCS) followed by adjuvant chemotherapy, radiotherapy and hormonal therapy as indicated. Majority of the patients with LABC (stage III) were treated with 5-FU, epirubicin and cyclophosphamide (FEC-60) given concurrently with radiotherapy (CTRT) every 3 weekly followed by MRM and adjuvant hormone therapy in ER/PR-positive patients. CTRT with FEC-60 was incorporated during the first 2–3 cycles of FEC-60. The dose of radiation was 40 Gy given to bilateral breasts, axilla, supraclavicular and internal mammary nodal regions. Few patients with LABC received neoadjuvant chemotherapy (NACT) followed by surgery, adjuvant chemotherapy, radiotherapy and hormone therapy as indicated. Adjuvant radiation was delivered to a dose of 46 Gy to the chest wall, supraclavicular and internal mammary nodal regions. In the neoadjuvant setting, patients received six cycles FEC-90 chemotherapy, and in adjuvant setting, patients received three cycles FEC-90 and three cycles docetaxel chemotherapy. Patients with metastatic breast cancer received palliative endocrine therapy and/or chemotherapy and when required palliative radiotherapy. None of the patients received anti-Her2-directed therapy. There was heterogeneity in the treatment the patients received as they were enrolled over a period of 15 years. This analysis was done to observe the demographic, clinical presentation and stage and outcomes of patient with bilateral breast cancers. Patients with second primary in the breast diagnosed within 6 months of the primary breast cancer were taken as synchronous cancers, and those diagnosed with the second primary cancer more than 6 months from the primary breast cancer were taken as metachronous cancers. Staging for each breast was done independently; however, for survival analysis, the maximum stage of either breast was taken. Diagnosis, staging workup and treatment of the synchronous breast cancer were similar to the primary breast cancer.
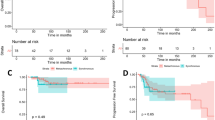
Event-free survival (EFS) was calculated from date of registration to date of relapse or progression or death. Overall survival (OS) was calculated from date of registration to date of death or last follow-up. All patients were censored for survival analysis at last follow-up or June 30, 2016, which ever was earlier. EFS and OS were estimated using Kaplan–Meier method, and variables were compared using the log-rank test. Statistical analysis was done using SPSS software (IBM SPSS Statistics version 16.0).
Results
SBBC was diagnosed in 55 of the 10,848 (0.5%) patients diagnosed to have breast cancer during the study period. The median age of the patients was 52 years (range; 21–74 years). All the patients were females, and 29/55 (53%) patients were postmenopausal. Family history of breast and ovarian cancer was present in only 4% of the patients. Only 4/55 (7%) patients had mammographically detected contralateral breast tumor; the rest of the patients were diagnosed by clinical examination. Patient demographic, clinical and pathological details have been provided in Table 1.
The maximum stage in either breast was stage II in 8/55 (15%) patients, stage III in 37/55 (67%) and stage IV in 10/55 (18%). Stage concordance was seen in 23 of 45 (51%) patients with non-metastatic disease. LABC (stage III) disease in both breasts was seen in 15/45 (37%) patients with non-metastatic disease. All the 10 patients with metastatic disease had bilateral locally advanced breast tumors (T3/T4 or N2). The sites of metastasis were bone in five patients, lung in four patients and liver and lung in one patient. The most common location for the tumor in both the breasts was the upper outer quadrant (right side 56% and left side 67%). Inner quadrant tumor was seen only in 9% of right breast and 16% of left breast tumor, and only 2/55 (3%) patients had tumor in the inner quadrant of both the breasts. Multi-centric tumor was seen in 8/55 (14%) patients, and 1/8 patient had bilateral multi-centric tumor. The second tumor in the contralateral breast was detected by mammography in 4/55 (7%) of patients.
Invasive ductal adenocarcinoma (IDC) was the most common pathology and was concordant in both the breasts in 53/55 (96%) patients. Among the patients with discordant pathology, one had IDC and neuroendocrine carcinoma and the other had poorly differentiated carcinoma and lobular carcinoma. Receptor testing in either breast tumor was not performed in 12 patients who were treated between 2000 and 2003 because of non-availability of IHC at our center during this period. Six patients had ER/PR testing in only one of the two breast tumor. Positivity for ER was seen in 14/37 (38%) right breast tumors and 18/41 (43%) left breast tumors; concordance for ER was seen in 31/35 (89%) patients who had testing in both breast tumors. Positivity for PR was seen in 19/36 (53%) right breast tumor and 21/40 (52%) left breast tumor; concordance for PR was seen in 29/34 (85%) patients. Her2 was 3+ in 10/28 (36%) right breast tumors and 12/31 (39%) left breast tumors; the concordance for Her2 in both breasts was seen in 24/26 (92%) patients who had testing in both breast tumors. Triple negative tumors (ER/PR and Her2 negative) were seen in either breast in 7/55 (13%) patients among whom five (9%) patients had triple negative tumors in both the breasts.
Among the 20 patients who received CTRT, 18 (90%) had a maximum stage of III, one patient had a maximum stage of II, and one patient had a maximum stage of IV. MRM was performed in 15/20 (75%) patients who received CTRT, and 5/20 (25%) patients (all maximum stage III) did not consent for MRM. These five patients were in complete remission at last follow-up; however, three of them have died due to non-breast cancer-related causes. Sixteen of 55 (29%) patients received NACT out of whom 10 underwent MRM followed by adjuvant treatment and six patients did not undergo MRM due to either disease progression or treatment abandonment. Upfront surgery was performed in 10 patients, among whom 7/10 underwent bilateral MRM and 2/10 underwent MRM on one side and breast conservation surgery (BCS) on the other side and 1/10 patient had bilateral BCS. Among the 10 patients who underwent upfront surgery, 7/10 had maximum stage II and 3/10 had maximum stage III. Palliative chemotherapy/endocrine treatment/radiotherapy was offered to nine patients who had metastatic disease at presentation and one patient received CTRT (had solitary pulmonary metastasis) as mentioned earlier.
There were 24 events in the study patients, 9/24 (38%) due to relapse (local relapse n = 4, distant relapse n = 4 and combined n = 1), 7/24 (29%) due to disease progression in patients with metastatic disease and 8/24 (33%) deaths unrelated to breast cancer. Twenty-one of 55 patients (38%) had died at last follow-up, and breast cancer was the cause of death in 13/21 (62%) patients. The mean and median duration of follow-up in the study was 41.5 months and 19.6 months, respectively (range 0.8–174.23 months). The median duration of time to event was 15.52 months, and majority of the patients died within few months of an event. The 3-year EFS and OS (Fig. 1) for all stages were 51.8% and 55.4%, respectively. The 3-year EFS for stages II, III and IV was 100, 61 and 0%, respectively (P < 0.001). The 3-year OS for stages II, III and IV was, respectively, 100, 64.5 and 0% (P < 0.001), respectively (Fig. 2).
Discussion
SBBC accounts for 1–2% of all breast cancers and is less commonly seen than metachronous breast cancer [1]. There are reports in the literature that suggest SBBC may be associated with increased frequency of lobular carcinoma; however, in contrast in our study IDC was seen in 96% of the patients and is similar to other reports from India (Table 2) [5,6,7,8,9]. The median age of our study patients was 52 years which is similar to what has been reported in unilateral breast cancer from India, and majority were postmenopausal [3, 4]. There are conflicting reports in the literature on the age of presentation of SBBC in comparison with unilateral breast cancer with some studies suggesting that they occur in younger patients and other studies suggesting that they occur in elderly population [1]. Only 7% of second breast tumor in our study were mammographically detected in contrast to 40–43% reported from other centers in India [7, 8].
Fifty percent of unilateral breast cancer patients in India present in advanced stage, and this was also seen in our study where 67% of patients had a maximum stage III disease [3, 4]. Studies have shown that the ER/PR positivity in unilateral breast cancer from India ranges from 35 to 45% and is lesser than what is reported from West [9, 10]. The positivity for ER in our study was 37% in right breast and 43% in left breast tumors; this is similar to what has been seen in unilateral tumors in India. Positivity for Her2 in either of the breast was seen in 36% right breast and 39% left breast tumors; this is higher than what has been reported for unilateral breast cancer from India but similar to reports on increased Her2 expression in SBBC [11, 12].
Compared to metachronous breast cancer, SBBC has higher concordance for ER and Her2neu receptors [13]. Concordance for ER and Her2 receptor was 89 and 92%, respectively, in our study. It has been proven by molecular studies that SBBC arises from different clones even though they have high concordance for pathology and receptor status [14, 15].
According to the literature, patients with bilateral breast cancer with metastatic disease are not included as SBBC. However, we included patients with metastatic disease as we noticed that majority of patient with SBBC at our center presented with advanced disease and by clinical examination and routine pathology it is not possible to rule out entirely if the second breast tumor is metastatic or de novo in nature. Even though we analyzed patients over a 15-year period, our median follow-up was only 19.6 months, and this was because majority of the events occurred within the first 16 months of starting treatment.
CTRT is not routinely practiced as a standard of care for treatment of breast cancer. However, at our center, CTRT is preferred for patients with inoperable LABC and it has been shown to be an effective modality of treatment [16].
There are conflicting reports on the survival outcomes of patients with SBBC in comparison with patients with unilateral breast cancer, with some studies showing no difference in outcome and others showing inferior outcome [1, 2, 17,18,19,20,21]. The stagewise EFS and OS in our study are similar to what has been reported in Indian literature for unilateral breast cancer [3, 4, 9]. One-third of the study patients died due to non-breast cancer-related causes like old age and cardiovascular diseases.
Our study has limitations which include its retrospective nature, non-availability of receptor status in many patients and heterogeneous treatment.
Conclusion
SBBCs are rare but have prognosis similar to unilateral breast cancer. The highest stage influences the outcome. SBBC in India differs from West with regard to clinical presentation and pathology.
References
Londero AP, Bernardi S, Bertozzi S, Angione V, Gentile G, Dri C, et al. Synchronous and metachronous breast malignancies: a cross-sectional retrospective study and review of the literature. Biomed Res Int. 2014;2014:250727.
Hartman M, Czene K, Reilly M, Adolfsson J, Bergh J, Adami HO, et al. Incidence and prognosis of synchronous and metachronous bilateral breast cancer. J Clin Oncol. 2007;25:4210–6.
Sathwara J, Bobdey S, Ganesh B. Breast cancer survival studies in India: a review. Int J Res Med Sci. 2016;4:3102–8.
Agarwal G, Ramakant P. Breast cancer care in India: the current scenario and the challenges for the future. Breast Care (Basel). 2008;3:21–7.
Chen JJ, Wang Y, Xue JY, Chen Y, Chen YL, Xiao Q, et al. A clinicopathological study of early-stage synchronous bilateral breast cancer: a retrospective evaluation and prospective validation of potential risk factors. PLoS ONE. 2014;9:e95185.
Selvakumar VP, Garg S, Siddiqui K, Goel A, Kumar K, Kumar R. Tailored approach to management of bilateral breast cancer in Indian women. Asian J Oncol. 2015;1:97–100.
Krishnappa R, Chikaraddi SB, Deshmane V. Primary synchronous bilateral breast cancer. Indian J Cancer. 2014;51:256–8.
Padmanabhan N, Subramanyan A, Radhakrishna S. Synchronous bilateral breast cancers. J Clin Diagn Res. 2015;9:XC05–8.
Gogia A, Raina V, Deo SV, Shukla NK, Mohanti BK, Sharma DN. Taxane and anthracycline based neoadjuvant chemotherapy for locally advanced breast cancer: institutional experience. Asian Pac J Cancer Prev. 2014;15:1989–92.
Patnayak R, Jena A, Rukmangadha N, Chowhan AK, Sambasivaiah K, Phaneendra BV, et al. Hormone receptor status (estrogen receptor, progesterone receptor), human epidermal growth factor-2 and p53 in South Indian breast cancer patients: a tertiary care center experience. Indian J Med Paediatr Oncol. 2015;36:117–22.
Doval DC, Sharma A, Sinha R, Kumar K, Dewan AK, Chaturvedi H, et al. Immunohistochemical profile of breast cancer patients at a tertiary care hospital in New Delhi, India. Asian Pac J Cancer Prev. 2015;16:4959–64.
Safal M, Lower EE, Hasselgren PO, Hungness ES, Gazder P, Aron B, et al. Bilateral synchronous breast cancer and HER-2/neu overexpression. Breast Cancer Res Treat. 2002;72:195–201.
Gong SJ, Rha SY, Jeung HC, Roh JK, Yang WI, Chung HC. Bilateral breast cancer: differential diagnosis using histological and biological parameters. Jpn J Clin Oncol. 2007;37:487–92.
Saad RS, Denning KL, Finkelstein SD, Liu Y, Pereira TC, Lin X, et al. Diagnostic and prognostic utility of molecular markers in synchronous bilateral breast carcinoma. Mod Pathol. 2008;21:1200–7.
Imyanitov EN, Hanson KP. Molecular pathogenesis of bilateral breast cancer. Cancer Lett. 2003;191:1–7.
Shanta V, Swaminathan R, Rama R, Radhika R. Retrospective analysis of locally advanced noninflammatory breast cancer from Chennai, South India, 1990–1999. Int J Radiat Oncol Biol Phys. 2008;70:51–8.
Vuoto HD, García AM, Candás GB, Zimmermann AG, Uriburu JL, Isetta JA, et al. Bilateral breast carcinoma: clinical characteristics and its impact on survival. Breast J. 2010;16:625–32.
Kheirelseid EA, Jumustafa H, Miller N, Curran C, Sweeney K, Malone C, et al. Bilateral breast cancer: analysis of incidence, outcome, survival and disease characteristics. Breast Cancer Res Treat. 2011;126:131–40.
Schmid SM, Pfefferkorn C, Myrick ME, Viehl CT, Obermann E, Schötzau A, et al. Prognosis of early-stage synchronous bilateral invasive breast cancer. Eur J Surg Oncol. 2011;37:623–8.
Carmichael AR, Bendall S, Lockerbie L, Prescott R, Bates T. The long-term outcome of synchronous bilateral breast cancer is worse than metachronous or unilateral tumours. Eur J Surg Oncol. 2002;28:388–91.
Beckmann KR, Buckingham J, Craft P, Dahlstrom JE, Zhang Y, Roder D, et al. Clinical characteristics and outcomes of bilateral breast cancer in an Australian cohort. Breast. 2011;20:158–64.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The study had no source of funding.
Conflict of interest
None of the authors have any conflict of interest.
Ethical Approval
The study is retrospective in nature. For this type of study, formal consent and ethical approval are not required. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
The study is retrospective in nature and does not require informed consent of individual participants included in the study.
Rights and permissions
About this article
Cite this article
Iyer, P., Radhakrishnan, V., Ananthi, B. et al. Synchronous Bilateral Breast Cancer: Clinical Features, Pathology and Survival Outcomes from a Tertiary Cancer Center. Indian J Gynecol Oncolog 15, 35 (2017). https://doi.org/10.1007/s40944-017-0128-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40944-017-0128-y